Sunday Poster Session
Category: Colon
P0389 - When Routine Fails: Rapid Onset of Anorectal Melanoma Despite Recent Colonoscopy
- BD
Brian Donahue, BA (he/him/his)
University of Virginia School of Medicine
Charlottesville, VA
Presenting Author(s)
1University of Virginia School of Medicine, Charlottesville, VA; 2University of Virginia, Charlottesville, VA; 3University of Virginia Medical Center, Charlottesville, VA
Introduction: Anorectal melanoma (AM) is a rare and aggressive diagnosis, representing just 1.3% of all melanomas. Patients often experience delayed diagnosis due to multiple factors, including nonspecific symptoms, misdiagnosis, and late presentation. Five-year survival rates are estimated to be between 10% to 20%, a reflection of the challenges associated with an aggressive malignancy. In this case report, we describe a presentation of AM with rapid growth and metastasis.
Case Description/
Methods:
A 77 year-old woman with a past medical history of heart failure and muscular dystrophy presented to the emergency department with abdominal pain. She also reported constipation, nausea, diaphoresis, a 25-pound weight loss, and generalized abdominal pain over the course of the last year. A CT scan of her abdomen from one year prior showed no masses, while colonoscopy from six months prior found three polyps: two tubular adenomas (6mm and 10mm) and one sessile serrated polyp (12mm). On admission, a CT abdomen pelvis with IV contrast revealed a large, irregular mass within the distal rectum at the anal verge measuring 6.6 cm by 4.0 cm with numerous large hepatic lesions, suggestive of a primary colonic neoplasm with hepatic metastasis. The patient then underwent diagnostic colonoscopy which showed a fungating and ulcerated non-obstructing large mass in the rectum just proximal to the anal verge. Biopsies were taken and returned positive for anorectal melanoma. General surgery and medical oncology were consulted for further management recommendations, however the patient opted for hospice care given her poor prognosis.
Discussion: The natural history of development of colorectal adenocarcinoma from a precursor adenoma is estimated at around 10 to 15 years, making it highly amenable to routine screening with colonoscopy. In contrast, AM follows a much more aggressive course. Limited data exists, however, to highlight how rapidly the malignancy may grow. In our case, the patient had been reporting new and non-specific symptoms of constipation and abdominal pain for one year, prompting a colonoscopy just six months prior to presentation with overall benign findings. Despite this, the patient’s symptoms persisted, culminating in her presentation to the ED with abdominal pain and finding of advanced disease. This case highlights an aggressive progression of AM in order to show the limitations of colonoscopy in rapidly-growing colorectal cancers. 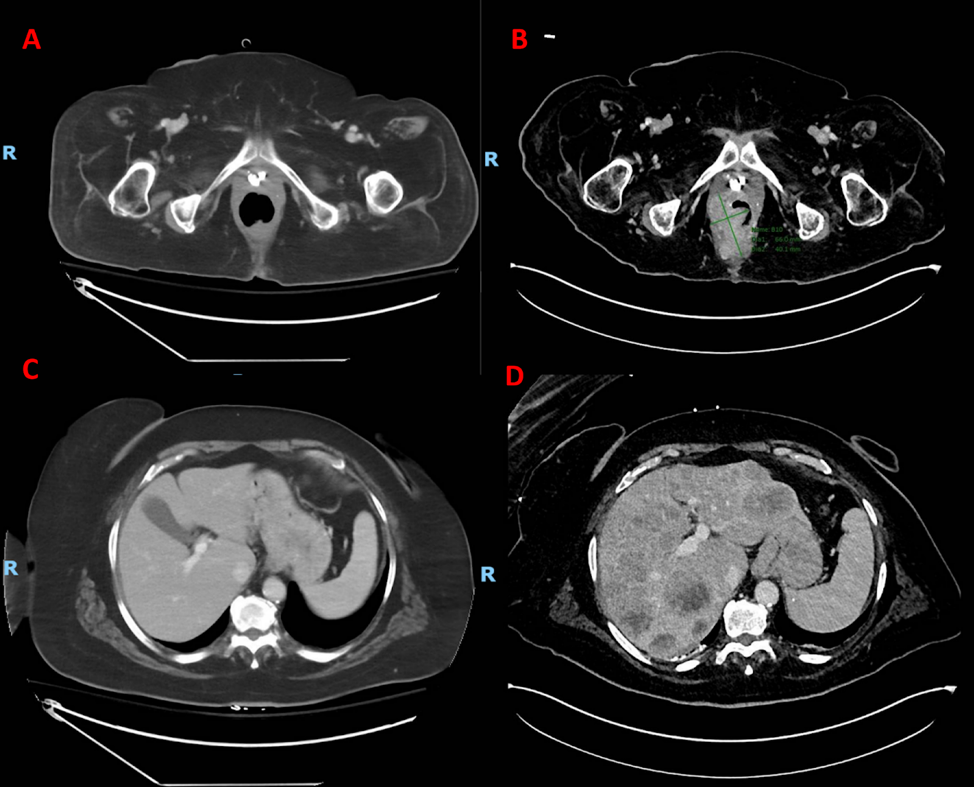
Figure: Figure 1. Endoscopic image of anorectal mass, pathologically diagnosed as anorectal melanoma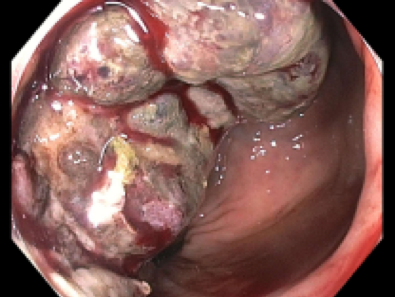
Figure: Figure 2. Side-by-side of the CT abdomen/pelvis one year apart showing development of the mass and liver metastases:
Figure 2A. Rectum one year prior to presentation, normal
Figure 2B. Rectum at admission with evidence of new mass
Figure 2C. Liver one year prior to presentation, normal parenchyma
Figure 2D. Liver at admission with new hepatic metastatic disease
Disclosures:
Brian Donahue indicated no relevant financial relationships.
Deepika Suresh indicated no relevant financial relationships.
Jacob Frenchman indicated no relevant financial relationships.
Amy Doran indicated no relevant financial relationships.
Jeanetta Frye indicated no relevant financial relationships.
Brian Donahue, BA1, Deepika Suresh, MD2, Jacob A.. Frenchman, BS1, Amy Doran, MD3, Jeanetta Frye, MD3. P0389 - When Routine Fails: Rapid Onset of Anorectal Melanoma Despite Recent Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
