Sunday Poster Session
Category: Colon
P0385 - Plaque Attack: When Amyloidosis Strikes the Colon
.jpg)
Rachel Patel, DO
Lehigh Valley Health Network
Coopersburg, PA
Presenting Author(s)
1Lehigh Valley Health Network, Coopersburg, PA; 2Lehigh Valley Health Network, Allentown, PA
Introduction:
Amyloidosis is a rare disorder marked by abnormal deposition of insoluble protein aggregates in tissues and organs, impairing function. Gastrointestinal (GI) involvement is more often seen in systemic forms than in localized disease. We present a rare case of localized GI amyloidosis presenting as persistent subacute diarrhea.
Case Description/
Methods:
A 79-year-old male with a past medical history of coronary artery disease, trans-aortic valve replacement, rheumatoid arthritis, chronic obstructive pulmonary disease, end-stage renal disease on hemodialysis, and recent C. difficile colonization following prolonged antibiotic therapy, presented with a fever, vomiting, and diarrhea. He was admitted for gram-negative bacteremia and Influenza A pneumonia.
Due to persistent subacute diarrhea, a comprehensive stool panel was obtained, revealing C. difficile colonization. Fecal elastase was measured at 71 μg/g and fecal calprotectin was elevated at 182 μg/g. He was maintained on oral vancomycin and initiated on loperamide. Due to persistent nausea, vomiting and a CT scan of the abdomen and pelvis demonstrating diffuse proctocolitis, loperamide was discontinued. Subsequent colonoscopy revealed abnormal mucosa with patchy erythema in the ascending colon and edematous folds in the sigmoid colon, from which biopsies were obtained. Despite treatment with cholestyramine, rifaximin, pancrelipase, and diphenoxylate/atropine, the patient continued to experience refractory non-bloody diarrhea. Due to ongoing hypotension related to diarrhea and overall clinical decline, the patient ultimately elected to pursue home hospice care. Pathological analysis of colonic biopsies confirmed the diagnosis of amyloidosis.
Discussion:
GI amyloidosis remains a diagnostic challenge due to its overlap with more common conditions and lack of distinctive features. It can present as a broad spectrum of clinical manifestations, including weight loss, GI bleeding, altered bowel habits, and malabsorption. Its insidious onset and nonspecific nature of symptoms often result in delayed diagnosis. Histopathological analysis remains essential for definitive diagnosis. This case highlights the diagnostic challenge of GI amyloidosis, particularly in elderly patients with multiple comorbidities. Given the potential for substantial morbidity and mortality, timely diagnosis and appropriate management are critical. Optimizing symptom control and nutritional support can significantly enhance quality of life in affected individuals.
Figure: Colonoscopy revealed abnormal, patchy erythematous mucosa in the ascending colon and edematous folds in the sigmoid colon, suggestive of underlying inflammatory or infiltrative pathology.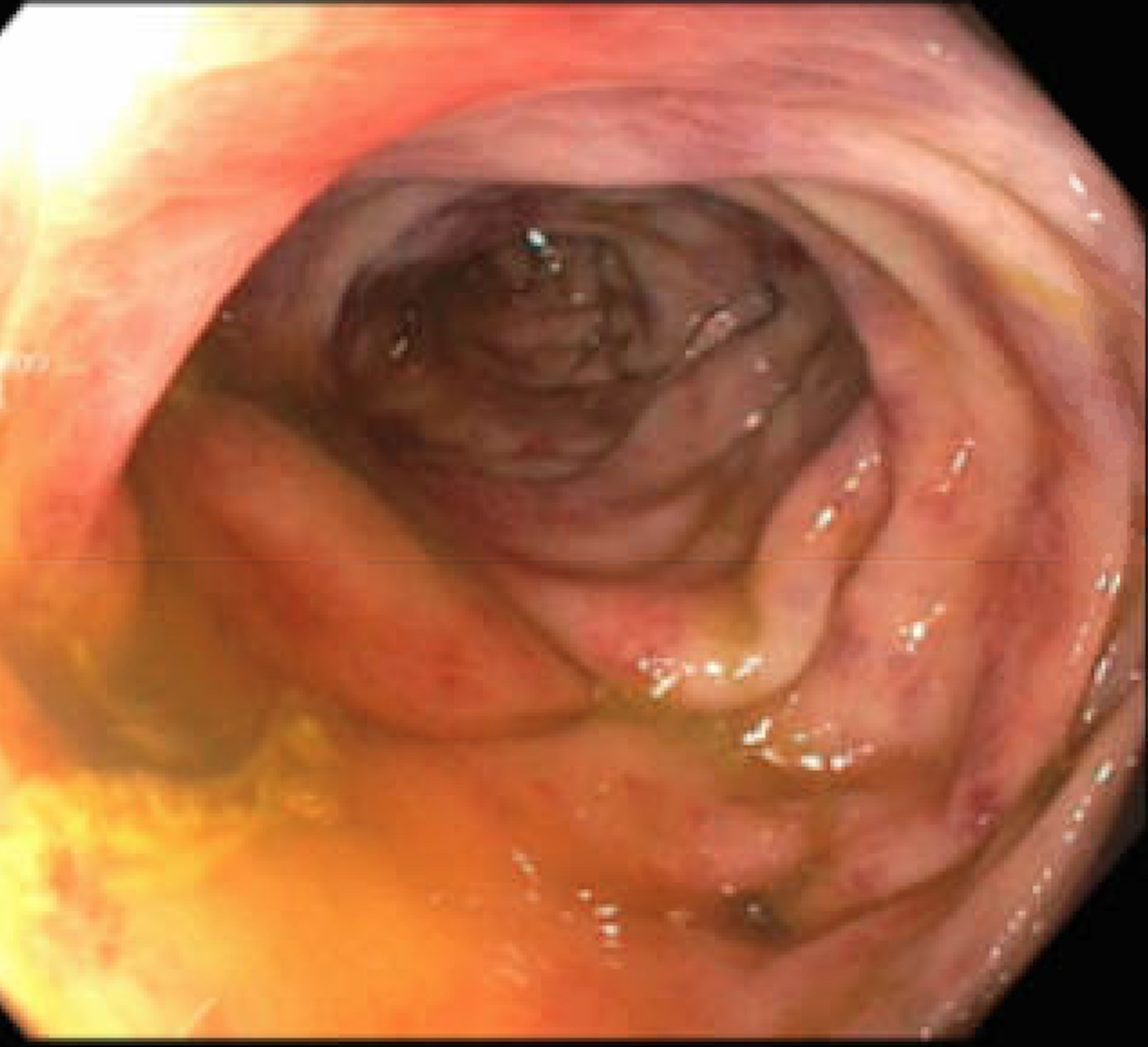
Figure: Additional image of patchy erythema noted at localized area of the ascending colon, raising concern for underlying mucosal inflammation or infiltrative disease.
Disclosures:
Rachel Patel indicated no relevant financial relationships.
Sarah Elrod indicated no relevant financial relationships.
Neil Patel indicated no relevant financial relationships.
Michael Engels indicated no relevant financial relationships.
Aaron Mendelson indicated no relevant financial relationships.
Rachel Patel, DO1, Sarah Elrod, DO2, Neil Patel, DO2, Michael Engels, MD2, Aaron Mendelson, MD2. P0385 - Plaque Attack: When Amyloidosis Strikes the Colon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
