Sunday Poster Session
Category: Biliary/Pancreas
P0249 - The Impostor Within: Contained Gastric Perforation Mimicking Pancreatic Walled-Off Necrosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Shriraj Patel, DO
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Shriraj Patel, DO1, Pranav Patel, MD2, Harshit S. Khara, MD3, Bradley D. Confer, DO2
1Geisinger Medical Center, Danville, PA; 2Geisinger Health System, Danville, PA; 3Geisinger Health System, Danville, NJ
Introduction: The Atlanta classification defines walled-off necrosis (WON) as a mature, encapsulated collection of necrotic tissue that develops at least four weeks after necrotizing pancreatitis. Although imaging and clinical context guide diagnosis, overlapping features may obscure alternative etiologies. We present a case of presumed early walled-off pancreatic necrosis (WOPN) that was instead a contained gastric ulcer perforation with rapid wall formation.
Case Description/
Methods: A 59-year-old obese male with history of alcohol use disorder and recurrent pancreatitis presented with sharp epigastric pain and a lipase >2000 U/L, consistent with acute pancreatitis. A computed tomography (CT) scan on hospital day two revealed an acute peripancreatic necrotic fluid collection without wall formation. For peritoneal signs on day three, repeat CT demonstrated interval enlargement of the peripancreatic fluid collection with early wall formation, presumed to be WOPN. Esophagogastroduodenoscopy (EGD) with endoscopic ultrasound (EUS) revealed a > 10 cm x 10 cm walled-off necrosis, drained via EUS-guided cystogastrostomy using two lumen-apposing metal stents in the proximal and distal gastric body (multiple transluminal gateway technique). A total of three necrosectomies were performed. During the second, a large gastric body ulcer was discovered. Given the ulcer’s proximity to the necrotic cavity with rapid wall formation within 13 days of pancreatitis, a contained gastric perforation was suspected to be the true etiology, not WOPN. The patient was ultimately discharged in stable condition to rehab with outpatient monitoring.
Discussion: This case illustrates the importance of challenging diagnostic assumptions. Given the history of alcohol use disorder, the patient’s fluid collection was initially attributed to his presentation with pancreatitis. However, the timeline was not consistent with typical WOPN. Radiographic and endoscopic findings concluded that the peripancreatic fluid collection was instead a result of a contained gastric ulcer perforation with rapid wall formation. The enlarging fluid collection was likely due to intraluminal hemorrhage with clot formation and necrotic cavity expansion adjacent to the stomach. This case underscores the risk of anchoring bias in pancreatic pathology and highlights the diagnostic value of endoscopy when imaging is non-specific. Early recognition of contained gastric perforation can guide timely intervention and avoid unnecessary or mistimed procedures.
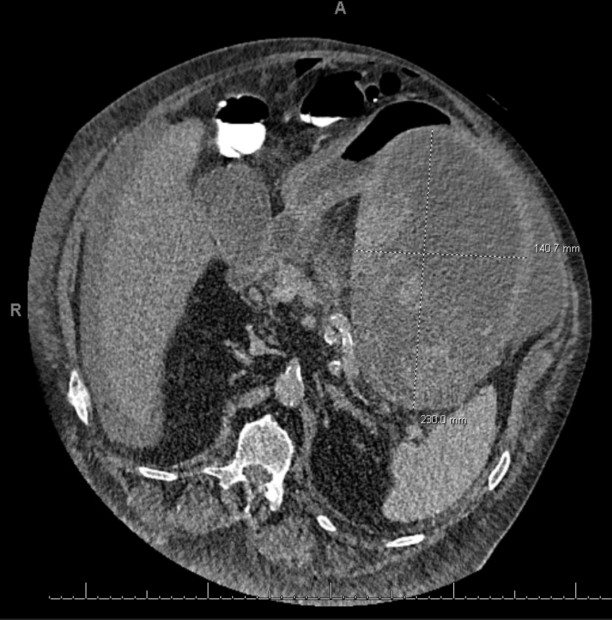
Figure: Image 1: Large necrotic collection adjacent to stomach wall.
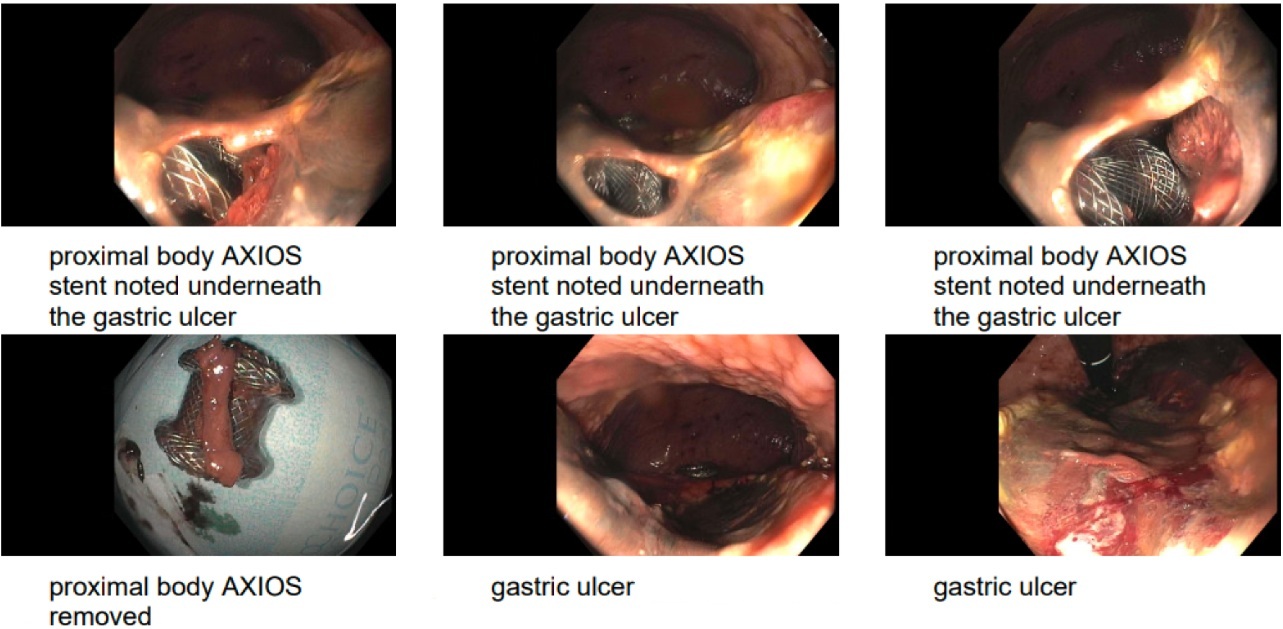
Figure: Image 2: Eroded gastric ulcer wall with full-length Axios stent visible during necrosectomy. The proximal body Axios stent is being removed following completion of debridement.
Disclosures:
Shriraj Patel indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Shriraj Patel, DO1, Pranav Patel, MD2, Harshit S. Khara, MD3, Bradley D. Confer, DO2. P0249 - The Impostor Within: Contained Gastric Perforation Mimicking Pancreatic Walled-Off Necrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2Geisinger Health System, Danville, PA; 3Geisinger Health System, Danville, NJ
Introduction: The Atlanta classification defines walled-off necrosis (WON) as a mature, encapsulated collection of necrotic tissue that develops at least four weeks after necrotizing pancreatitis. Although imaging and clinical context guide diagnosis, overlapping features may obscure alternative etiologies. We present a case of presumed early walled-off pancreatic necrosis (WOPN) that was instead a contained gastric ulcer perforation with rapid wall formation.
Case Description/
Methods: A 59-year-old obese male with history of alcohol use disorder and recurrent pancreatitis presented with sharp epigastric pain and a lipase >2000 U/L, consistent with acute pancreatitis. A computed tomography (CT) scan on hospital day two revealed an acute peripancreatic necrotic fluid collection without wall formation. For peritoneal signs on day three, repeat CT demonstrated interval enlargement of the peripancreatic fluid collection with early wall formation, presumed to be WOPN. Esophagogastroduodenoscopy (EGD) with endoscopic ultrasound (EUS) revealed a > 10 cm x 10 cm walled-off necrosis, drained via EUS-guided cystogastrostomy using two lumen-apposing metal stents in the proximal and distal gastric body (multiple transluminal gateway technique). A total of three necrosectomies were performed. During the second, a large gastric body ulcer was discovered. Given the ulcer’s proximity to the necrotic cavity with rapid wall formation within 13 days of pancreatitis, a contained gastric perforation was suspected to be the true etiology, not WOPN. The patient was ultimately discharged in stable condition to rehab with outpatient monitoring.
Discussion: This case illustrates the importance of challenging diagnostic assumptions. Given the history of alcohol use disorder, the patient’s fluid collection was initially attributed to his presentation with pancreatitis. However, the timeline was not consistent with typical WOPN. Radiographic and endoscopic findings concluded that the peripancreatic fluid collection was instead a result of a contained gastric ulcer perforation with rapid wall formation. The enlarging fluid collection was likely due to intraluminal hemorrhage with clot formation and necrotic cavity expansion adjacent to the stomach. This case underscores the risk of anchoring bias in pancreatic pathology and highlights the diagnostic value of endoscopy when imaging is non-specific. Early recognition of contained gastric perforation can guide timely intervention and avoid unnecessary or mistimed procedures.
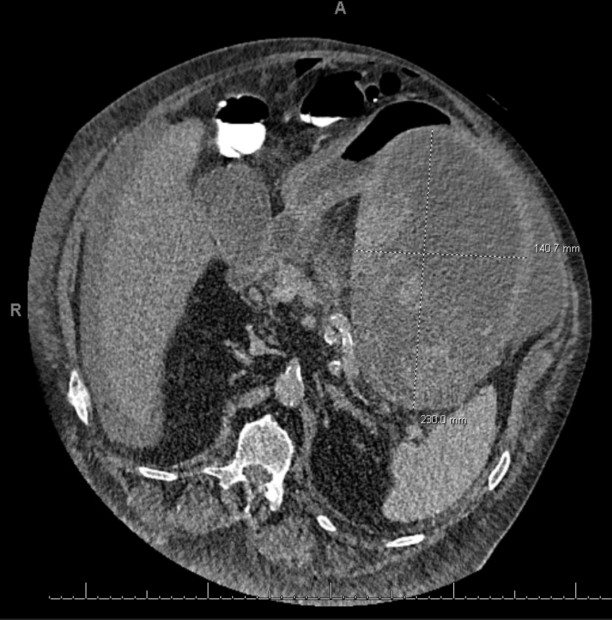
Figure: Image 1: Large necrotic collection adjacent to stomach wall.
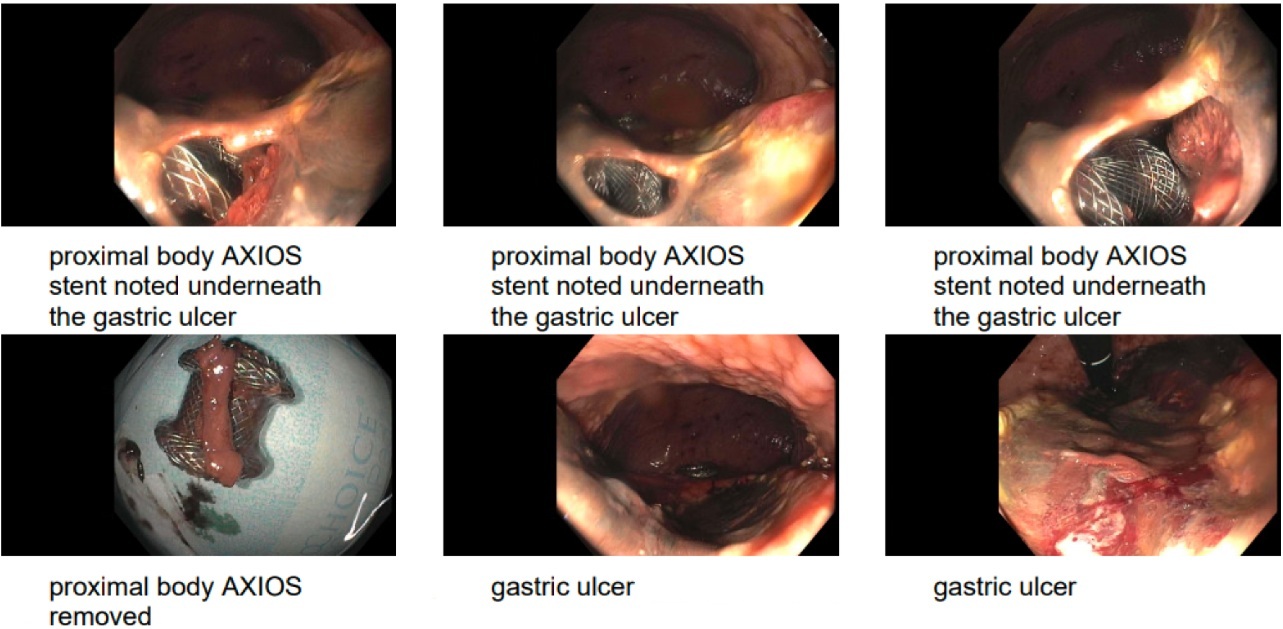
Figure: Image 2: Eroded gastric ulcer wall with full-length Axios stent visible during necrosectomy. The proximal body Axios stent is being removed following completion of debridement.
Disclosures:
Shriraj Patel indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Shriraj Patel, DO1, Pranav Patel, MD2, Harshit S. Khara, MD3, Bradley D. Confer, DO2. P0249 - The Impostor Within: Contained Gastric Perforation Mimicking Pancreatic Walled-Off Necrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
