Sunday Poster Session
Category: Colon
P0403 - Beyond Adenocarcinoma: A Case of Primary Colonic Diffuse Large B-Cell Lymphoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Varun Vemulapalli, MD
McGovern Medical School at UTHealth
Houston, TX
Presenting Author(s)
Varun Vemulapalli, MD1, Cristina Natha, MD1, Aastha Bharwad, MD2, Ruth Bell, MD1, Alexander Banerjee, MD1, Tanima Jana, MD3
1McGovern Medical School at UTHealth, Houston, TX; 2University of Texas at Houston, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Primary gastrointestinal lymphomas are rare, with the colon representing an uncommon site of involvement. Adenocarcinoma is the most common colorectal malignancy with diffuse large B-cell lymphoma (DLBCL) of the colon accounting for less than 1% of cases. DLBCL requires prompt recognition due to its distinct clinical behavior and management.
Case Description/
Methods: A 50-year-old previously healthy male presented with five days of worsening right-sided abdominal cramping, bloating, and non-bloody emesis. He denied hematochezia, changes in bowel habits, or prior gastrointestinal history. However, he reported mild unintentional weight loss and night sweats over several months. Computed tomography (CT) of the abdomen and pelvis revealed a 12.4 cm centrally necrotic soft tissue mass involving the ascending colon and hepatic flexure with mildly enlarged retroperitoneal and pericolic lymph nodes. No bowel obstruction or metastatic disease was noted. Magnetic resonance imaging (MRI) demonstrated aneurysmal dilation without upstream obstruction—features concerning for lymphoma. Colonoscopy revealed a friable, ulcerated, and traversable mass extending from the cecum to the mid-ascending colon. Biopsies confirmed primary colonic DLBCL, non–germinal center subtype. Immunohistochemistry (IHC) was positive for CD20 and BCL6 and negative for CD3 and CD10, with a high Ki-67 proliferation index of 70–80%. Fluorescence in situ hybridization (FISH) analysis showed no MYC, BCL2, or BCL6 rearrangements. The patient was referred to hematology-oncology and initiated on systemic chemotherapy (R-CHOP).
Discussion: Primary colonic DLBCL is an exceptionally rare malignancy that may initially resemble colorectal adenocarcinoma. However, key distinguishing features—such as systemic B symptoms, aneurysmal dilation with luminal preservation, absence of hematochezia, and a friable yet traversable mass on endoscopy—should raise suspicion for lymphoma. Histologic confirmation is essential, as treatment with systemic chemotherapy differs substantially from the surgical resection typically employed for colorectal adenocarcinoma. This case underscores the importance of maintaining a broad differential diagnosis when evaluating colonic masses to ensure timely recognition, appropriate oncologic management, and optimal patient outcomes.
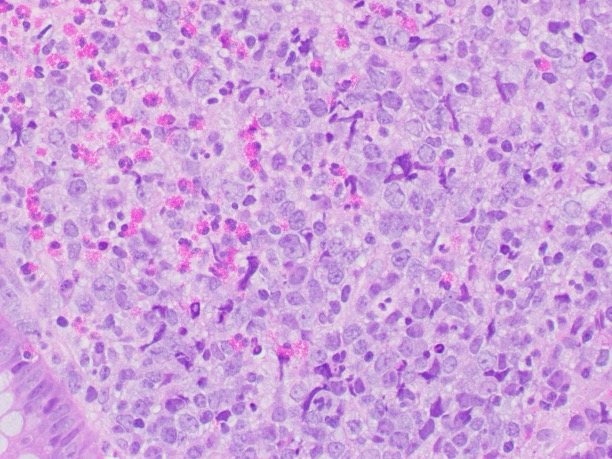
Figure: Distinguishing Features of Colonic Lymphoma and Colorectal Adenocarcinoma
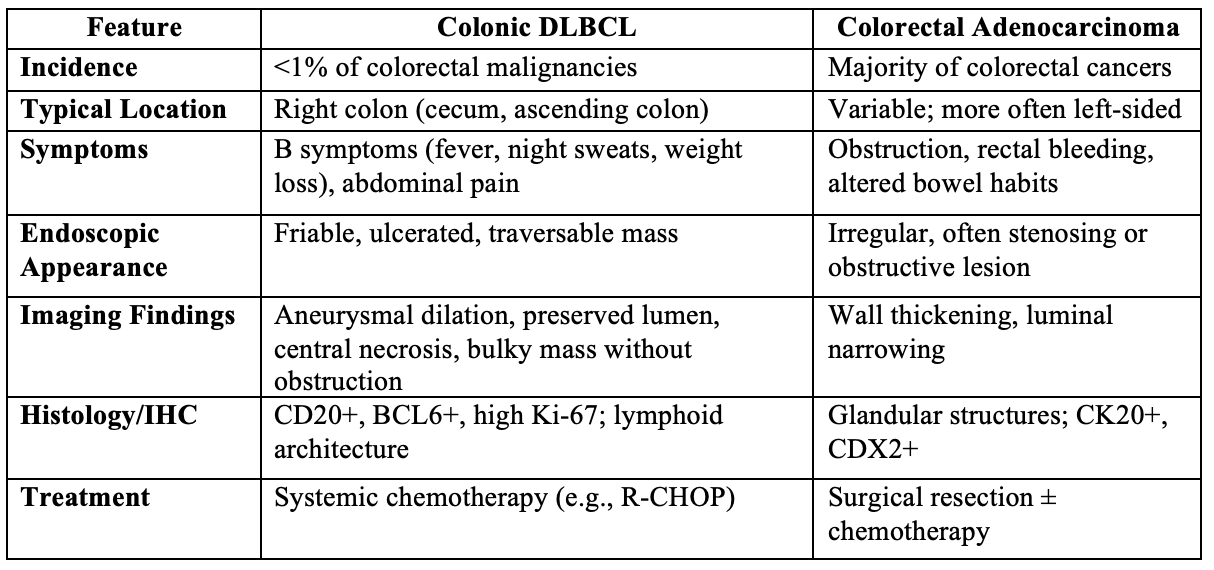
Figure: H&E Cross Section with Focal Diffuse Lymphocytic Infiltrate in a Mixed Inflammatory Background
Disclosures:
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Aastha Bharwad indicated no relevant financial relationships.
Ruth Bell indicated no relevant financial relationships.
Alexander Banerjee indicated no relevant financial relationships.
Tanima Jana indicated no relevant financial relationships.
Varun Vemulapalli, MD1, Cristina Natha, MD1, Aastha Bharwad, MD2, Ruth Bell, MD1, Alexander Banerjee, MD1, Tanima Jana, MD3. P0403 - Beyond Adenocarcinoma: A Case of Primary Colonic Diffuse Large B-Cell Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McGovern Medical School at UTHealth, Houston, TX; 2University of Texas at Houston, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Primary gastrointestinal lymphomas are rare, with the colon representing an uncommon site of involvement. Adenocarcinoma is the most common colorectal malignancy with diffuse large B-cell lymphoma (DLBCL) of the colon accounting for less than 1% of cases. DLBCL requires prompt recognition due to its distinct clinical behavior and management.
Case Description/
Methods: A 50-year-old previously healthy male presented with five days of worsening right-sided abdominal cramping, bloating, and non-bloody emesis. He denied hematochezia, changes in bowel habits, or prior gastrointestinal history. However, he reported mild unintentional weight loss and night sweats over several months. Computed tomography (CT) of the abdomen and pelvis revealed a 12.4 cm centrally necrotic soft tissue mass involving the ascending colon and hepatic flexure with mildly enlarged retroperitoneal and pericolic lymph nodes. No bowel obstruction or metastatic disease was noted. Magnetic resonance imaging (MRI) demonstrated aneurysmal dilation without upstream obstruction—features concerning for lymphoma. Colonoscopy revealed a friable, ulcerated, and traversable mass extending from the cecum to the mid-ascending colon. Biopsies confirmed primary colonic DLBCL, non–germinal center subtype. Immunohistochemistry (IHC) was positive for CD20 and BCL6 and negative for CD3 and CD10, with a high Ki-67 proliferation index of 70–80%. Fluorescence in situ hybridization (FISH) analysis showed no MYC, BCL2, or BCL6 rearrangements. The patient was referred to hematology-oncology and initiated on systemic chemotherapy (R-CHOP).
Discussion: Primary colonic DLBCL is an exceptionally rare malignancy that may initially resemble colorectal adenocarcinoma. However, key distinguishing features—such as systemic B symptoms, aneurysmal dilation with luminal preservation, absence of hematochezia, and a friable yet traversable mass on endoscopy—should raise suspicion for lymphoma. Histologic confirmation is essential, as treatment with systemic chemotherapy differs substantially from the surgical resection typically employed for colorectal adenocarcinoma. This case underscores the importance of maintaining a broad differential diagnosis when evaluating colonic masses to ensure timely recognition, appropriate oncologic management, and optimal patient outcomes.
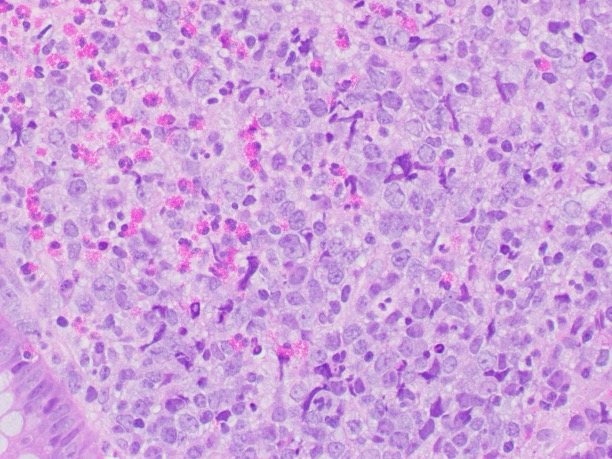
Figure: Distinguishing Features of Colonic Lymphoma and Colorectal Adenocarcinoma
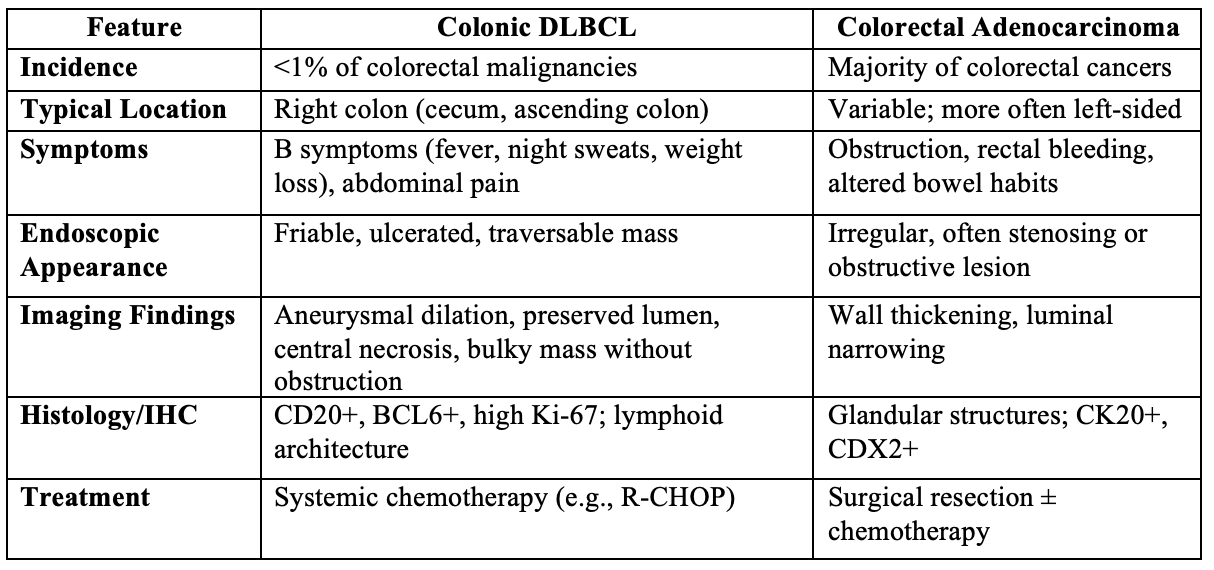
Figure: H&E Cross Section with Focal Diffuse Lymphocytic Infiltrate in a Mixed Inflammatory Background
Disclosures:
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Aastha Bharwad indicated no relevant financial relationships.
Ruth Bell indicated no relevant financial relationships.
Alexander Banerjee indicated no relevant financial relationships.
Tanima Jana indicated no relevant financial relationships.
Varun Vemulapalli, MD1, Cristina Natha, MD1, Aastha Bharwad, MD2, Ruth Bell, MD1, Alexander Banerjee, MD1, Tanima Jana, MD3. P0403 - Beyond Adenocarcinoma: A Case of Primary Colonic Diffuse Large B-Cell Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
