Sunday Poster Session
Category: Colon
P0307 - Colonic Transit Time: A Forgotten Modality– A Systematic Narrative Review
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Shivam Kalra, MBBS, MHA (he/him/his)
Trident Medical Center
North Charleston, SC
Presenting Author(s)
Shivam Kalra, MBBS, MHA1, Manjeet Kumar Goyal, MBBS, MD, DM, DNB2, Ayushi Garg, MD1, Abhinav Rao, MD1, Salvatore A Moscatello, MD1, Omesh Goyal, MBBS, MD, DM3
1Trident Medical Center, North Charleston, SC; 2Cleveland Clinic Akron General, Akron, OH; 3Dayanand Medical College and Hospital, Ludhiana, Punjab, India
Introduction: Functional constipation (FC) imposes a significant burden worldwide. Accurate subtyping—normal transit constipation (NTC), slow transit constipation (STC), and dyssynergic defecation (DD)—is important, but colonic transit time (CTT) assessment remains underused, particularly in diverse and resource-limited settings.
Methods: We performed a systematic narrative review of CTT measurement methodologies, clinical relevance, ethnic variability, and regional adaptations, with emphasis on Indian and Asian populations compared to Western cohorts.
Results:
CTT protocols vary widely across different populations and research contexts, with marker quantities ranging from 20 to 50 per day to balance marker visibility and patient compliance. X-ray acquisition timing ranges from 27 hours to 11 days post-marker ingestion, reflecting local practices and patient characteristics. Supine positioning for abdominal radiographs is most common to improve image quality and reduce radiation exposure.
Asian populations (e.g., India, Korea) consistently report faster colonic transit times (mean ~15.4 hours) compared to Western populations (30–40 hours), highlighting the critical need for population-specific normative data to ensure accurate interpretation. Diagnostic protocols have been adapted for subgroups such as pediatric patients and individuals with neurogenic disorders, further underscoring the necessity for tailored CTT approaches.
Despite its clinical value in differentiating constipation subtypes and informing management—particularly in refractory cases—CTT remains a “forgotten modality,” underutilized due to limited clinician awareness, lack of standardized protocols, and resource constraints
Discussion: CTT measurement, while often overlooked, is a powerful diagnostic tool for precise constipation subtyping and management optimization. Standardized, regionally validated protocols and broader adoption are urgently needed. To mitigate these limitations, supine position is preferred for abdominal radiograph in a ROM study because it results in significantly lower radiation dose and better image quality compared to erect position. Educational initiatives and technological innovations, including AI-based radiograph interpretation, can revitalize CTT as a cornerstone of constipation care, especially in Asian and resource-limited settings.
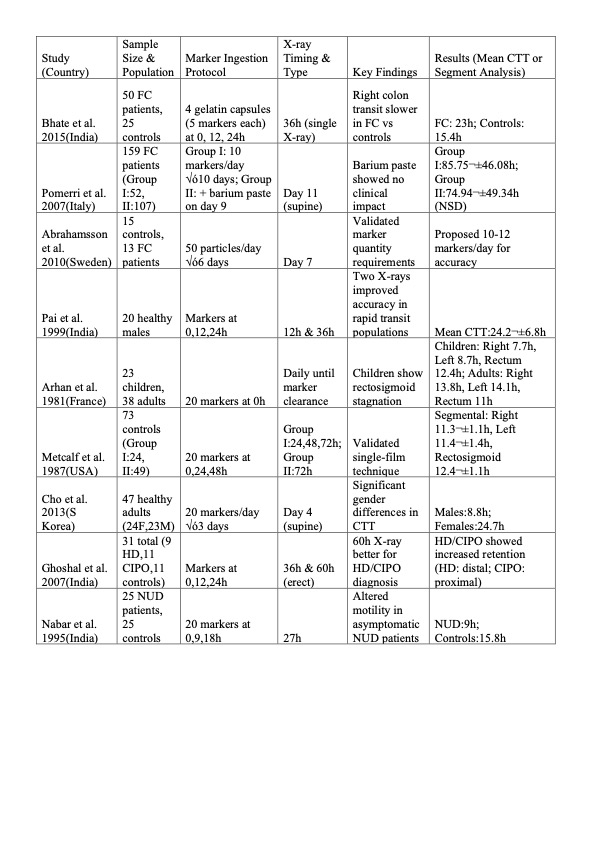
Figure: Comparison of Previously Studied Protocols

Figure: Classification of Constipation
Disclosures:
Shivam Kalra indicated no relevant financial relationships.
Manjeet Kumar Goyal indicated no relevant financial relationships.
Ayushi Garg indicated no relevant financial relationships.
Abhinav Rao indicated no relevant financial relationships.
Salvatore A Moscatello indicated no relevant financial relationships.
Omesh Goyal indicated no relevant financial relationships.
Shivam Kalra, MBBS, MHA1, Manjeet Kumar Goyal, MBBS, MD, DM, DNB2, Ayushi Garg, MD1, Abhinav Rao, MD1, Salvatore A Moscatello, MD1, Omesh Goyal, MBBS, MD, DM3. P0307 - Colonic Transit Time: A Forgotten Modality– A Systematic Narrative Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Trident Medical Center, North Charleston, SC; 2Cleveland Clinic Akron General, Akron, OH; 3Dayanand Medical College and Hospital, Ludhiana, Punjab, India
Introduction: Functional constipation (FC) imposes a significant burden worldwide. Accurate subtyping—normal transit constipation (NTC), slow transit constipation (STC), and dyssynergic defecation (DD)—is important, but colonic transit time (CTT) assessment remains underused, particularly in diverse and resource-limited settings.
Methods: We performed a systematic narrative review of CTT measurement methodologies, clinical relevance, ethnic variability, and regional adaptations, with emphasis on Indian and Asian populations compared to Western cohorts.
Results:
CTT protocols vary widely across different populations and research contexts, with marker quantities ranging from 20 to 50 per day to balance marker visibility and patient compliance. X-ray acquisition timing ranges from 27 hours to 11 days post-marker ingestion, reflecting local practices and patient characteristics. Supine positioning for abdominal radiographs is most common to improve image quality and reduce radiation exposure.
Asian populations (e.g., India, Korea) consistently report faster colonic transit times (mean ~15.4 hours) compared to Western populations (30–40 hours), highlighting the critical need for population-specific normative data to ensure accurate interpretation. Diagnostic protocols have been adapted for subgroups such as pediatric patients and individuals with neurogenic disorders, further underscoring the necessity for tailored CTT approaches.
Despite its clinical value in differentiating constipation subtypes and informing management—particularly in refractory cases—CTT remains a “forgotten modality,” underutilized due to limited clinician awareness, lack of standardized protocols, and resource constraints
Discussion: CTT measurement, while often overlooked, is a powerful diagnostic tool for precise constipation subtyping and management optimization. Standardized, regionally validated protocols and broader adoption are urgently needed. To mitigate these limitations, supine position is preferred for abdominal radiograph in a ROM study because it results in significantly lower radiation dose and better image quality compared to erect position. Educational initiatives and technological innovations, including AI-based radiograph interpretation, can revitalize CTT as a cornerstone of constipation care, especially in Asian and resource-limited settings.
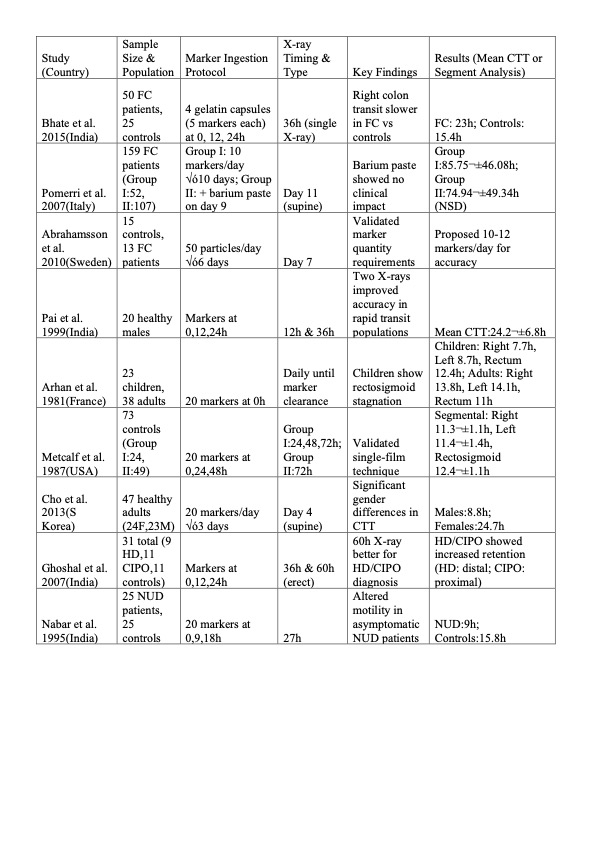
Figure: Comparison of Previously Studied Protocols

Figure: Classification of Constipation
Disclosures:
Shivam Kalra indicated no relevant financial relationships.
Manjeet Kumar Goyal indicated no relevant financial relationships.
Ayushi Garg indicated no relevant financial relationships.
Abhinav Rao indicated no relevant financial relationships.
Salvatore A Moscatello indicated no relevant financial relationships.
Omesh Goyal indicated no relevant financial relationships.
Shivam Kalra, MBBS, MHA1, Manjeet Kumar Goyal, MBBS, MD, DM, DNB2, Ayushi Garg, MD1, Abhinav Rao, MD1, Salvatore A Moscatello, MD1, Omesh Goyal, MBBS, MD, DM3. P0307 - Colonic Transit Time: A Forgotten Modality– A Systematic Narrative Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
