Sunday Poster Session
Category: Colorectal Cancer Prevention
P0464 - Cumulative Incidence and Predictors of Advanced Neoplasia in Elderly Patients With Lynch Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Anthony Kerbage, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Award: ACG Presidential Poster Award
Anthony Kerbage, MD1, Sara Haddad, MD2, Natalie Farha, MD3, James Bena, MS2, Shannon Morrisson, MS2, Carole Macaron, MD2, David Liska, MD, MA2, Joshua Sommovilla, MD2, Carol A.. Burke, MD, MACG2
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Cleveland Clinic, Wichita, KS
Introduction: United States guidelines recommend colonoscopy surveillance starting age 25-35 in Lynch Syndrome (LS) with no set age to stop. Risk of both advanced neoplasia (AN) and endoscopic complications rise with age. The risk-benefit of surveillance colonoscopy in elderly LS patients is unknown. We assessed the incidence of and predictors for AN and endoscopic complications in LS patients ≥ 75 yrs of age undergoing surveillance lower endoscopy.
Methods: LS patients with ≥ 1 lower endoscopy at age ≥ 75 years were reviewed in the electronic medical record. The incidence of AN (tubular adenoma ≥10 mm, or with villous features, or high-grade dysplasia; hyperplastic polyp ≥10 mm; sessile serrated polyp ≥10 mm or with or without dysplasia; traditional serrated adenoma; or adenocarcinoma) on lower endoscopy ≥75 years of age, pre- and post-age 75 clinical and endoscopic predictors of AN, and pre-, intra- and post procedural lower endoscopic complications were reviewed. Kaplan-Meier estimated the cumulative incidence of AN. Predictors of AN were evaluated by univariable time-to-event analyses using Cox proportional hazards models. Endoscopic complications were described.
Results: 58 eligible LS patients were included, with an average age-adjusted Charlson Comorbidity Index of 5.1 ± 2.1. 172 lower endoscopies were performed over a median follow-up of 26 months [IQR 6, 48] from first to last lower endoscopy ≥ 75 years of age (Table 1). AN occurred in 28% (16/58) including CRC in 12% (7/58). Mean age at first AN and CRC ≥ 75 yrs was 78.4 and 80.6 yrs, respectively. The cumulative incidence of AN reached 40.5% by year 7. Predictors of AN ≥ 75 yrs included a history of AN < 75 yrs (HR 4.23, 95% CI 1.46–12.22), older age at first colonoscopy ≥ age 75 (HR 1.25 per year), greater number of colonoscopies ≥ age 75 (HR 1.24 per procedure, p=0.027), and absence of aspirin use (p=0.009). One complication, intraprocedural hypotension, occurred (0.6% of procedures).
Discussion: In this small, healthy cohort of elderly LS patients, the risk of AN is substantial after age 75, particularly in patients with a history of AN. Aspirin seemed to have a protective role. Endoscopic complications were mild and rare. These findings support continuing lower endoscopic surveillance in LS patients ≥ age 75 using the risk factors that we identified to help guide informed discussions about the risks and benefits. Larger studies are needed to confirm our findings and inform future LS guidelines.
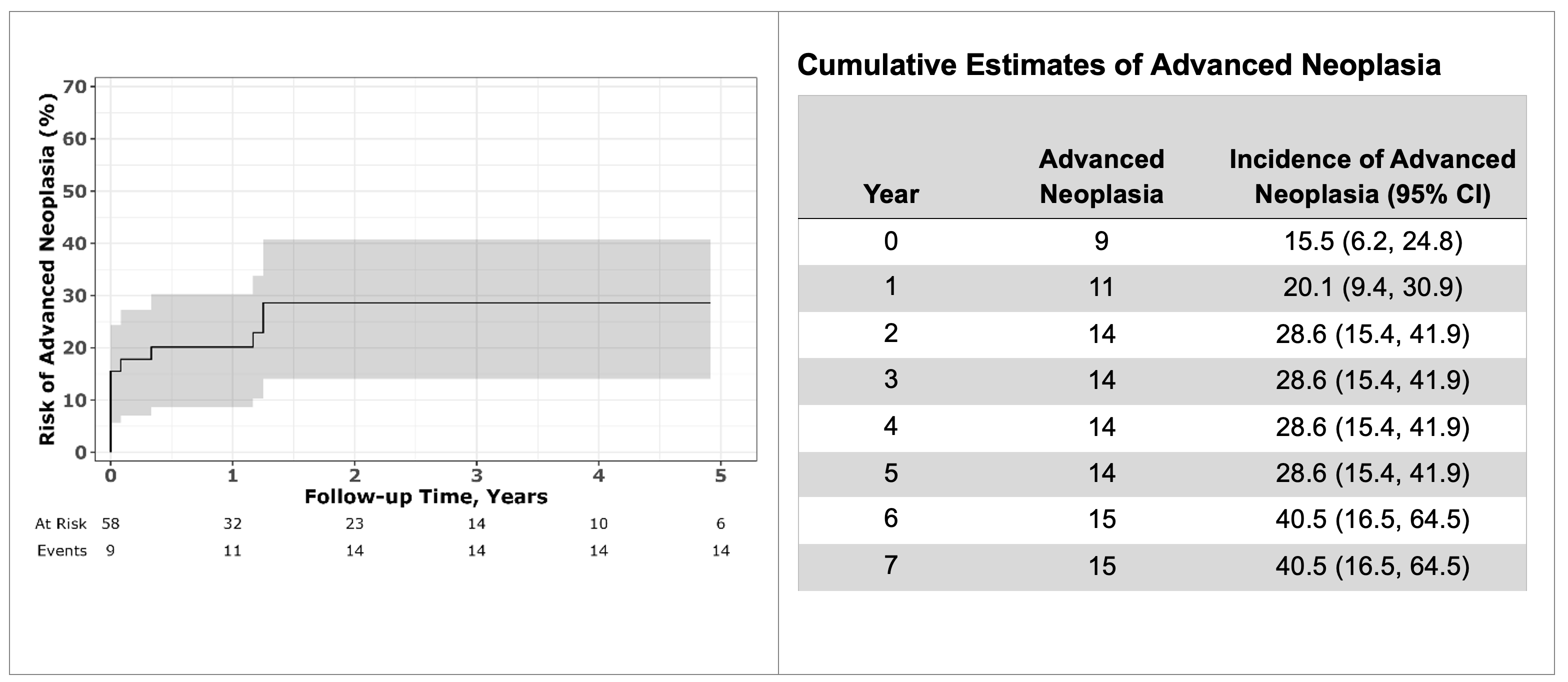
Figure: Figure 1. Incidence of Advanced Neoplasia Over Time on Colonoscopies done after age 75
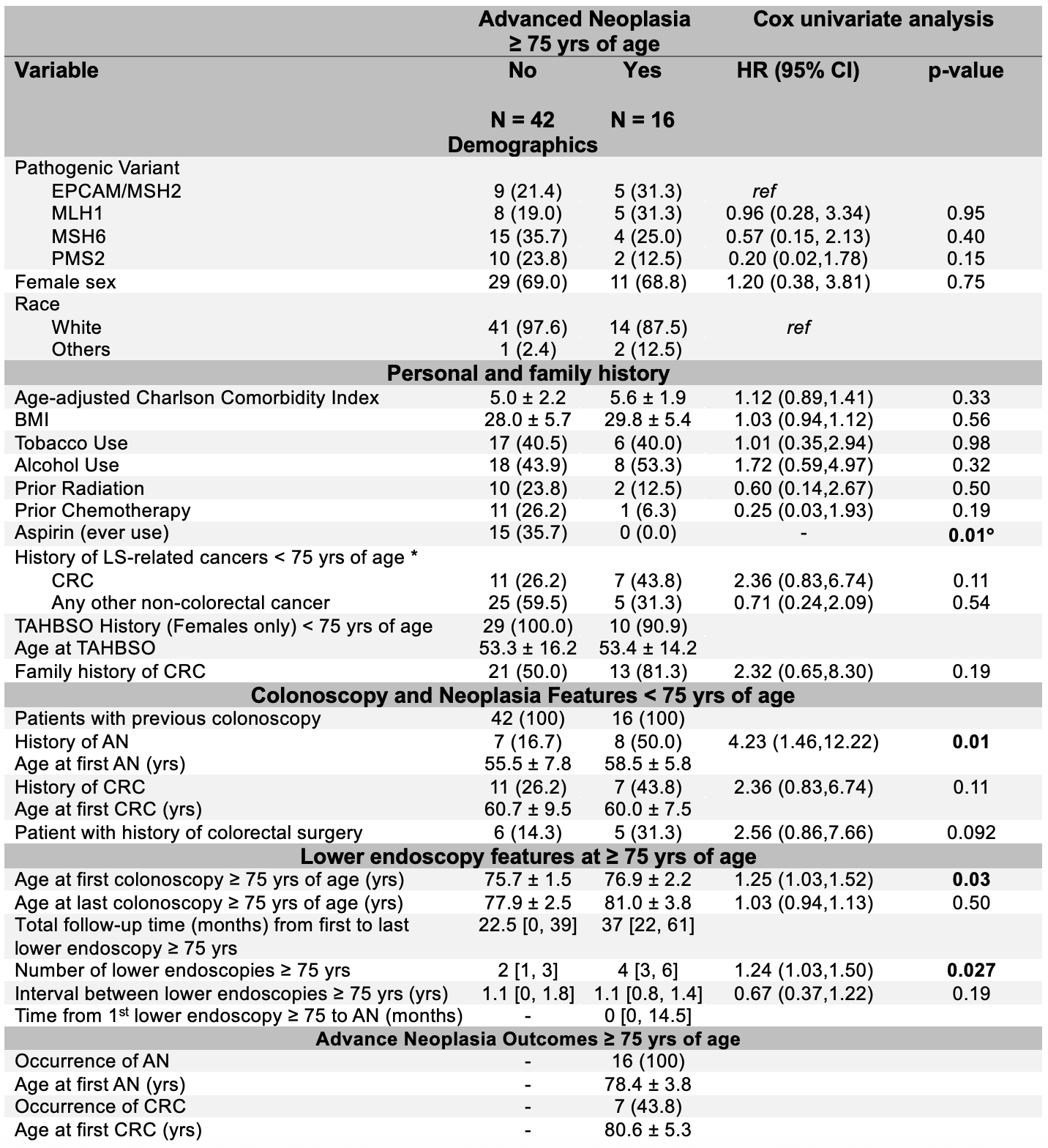
Figure: Table 1. Predictors of advanced neoplasia in Lynch syndrome on lower endoscopy done at age ≥ 75 yrs
TAHBSO (Total Abdominal Hysterectomy with Bilateral Salpingo-Oophorectomy), BMI (Body Mass Index), LS (Lynch Syndrome), AN (Advanced Neoplasia), CRC (Colorectal Cancer), SSA/SSP (Sessile Serrated Adenoma/Sessile Serrated Polyp), TSA (Traditional Serrated Adenoma).
Log-rank test
* Other cancers included: Endometrial, gastric, urothelial, cholangiocarcinoma, gallbladder, ampullary, brain, small intestinal and keratoacanthomas.
* All surgeries were limited resections (including right hemicolectomy, low anterior resection, sigmoid colectomy, right hemicolectomy with low anterior resection, left hemicolectomy, partial colectomy (unspecified location), proctosigmoidectomy, and proctocolectomy.
Disclosures:
Anthony Kerbage indicated no relevant financial relationships.
Sara Haddad indicated no relevant financial relationships.
Natalie Farha indicated no relevant financial relationships.
James Bena indicated no relevant financial relationships.
Shannon Morrisson indicated no relevant financial relationships.
Carole Macaron indicated no relevant financial relationships.
David Liska indicated no relevant financial relationships.
Joshua Sommovilla indicated no relevant financial relationships.
Carol Burke: emtora biosciences – Grant/Research Support. lumabridge – Consultant. myriad – Food and beverage. Natera – Food and beverage.
Anthony Kerbage, MD1, Sara Haddad, MD2, Natalie Farha, MD3, James Bena, MS2, Shannon Morrisson, MS2, Carole Macaron, MD2, David Liska, MD, MA2, Joshua Sommovilla, MD2, Carol A.. Burke, MD, MACG2. P0464 - Cumulative Incidence and Predictors of Advanced Neoplasia in Elderly Patients With Lynch Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Anthony Kerbage, MD1, Sara Haddad, MD2, Natalie Farha, MD3, James Bena, MS2, Shannon Morrisson, MS2, Carole Macaron, MD2, David Liska, MD, MA2, Joshua Sommovilla, MD2, Carol A.. Burke, MD, MACG2
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Cleveland Clinic, Wichita, KS
Introduction: United States guidelines recommend colonoscopy surveillance starting age 25-35 in Lynch Syndrome (LS) with no set age to stop. Risk of both advanced neoplasia (AN) and endoscopic complications rise with age. The risk-benefit of surveillance colonoscopy in elderly LS patients is unknown. We assessed the incidence of and predictors for AN and endoscopic complications in LS patients ≥ 75 yrs of age undergoing surveillance lower endoscopy.
Methods: LS patients with ≥ 1 lower endoscopy at age ≥ 75 years were reviewed in the electronic medical record. The incidence of AN (tubular adenoma ≥10 mm, or with villous features, or high-grade dysplasia; hyperplastic polyp ≥10 mm; sessile serrated polyp ≥10 mm or with or without dysplasia; traditional serrated adenoma; or adenocarcinoma) on lower endoscopy ≥75 years of age, pre- and post-age 75 clinical and endoscopic predictors of AN, and pre-, intra- and post procedural lower endoscopic complications were reviewed. Kaplan-Meier estimated the cumulative incidence of AN. Predictors of AN were evaluated by univariable time-to-event analyses using Cox proportional hazards models. Endoscopic complications were described.
Results: 58 eligible LS patients were included, with an average age-adjusted Charlson Comorbidity Index of 5.1 ± 2.1. 172 lower endoscopies were performed over a median follow-up of 26 months [IQR 6, 48] from first to last lower endoscopy ≥ 75 years of age (Table 1). AN occurred in 28% (16/58) including CRC in 12% (7/58). Mean age at first AN and CRC ≥ 75 yrs was 78.4 and 80.6 yrs, respectively. The cumulative incidence of AN reached 40.5% by year 7. Predictors of AN ≥ 75 yrs included a history of AN < 75 yrs (HR 4.23, 95% CI 1.46–12.22), older age at first colonoscopy ≥ age 75 (HR 1.25 per year), greater number of colonoscopies ≥ age 75 (HR 1.24 per procedure, p=0.027), and absence of aspirin use (p=0.009). One complication, intraprocedural hypotension, occurred (0.6% of procedures).
Discussion: In this small, healthy cohort of elderly LS patients, the risk of AN is substantial after age 75, particularly in patients with a history of AN. Aspirin seemed to have a protective role. Endoscopic complications were mild and rare. These findings support continuing lower endoscopic surveillance in LS patients ≥ age 75 using the risk factors that we identified to help guide informed discussions about the risks and benefits. Larger studies are needed to confirm our findings and inform future LS guidelines.
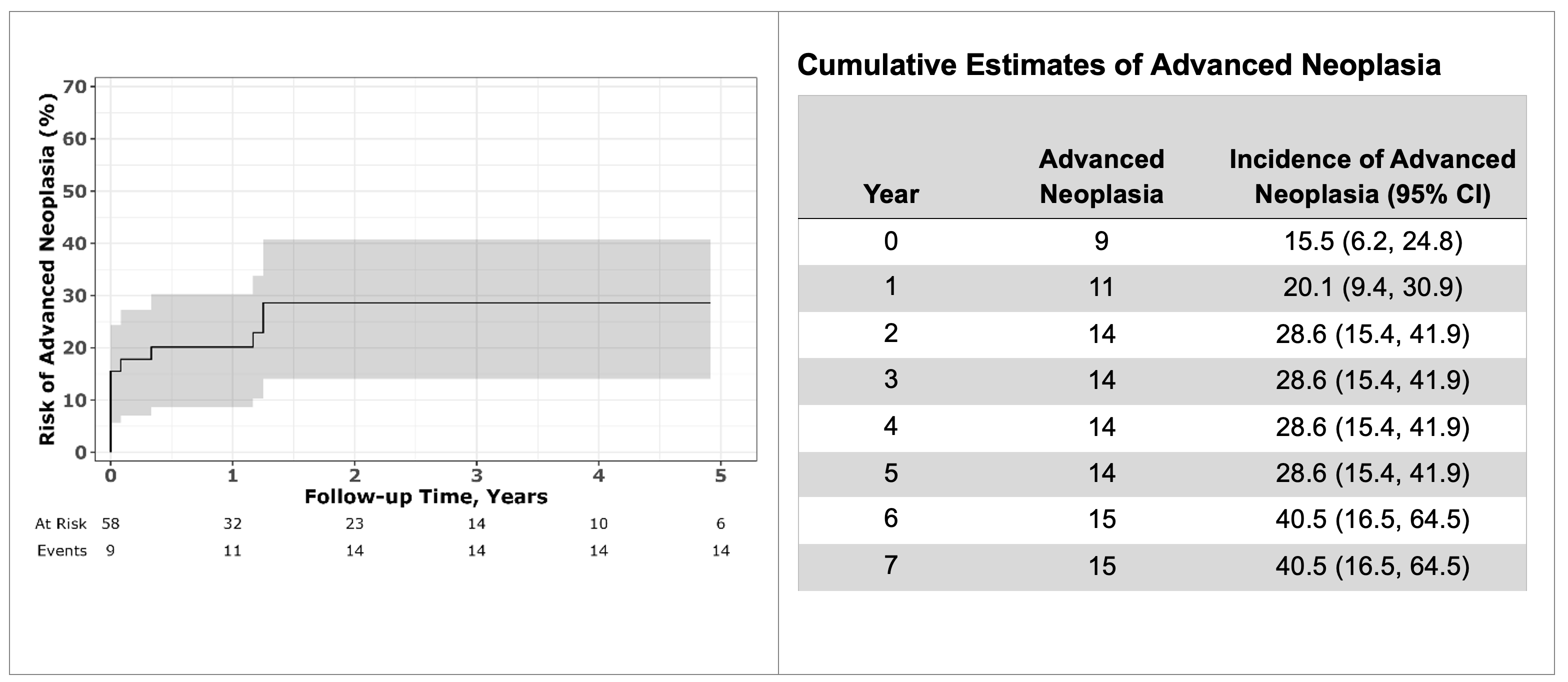
Figure: Figure 1. Incidence of Advanced Neoplasia Over Time on Colonoscopies done after age 75
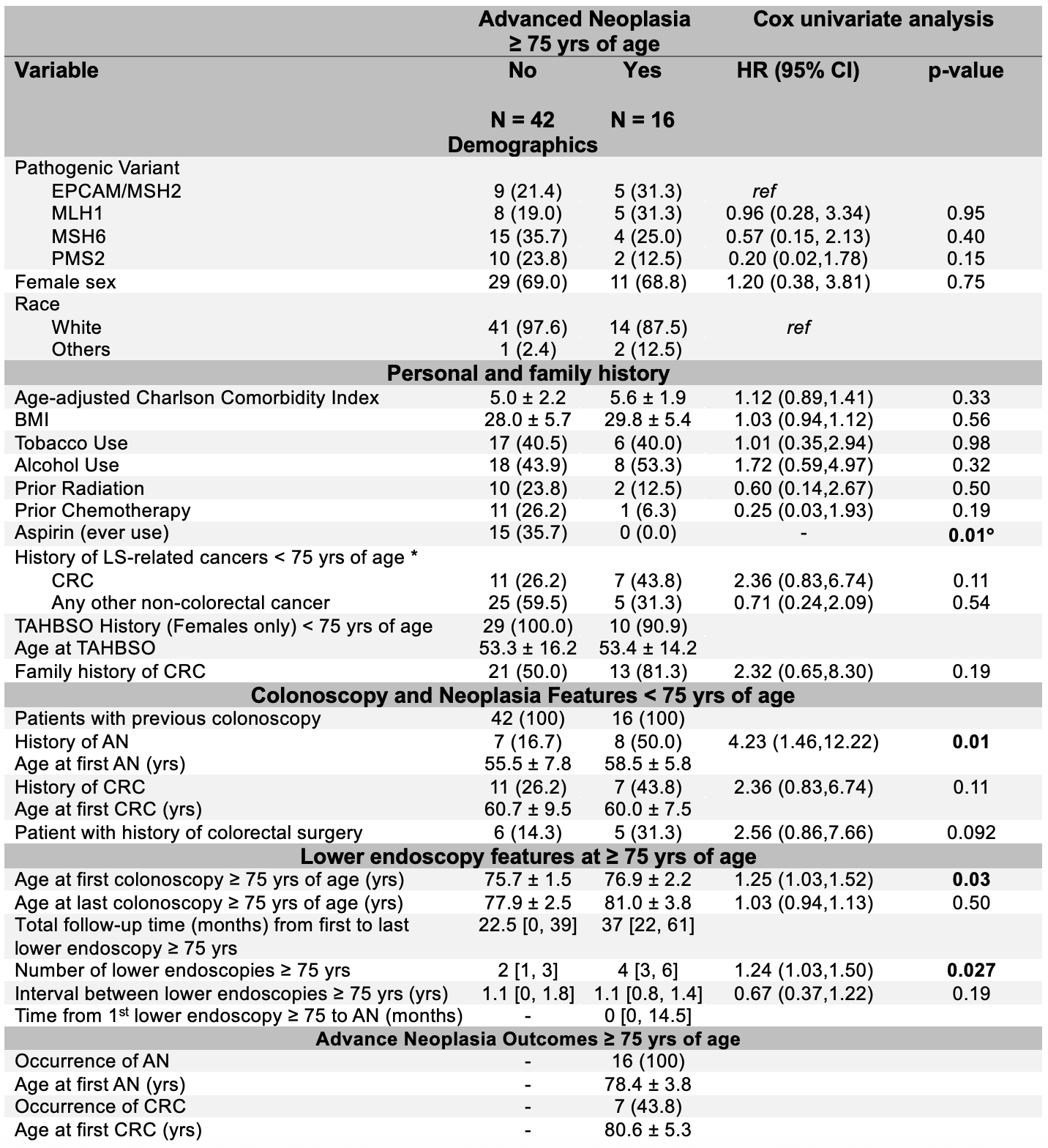
Figure: Table 1. Predictors of advanced neoplasia in Lynch syndrome on lower endoscopy done at age ≥ 75 yrs
TAHBSO (Total Abdominal Hysterectomy with Bilateral Salpingo-Oophorectomy), BMI (Body Mass Index), LS (Lynch Syndrome), AN (Advanced Neoplasia), CRC (Colorectal Cancer), SSA/SSP (Sessile Serrated Adenoma/Sessile Serrated Polyp), TSA (Traditional Serrated Adenoma).
Log-rank test
* Other cancers included: Endometrial, gastric, urothelial, cholangiocarcinoma, gallbladder, ampullary, brain, small intestinal and keratoacanthomas.
* All surgeries were limited resections (including right hemicolectomy, low anterior resection, sigmoid colectomy, right hemicolectomy with low anterior resection, left hemicolectomy, partial colectomy (unspecified location), proctosigmoidectomy, and proctocolectomy.
Disclosures:
Anthony Kerbage indicated no relevant financial relationships.
Sara Haddad indicated no relevant financial relationships.
Natalie Farha indicated no relevant financial relationships.
James Bena indicated no relevant financial relationships.
Shannon Morrisson indicated no relevant financial relationships.
Carole Macaron indicated no relevant financial relationships.
David Liska indicated no relevant financial relationships.
Joshua Sommovilla indicated no relevant financial relationships.
Carol Burke: emtora biosciences – Grant/Research Support. lumabridge – Consultant. myriad – Food and beverage. Natera – Food and beverage.
Anthony Kerbage, MD1, Sara Haddad, MD2, Natalie Farha, MD3, James Bena, MS2, Shannon Morrisson, MS2, Carole Macaron, MD2, David Liska, MD, MA2, Joshua Sommovilla, MD2, Carol A.. Burke, MD, MACG2. P0464 - Cumulative Incidence and Predictors of Advanced Neoplasia in Elderly Patients With Lynch Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

