Sunday Poster Session
Category: Colon
P0412 - A Case of Atypical Hemolytic Uremic Syndrome Mimicking IBD

Rebhi Rabah, MD (he/him/his)
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Garnet Health Medical Center, Brooklyn, NY; 3NYC Health + Hospitals/Kings County, Brooklyn, NY
Introduction:
Hemolytic uremic syndrome (HUS) is a triad composed of microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure. Atypical HUS (AHUS) is characterized by complement overactivation. Triggers include upper respiratory infection, fever, pregnancy, drugs, and non-E. Coli diarrheal illness. AHUS causes microvascular injury and loss of GI mucosal integrity causing inflammatory changes like that of Inflammatory Bowel Disease (IBD). We present a case of a 27-year-old male with AHUS mimicking IBD treated successfully with eculizumab.
Case Description/
Methods:
A 27 year old male with history of lead exposure presented to the hospital with complaints of progressive fatigue and intermittent loose, bloody bowel movements for 2 months. In the ED, vitals were significant for heart rate of 120 beats per minute. Patient was anemic with hemoglobin of 2.9 g/dL, leukocytosis of 52.66 k/uL and mild thrombocytopenia of 100 k/uL. He was hypokalemic to 2.7 mmol/L with a creatinine of 8.2 mg/dL and BUN of 86 mg/dL. CT revealed diffuse bowel wall thickening and abdominal pelvic ascites. Inflammatory markers were elevated. Infectious workup was negative for acute infections. C3 complement levels was low to 40 mg/dL. Alternative complement pathway was less than 10. Empiric antibiotics and IV steroids were given due to concern for IBD. Upper endoscopy was unremarkable. Flexible sigmoidoscope up to the transverse colon revealed diffuse, severe inflammation characterized by congestion, erythema and loss of vascularity throughout the examined colon. Biopsies showed chronic colitis with mild to moderate activity. A renal biopsy was consistent with immune mediated acute diffuse proliferative glomerulonephritis and thrombotic microangiopathic changes. A diagnosis of AHUS was established. The patient was started on eculizumab and symptoms resolved. Repeat colonoscopy after 4 month of therapy revealed significant improvement.
Discussion:
Our case provides insight in the diagnostic challenges in distinguishing AHUS from IBD. Complement mediated endothelial injury seen in AHUS can mimic the clinical and histologic features of IBD. As seen in this case, standard treatments of IBD may not treat AHUS and delay care. Early recognition of complement dysfunction and initiation of proper therapy are crucial for improving outcomes. In patients with unexplained colitis in the setting of renal impairment, clinician should maintain a high index of suspicion for AHUS. 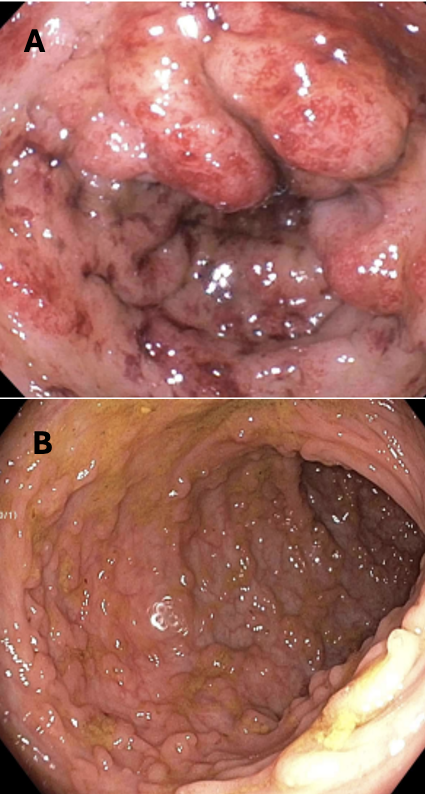
Figure: Figure 1. Diffuse severe inflammation characterized by edema, erythema and loss of vascularity was found in the rectum extending to transverse colon seen on initial Flexible Sigmoidoscopy (A). Repeat colonoscopy performed 4 months after discharge revealing diffuse pseudopolyposis and scarring in entire colon sparing the rectum (B).
Disclosures:
Rebhi Rabah indicated no relevant financial relationships.
Fariha Chowdhury indicated no relevant financial relationships.
Sonny Caceres indicated no relevant financial relationships.
Binyamin Abramowitz indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Niketa Gupta indicated no relevant financial relationships.
Yaniuska Lescaille indicated no relevant financial relationships.
Rebhi Rabah, MD1, Fariha Chowdhury, MD2, Sonny Caceres, MD1, Binyamin Abramowitz, MD1, Narinderjeet Kaur, MD, MS1, Niketa Gupta, MD1, Yaniuska Lescaille, MD, MPH3. P0412 - A Case of Atypical Hemolytic Uremic Syndrome Mimicking IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
