Sunday Poster Session
Category: Colon
P0410 - Silent Colonic Polyposis and Adenocarcinoma in a Young Woman With Refractory Iron Deficiency Anemia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Joselyn De Jesus-Gonzalez, MD (she/her/hers)
Ponce Health Sciences University
Ponce, PR
Presenting Author(s)
Joselyn De Jesus-Gonzalez, MD1, Barbara Rosado-Carrion, MD2, Kathia E. Rosado-Orozco, MD3
1Ponce Health Sciences University, Ponce, Puerto Rico; 2Ponce Health Sciences University, School of Medicine, Ponce, Puerto Rico; 3Hrplabs, San Juan, Puerto Rico
Introduction: Early-onset colorectal cancer associated with diffuse colonic polyposis is uncommon in patients without a known hereditary polyposis syndrome. While most cases involve identifiable germline mutations, rare instances occur without genetic etiology. We present a case of innumerable colonic adenomatous polyposis manifesting as iron deficiency anemia (IDA) in a young patient with no hereditary predisposition.
Case Description/
Methods: A 46-year-old female with controlled type 2 diabetes, asthma, and obesity presented with persistent fatigue, nausea, intermittent vomiting, and palpitations secondary to intractable IDA beginning in 2020. She was hospitalized twice for symptomatic anemia, requiring a total of three units of packed red blood cells. She denied melena, hematochezia, or weight loss. Family history was negative for colorectal cancer. In 2021, she underwent a total abdominal hysterectomy for uterine fibromas, but anemia persisted. Laboratory results showed a hemoglobin level of 8.5 g/dL and a serum iron level of 20 mcg/dL. A positive fecal occult blood test and a poor response to four intravenous iron infusions led to a referral to gastroenterology.
Esophagogastroduodenoscopy revealed multiple 3 mm fundic gland polyps. However, colonoscopy uncovered an unexpected finding: more than 100 adenomatous polyps spanning from the proximal rectum to the cecum, with larger, friable lesions concentrated in the rectosigmoid, splenic flexure and cecum. A 2.2 cm poorly differentiated adenocarcinoma was identified at the splenic flexure, causing luminal narrowing. Multigene panel testing for hereditary polyposis syndromes, including APC, MUTYH, and mismatch repair genes, was negative. She underwent total colectomy with rectal anastomosis and completed adjuvant chemotherapy. Histopathology confirmed stage pT3 pN1b colorectal adenocarcinoma. Postoperative follow-up showed no evidence of recurrence, and the patient remains disease-free at one year.
Discussion: The incidence of early-onset colorectal cancer has been rising among younger populations. Although upper gastrointestinal and gynecologic sources are commonly prioritized in the evaluation of anemia in premenopausal women, this case emphasizes the importance of timely endoscopic assessment when the etiology remains unclear. Including colorectal cancer in the differential diagnosis is essential, as neoplastic disease may develop even in the absence of classic risk factors, family history, or identifiable germline mutations.
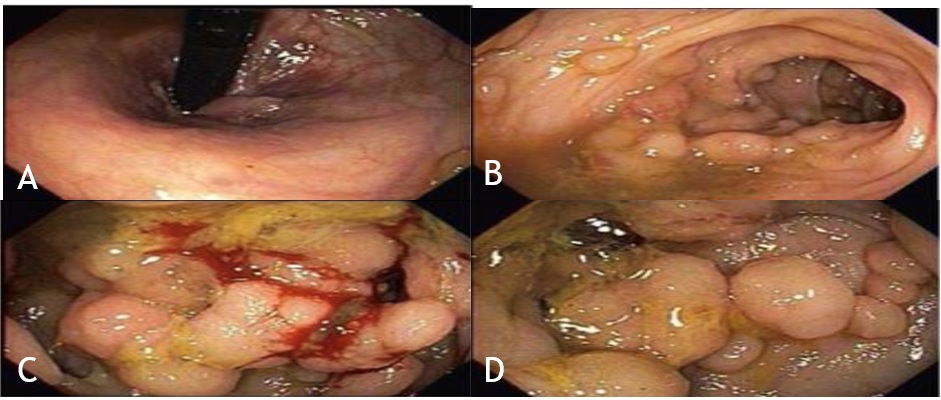
Figure: Figure 1: Colonoscopy findings. (A) Internal Hemorrhoids visualized in retroflexed view of the distal rectum; (B) Multiple large polypoid lesions observed in the rectosigmoid colon; (C) A friable, obstructing mass causing luminal narrowing identified at the splenic flexure; (D) The cecum was nearly completely replaced by innumerable adenomatous polyps.

Figure: Figure 2: Histopathological evaluation. (A) Biopsy of a representative polyp showing a tubular adenoma; (B) Biopsy of the splenic flexure mass revealing invasive adenocarcinoma; (C) Immunohistochemical staining showing preserved MLH1 expression. The tumor retained expression of all mismatch repair proteins, indicating microsatellite stability.
Disclosures:
Joselyn De Jesus-Gonzalez indicated no relevant financial relationships.
Barbara Rosado-Carrion indicated no relevant financial relationships.
Kathia Rosado-Orozco indicated no relevant financial relationships.
Joselyn De Jesus-Gonzalez, MD1, Barbara Rosado-Carrion, MD2, Kathia E. Rosado-Orozco, MD3. P0410 - Silent Colonic Polyposis and Adenocarcinoma in a Young Woman With Refractory Iron Deficiency Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ponce Health Sciences University, Ponce, Puerto Rico; 2Ponce Health Sciences University, School of Medicine, Ponce, Puerto Rico; 3Hrplabs, San Juan, Puerto Rico
Introduction: Early-onset colorectal cancer associated with diffuse colonic polyposis is uncommon in patients without a known hereditary polyposis syndrome. While most cases involve identifiable germline mutations, rare instances occur without genetic etiology. We present a case of innumerable colonic adenomatous polyposis manifesting as iron deficiency anemia (IDA) in a young patient with no hereditary predisposition.
Case Description/
Methods: A 46-year-old female with controlled type 2 diabetes, asthma, and obesity presented with persistent fatigue, nausea, intermittent vomiting, and palpitations secondary to intractable IDA beginning in 2020. She was hospitalized twice for symptomatic anemia, requiring a total of three units of packed red blood cells. She denied melena, hematochezia, or weight loss. Family history was negative for colorectal cancer. In 2021, she underwent a total abdominal hysterectomy for uterine fibromas, but anemia persisted. Laboratory results showed a hemoglobin level of 8.5 g/dL and a serum iron level of 20 mcg/dL. A positive fecal occult blood test and a poor response to four intravenous iron infusions led to a referral to gastroenterology.
Esophagogastroduodenoscopy revealed multiple 3 mm fundic gland polyps. However, colonoscopy uncovered an unexpected finding: more than 100 adenomatous polyps spanning from the proximal rectum to the cecum, with larger, friable lesions concentrated in the rectosigmoid, splenic flexure and cecum. A 2.2 cm poorly differentiated adenocarcinoma was identified at the splenic flexure, causing luminal narrowing. Multigene panel testing for hereditary polyposis syndromes, including APC, MUTYH, and mismatch repair genes, was negative. She underwent total colectomy with rectal anastomosis and completed adjuvant chemotherapy. Histopathology confirmed stage pT3 pN1b colorectal adenocarcinoma. Postoperative follow-up showed no evidence of recurrence, and the patient remains disease-free at one year.
Discussion: The incidence of early-onset colorectal cancer has been rising among younger populations. Although upper gastrointestinal and gynecologic sources are commonly prioritized in the evaluation of anemia in premenopausal women, this case emphasizes the importance of timely endoscopic assessment when the etiology remains unclear. Including colorectal cancer in the differential diagnosis is essential, as neoplastic disease may develop even in the absence of classic risk factors, family history, or identifiable germline mutations.
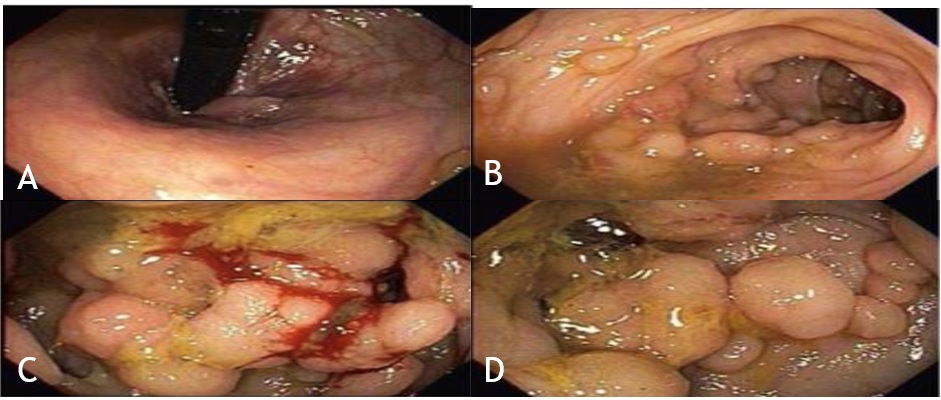
Figure: Figure 1: Colonoscopy findings. (A) Internal Hemorrhoids visualized in retroflexed view of the distal rectum; (B) Multiple large polypoid lesions observed in the rectosigmoid colon; (C) A friable, obstructing mass causing luminal narrowing identified at the splenic flexure; (D) The cecum was nearly completely replaced by innumerable adenomatous polyps.

Figure: Figure 2: Histopathological evaluation. (A) Biopsy of a representative polyp showing a tubular adenoma; (B) Biopsy of the splenic flexure mass revealing invasive adenocarcinoma; (C) Immunohistochemical staining showing preserved MLH1 expression. The tumor retained expression of all mismatch repair proteins, indicating microsatellite stability.
Disclosures:
Joselyn De Jesus-Gonzalez indicated no relevant financial relationships.
Barbara Rosado-Carrion indicated no relevant financial relationships.
Kathia Rosado-Orozco indicated no relevant financial relationships.
Joselyn De Jesus-Gonzalez, MD1, Barbara Rosado-Carrion, MD2, Kathia E. Rosado-Orozco, MD3. P0410 - Silent Colonic Polyposis and Adenocarcinoma in a Young Woman With Refractory Iron Deficiency Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
