Sunday Poster Session
Category: Colon
P0259 - Referral Roadblocks: Underutilization of Genetic Evaluation in Colorectal Cancer Patients With Loss of MLH-1 and PMS-2
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Qusai Al Zureikat, MD (he/him/his)
MedStar Health-Georgetown/Washington Hospital Center
Washington, DC
Presenting Author(s)
Qusai Al Zureikat, MD1, Ruben Alberto Hiraldo, MD2, Samuel Speizman, BS3, Rashmi Samdani, MD2, Priyanka Kanth, MD2
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2MedStar Georgetown University Hospital, Washington, DC; 3Georgetown University School of Medicine, Washington, DC
Introduction: Mismatch repair (MMR) immunohistochemistry is a standard part of colorectal cancer (CRC) diagnostics, used to identify patients at risk for Lynch syndrome (LS). When tumors show loss of MLH1 and PMS2, testing for BRAF mutation or MLH1 promoter hypermethylation helps distinguish sporadic cases from LS. If negative, current guidelines recommend referral to genetic counseling and germline testing. Despite clear recommendations, adherence remains inconsistent. This study evaluated referral patterns, testing completion, and barriers among eligible patients with MLH1/PMS2 loss across a multi-center system.
Methods: A retrospective chart review was conducted on 102 CRC patients with MLH1/PMS2 loss between January 2022 and December 2024. After excluding patients with BRAF mutation or MLH1 hypermethylation, 64 were eligible. Demographics, immunohistochemical findings, referral/testing outcomes, and documented barriers were collected. Chi-square tests assessed differences in referral and counseling completion by site of care.
Results: Among the 64 eligible patients, mean age was 70; 55% were female. The cohort included 53% White, 37.7% African American, and 9.3% Asian patients. A history of other cancers was documented in 25%, with breast cancer in 33% of those. A total of 23 patients (35.9%) were seen at a university hospital and 41 (64.1%) at community hospitals. MLH1 loss was seen in 69% and PMS2 loss in 71.8%. Only 24 patients (37.5%) were referred to genetic counseling—10 of 23 (43.5%) at the university site and 14 of 41 (34.1%) at community sites. Of those referred, 13 (54.2%) completed germline testing—6 at the university and 7 at community sites—representing 20.3% of all eligible patients. Referral rates did not differ significantly between sites (χ² = 0.026, p = 0.871), nor did completion rates (χ² = 0.725, p = 0.394). The most common barrier was lack of provider initiation (63%). Patient-related barriers, including language, transportation, and relocation, were noted in 23%.
Discussion: Despite eligibility, fewer than 40% were referred, and only one in five completed testing. Referral and testing rates were slightly higher at the university site but remained suboptimal. Lack of provider referral was the main barrier, though social determinants contributed. These findings highlight the need for systems-based solutions—automated referrals, provider education, and navigation support—to improve LS evaluation and reduce disparities in access to genetic services.
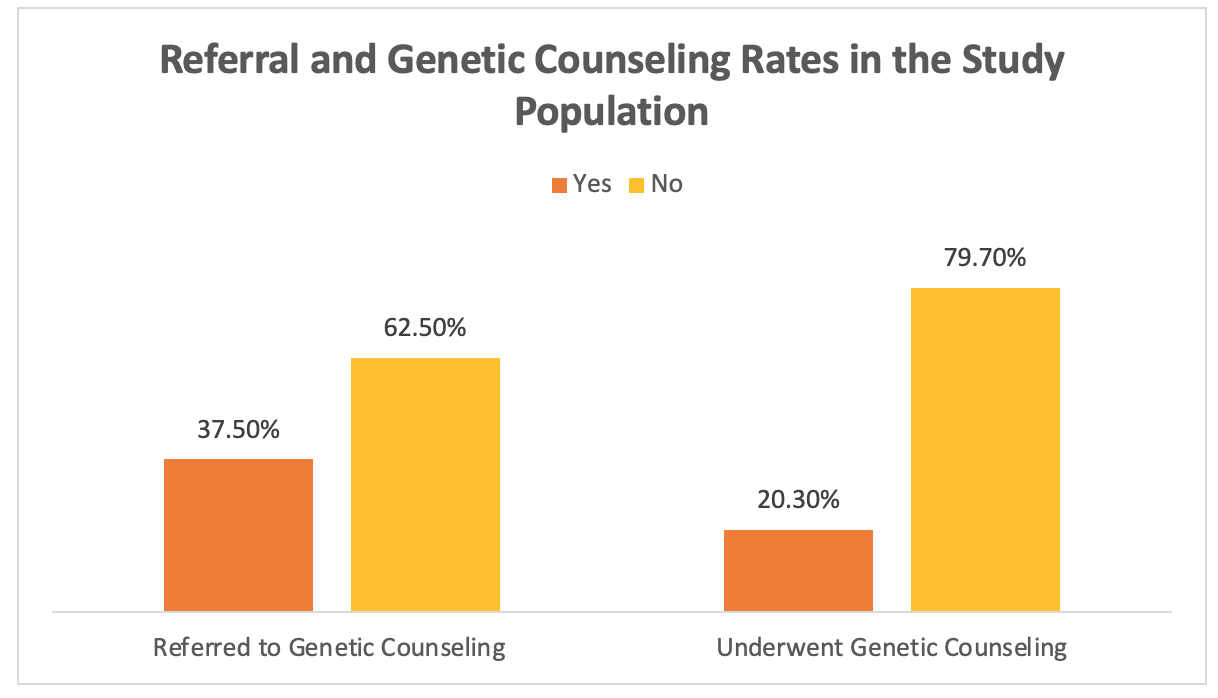
Figure: Graph 1: Referral and Genetic Counseling Rates in the Study Population
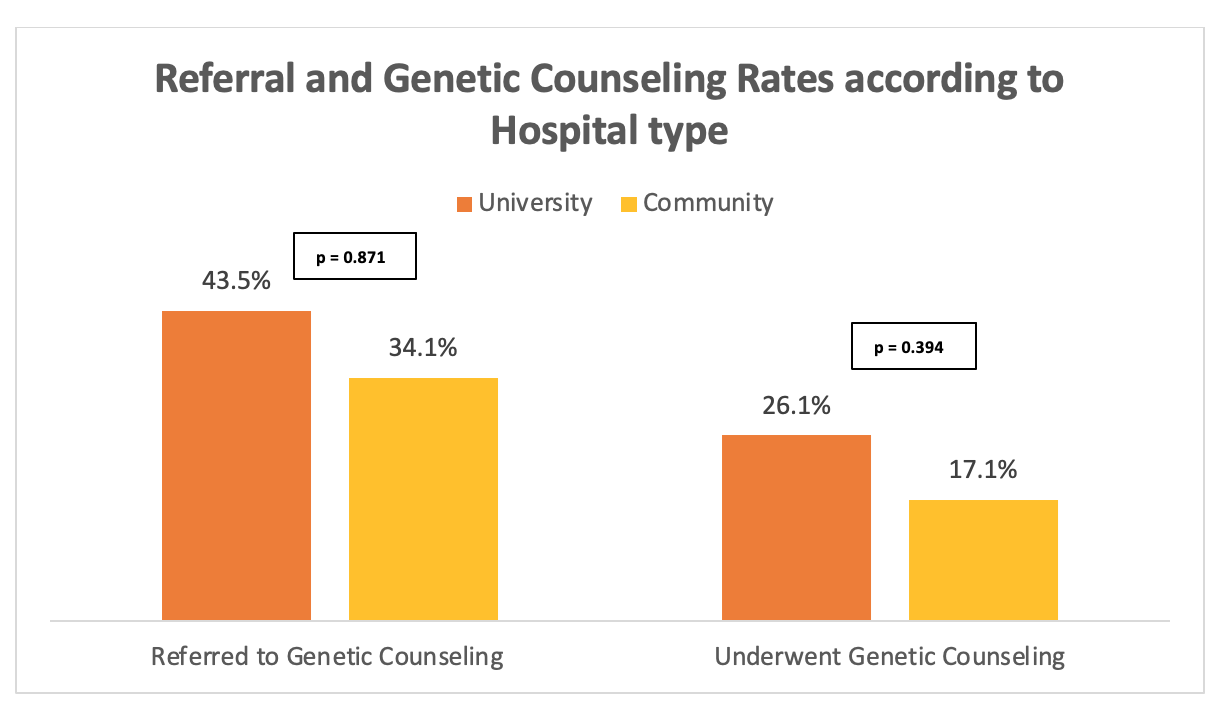
Figure: Graph 2: Referral and Genetic Counseling Rates according to Hospital type
Disclosures:
Qusai Al Zureikat indicated no relevant financial relationships.
Ruben Alberto Hiraldo indicated no relevant financial relationships.
Samuel Speizman indicated no relevant financial relationships.
Rashmi Samdani indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Qusai Al Zureikat, MD1, Ruben Alberto Hiraldo, MD2, Samuel Speizman, BS3, Rashmi Samdani, MD2, Priyanka Kanth, MD2. P0259 - Referral Roadblocks: Underutilization of Genetic Evaluation in Colorectal Cancer Patients With Loss of MLH-1 and PMS-2, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2MedStar Georgetown University Hospital, Washington, DC; 3Georgetown University School of Medicine, Washington, DC
Introduction: Mismatch repair (MMR) immunohistochemistry is a standard part of colorectal cancer (CRC) diagnostics, used to identify patients at risk for Lynch syndrome (LS). When tumors show loss of MLH1 and PMS2, testing for BRAF mutation or MLH1 promoter hypermethylation helps distinguish sporadic cases from LS. If negative, current guidelines recommend referral to genetic counseling and germline testing. Despite clear recommendations, adherence remains inconsistent. This study evaluated referral patterns, testing completion, and barriers among eligible patients with MLH1/PMS2 loss across a multi-center system.
Methods: A retrospective chart review was conducted on 102 CRC patients with MLH1/PMS2 loss between January 2022 and December 2024. After excluding patients with BRAF mutation or MLH1 hypermethylation, 64 were eligible. Demographics, immunohistochemical findings, referral/testing outcomes, and documented barriers were collected. Chi-square tests assessed differences in referral and counseling completion by site of care.
Results: Among the 64 eligible patients, mean age was 70; 55% were female. The cohort included 53% White, 37.7% African American, and 9.3% Asian patients. A history of other cancers was documented in 25%, with breast cancer in 33% of those. A total of 23 patients (35.9%) were seen at a university hospital and 41 (64.1%) at community hospitals. MLH1 loss was seen in 69% and PMS2 loss in 71.8%. Only 24 patients (37.5%) were referred to genetic counseling—10 of 23 (43.5%) at the university site and 14 of 41 (34.1%) at community sites. Of those referred, 13 (54.2%) completed germline testing—6 at the university and 7 at community sites—representing 20.3% of all eligible patients. Referral rates did not differ significantly between sites (χ² = 0.026, p = 0.871), nor did completion rates (χ² = 0.725, p = 0.394). The most common barrier was lack of provider initiation (63%). Patient-related barriers, including language, transportation, and relocation, were noted in 23%.
Discussion: Despite eligibility, fewer than 40% were referred, and only one in five completed testing. Referral and testing rates were slightly higher at the university site but remained suboptimal. Lack of provider referral was the main barrier, though social determinants contributed. These findings highlight the need for systems-based solutions—automated referrals, provider education, and navigation support—to improve LS evaluation and reduce disparities in access to genetic services.
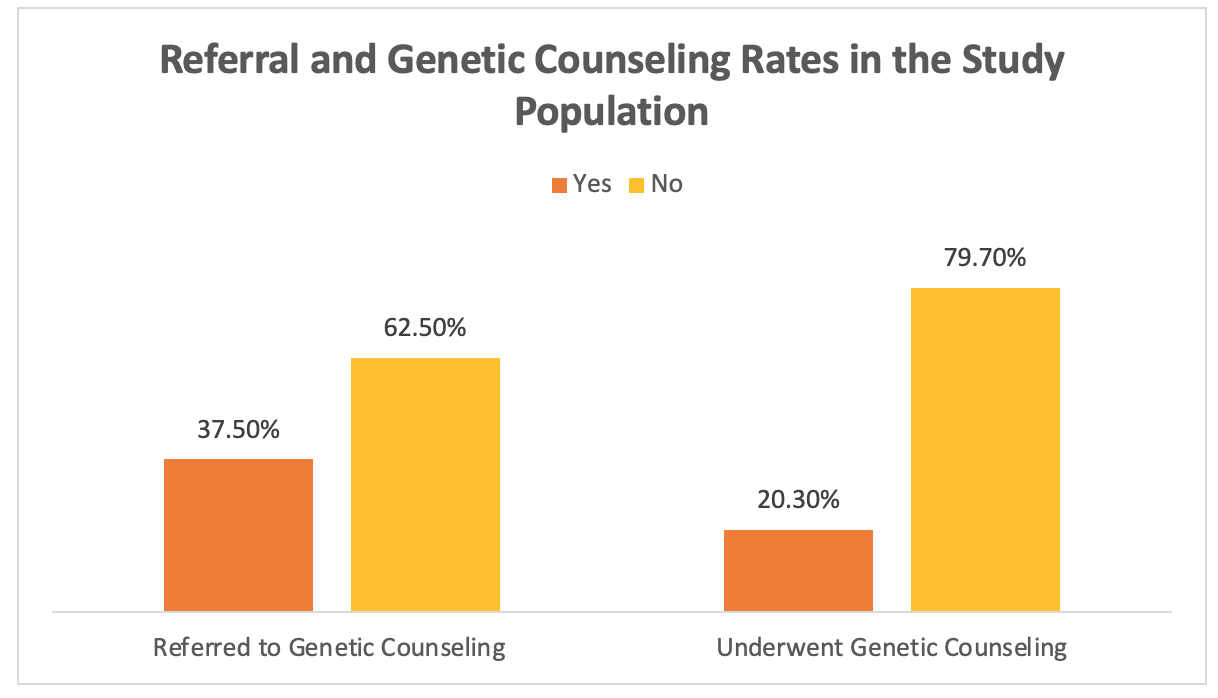
Figure: Graph 1: Referral and Genetic Counseling Rates in the Study Population
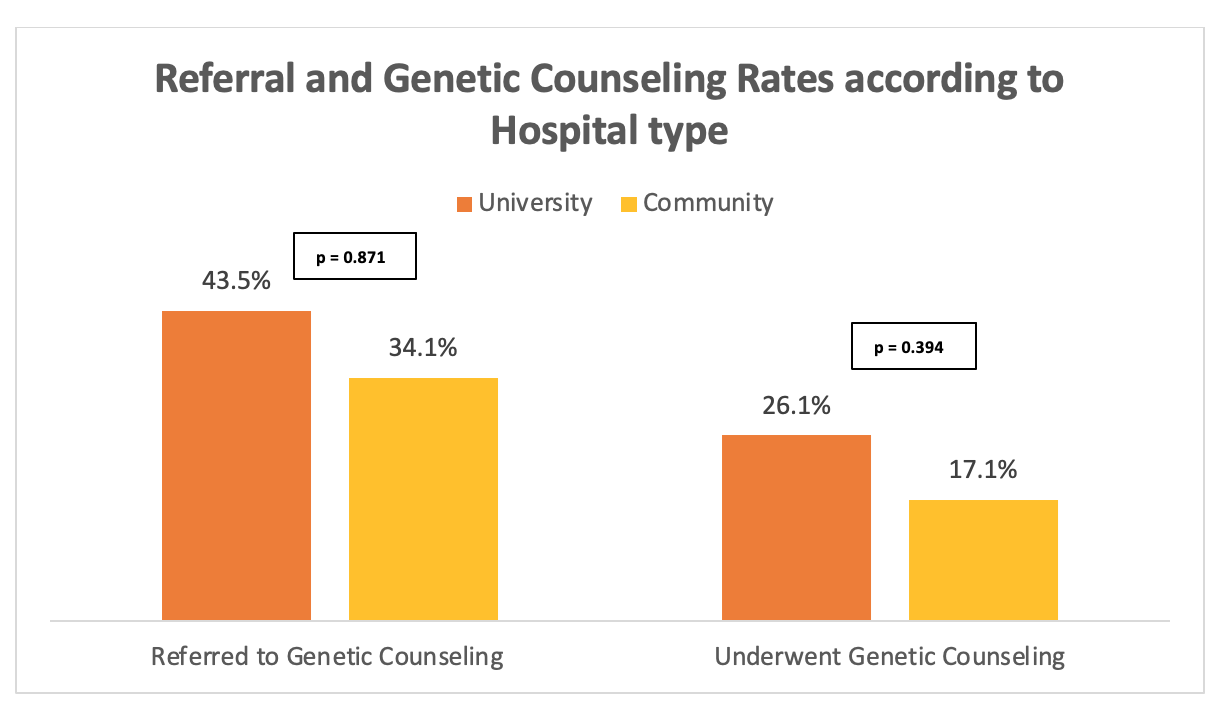
Figure: Graph 2: Referral and Genetic Counseling Rates according to Hospital type
Disclosures:
Qusai Al Zureikat indicated no relevant financial relationships.
Ruben Alberto Hiraldo indicated no relevant financial relationships.
Samuel Speizman indicated no relevant financial relationships.
Rashmi Samdani indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Qusai Al Zureikat, MD1, Ruben Alberto Hiraldo, MD2, Samuel Speizman, BS3, Rashmi Samdani, MD2, Priyanka Kanth, MD2. P0259 - Referral Roadblocks: Underutilization of Genetic Evaluation in Colorectal Cancer Patients With Loss of MLH-1 and PMS-2, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

