Sunday Poster Session
Category: Colon
P0272 - Antidepressants and Microscopic Colitis: A Propensity-Matched Comparison to Bupropion
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Morgan R. Starkey, MD (she/her/hers)
MetroHealth Medical Center
Aurora, OH
Presenting Author(s)
Morgan R. Starkey, MD1, Andrew Ford, MD2, Michael Kurin, MD2
1MetroHealth Medical Center, Cleveland, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Selective serotonin reuptake inhibitors (SSRIs) and serotonin–norepinephrine reuptake inhibitors (SNRIs) are some of the most frequently prescribed medications in the US, with 150 million prescriptions dispensed in 2022 alone. While SSRIs/SNRIs have long been linked to microscopic colitis (MC), studies on the association remain limited. Given the widespread use of these medications, this study aims to determine whether prior use of SSRIs or SNRIs is associated with an increased odds of developing MC.
Methods: A TriNetx case-control study was conducted comparing patients who initiated SSRIs or SNRIs to those prescribed bupropion, an atypical antidepressant not previously implicated in MC. The primary outcome was the development of microscopic colitis after antidepressant initiation. Propensity score matching was performed to balance cohorts on age, gender, race, smoking status, and other relevant confounders. Patients with known alternative causes of colitis and those with recent NSAID, PPI, or statin use were excluded.
Results: After propensity score matching, ten antidepressant exposure groups (including SSRIs and SNRIs) were compared to bupropion for the development of microscopic colitis. Both SSRIs and SNRIs as medication classes were associated with significantly lower odds of developing microscopic colitis compared to bupropion (SSRI OR 0.68, 95% CI 0.54–0.86, p = 0.001; SNRI OR 0.64, 95% CI 0.50–0.81, p = 0.0002). Among individual agents, duloxetine (OR 0.79, 95% CI 0.45–0.77, p < 0.0001), escitalopram (OR 0.77, 95% CI 0.60–0.98, p = 0.04), and paroxetine (OR 0.66, 95% CI 0.45–0.97, p = 0.03) were also significantly associated with decreased odds. Other individual agents, including sertraline, fluoxetine, venlafaxine, and desvenlafaxine, were not significantly associated with MC compared to bupropion.
Discussion: In this large, multi-institutional propensity-matched analysis, SSRIs and SNRIs were not associated with increased odds of developing microscopic colitis compared to bupropion. Several agents, duloxetine, escitalopram, and paroxetine, were associated with a significantly lower risk. These findings challenge previous assumptions about the role of serotonergic antidepressants in MC pathogenesis and suggest that their use may not confer additional risk compared to bupropion. Further prospective studies are warranted to better understand underlying mechanisms and confirm these associations in broader populations.
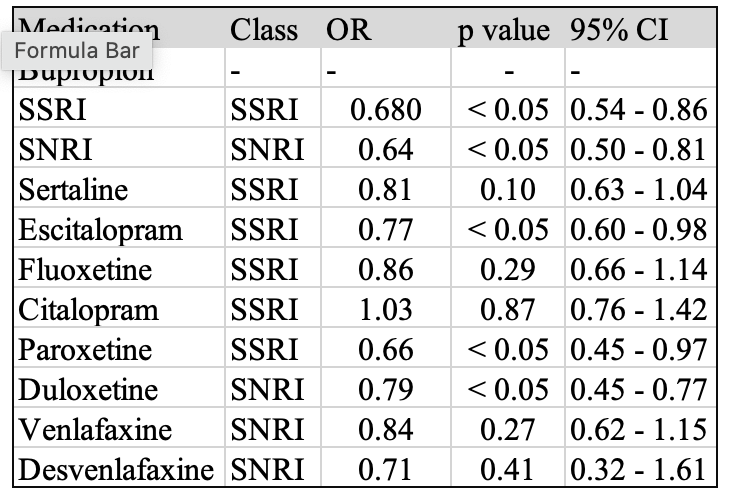
Figure: Table 1. Propensity-matched odds ratios for microscopic colitis following antidepressant use compared to buproprion
Disclosures:
Morgan Starkey indicated no relevant financial relationships.
Andrew Ford indicated no relevant financial relationships.
Michael Kurin indicated no relevant financial relationships.
Morgan R. Starkey, MD1, Andrew Ford, MD2, Michael Kurin, MD2. P0272 - Antidepressants and Microscopic Colitis: A Propensity-Matched Comparison to Bupropion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MetroHealth Medical Center, Cleveland, OH; 2Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Selective serotonin reuptake inhibitors (SSRIs) and serotonin–norepinephrine reuptake inhibitors (SNRIs) are some of the most frequently prescribed medications in the US, with 150 million prescriptions dispensed in 2022 alone. While SSRIs/SNRIs have long been linked to microscopic colitis (MC), studies on the association remain limited. Given the widespread use of these medications, this study aims to determine whether prior use of SSRIs or SNRIs is associated with an increased odds of developing MC.
Methods: A TriNetx case-control study was conducted comparing patients who initiated SSRIs or SNRIs to those prescribed bupropion, an atypical antidepressant not previously implicated in MC. The primary outcome was the development of microscopic colitis after antidepressant initiation. Propensity score matching was performed to balance cohorts on age, gender, race, smoking status, and other relevant confounders. Patients with known alternative causes of colitis and those with recent NSAID, PPI, or statin use were excluded.
Results: After propensity score matching, ten antidepressant exposure groups (including SSRIs and SNRIs) were compared to bupropion for the development of microscopic colitis. Both SSRIs and SNRIs as medication classes were associated with significantly lower odds of developing microscopic colitis compared to bupropion (SSRI OR 0.68, 95% CI 0.54–0.86, p = 0.001; SNRI OR 0.64, 95% CI 0.50–0.81, p = 0.0002). Among individual agents, duloxetine (OR 0.79, 95% CI 0.45–0.77, p < 0.0001), escitalopram (OR 0.77, 95% CI 0.60–0.98, p = 0.04), and paroxetine (OR 0.66, 95% CI 0.45–0.97, p = 0.03) were also significantly associated with decreased odds. Other individual agents, including sertraline, fluoxetine, venlafaxine, and desvenlafaxine, were not significantly associated with MC compared to bupropion.
Discussion: In this large, multi-institutional propensity-matched analysis, SSRIs and SNRIs were not associated with increased odds of developing microscopic colitis compared to bupropion. Several agents, duloxetine, escitalopram, and paroxetine, were associated with a significantly lower risk. These findings challenge previous assumptions about the role of serotonergic antidepressants in MC pathogenesis and suggest that their use may not confer additional risk compared to bupropion. Further prospective studies are warranted to better understand underlying mechanisms and confirm these associations in broader populations.
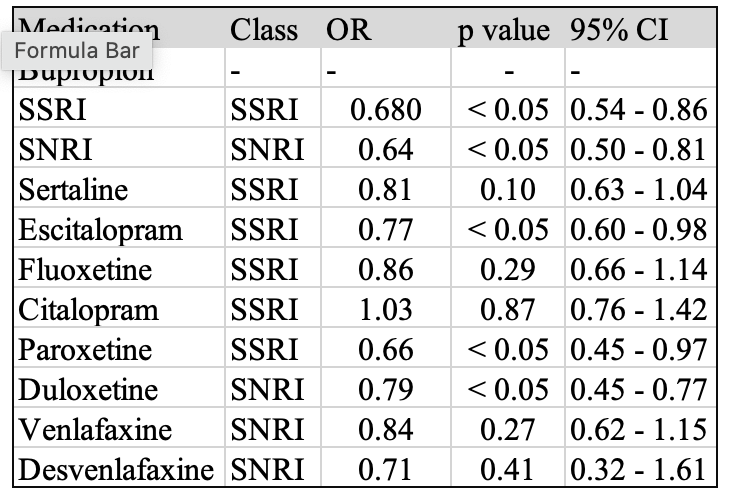
Figure: Table 1. Propensity-matched odds ratios for microscopic colitis following antidepressant use compared to buproprion
Disclosures:
Morgan Starkey indicated no relevant financial relationships.
Andrew Ford indicated no relevant financial relationships.
Michael Kurin indicated no relevant financial relationships.
Morgan R. Starkey, MD1, Andrew Ford, MD2, Michael Kurin, MD2. P0272 - Antidepressants and Microscopic Colitis: A Propensity-Matched Comparison to Bupropion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
