Sunday Poster Session
Category: Biliary/Pancreas
P0203 - Vanishing Bile Duct Syndrome: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Davood K. Hosseini, MD
Hackensack University Medical Center
Hackensack, NJ
Presenting Author(s)
Davood Karimi Hosseini, MD1, Ethan Burg, MS1, Max Edeson, BA1, Gabrielle Sharbin, MS1, Lahari Kota, MD1, Katherine Panagos, MD1, Chinmay Trivedi, MD1, Colin Westman, DO1, Jose P. Garcia, MD2, Hanieh K. Hosseini, PharmD1, Shil Patel, DO1, Hongfa Zhu, MD1, Jonathan Weinberger, MD1, Shalom Frager, MD1, Rosario Ligresti, MD1
1Hackensack University Medical Center, Hackensack, NJ; 2Hackensack University Medical Center, Saddle River, NJ
Introduction: Vanishing bile duct syndrome (VBDS) is a rare, acquired form of cholestatic liver disease associated with hepatic ductopenia. Causes of VBDS include infections, autoimmune disease malignancy, idiopathic causes and drugs. Identifying the cause is essential for treatment. We present a case of suspected drug induced VBDS to increase awareness and discuss differential causes.
Case Description/
Methods: A 52 year old female with a history of hypertension (HTN), type I diabetes complicated by End Stage Renal Disease status post pancreatic (2007) and kidney transplant (2005) on azathioprine, presented with worsening fatigue and jaundice for 6-12 months. She endorsed weight loss, dyspnea and lower extremity (LE) edema. She denied abdominal pain or nausea/vomiting. She had rising leukocytosis over the past year with no clear source. Exam was significant for jaundice, scleral icterus, bilateral LE edema and rales. Labs showed significant leukocytosis, significantly elevated bilirubin (direct predominant) and alkaline phosphatase (ALP) with mild transaminemia.
Infectious and autoimmune work up of her cholestatic liver injury was negative. Imaging showed lithiasis with no ductal dilation or inflammation. She continued to deteriorate, developing worsening cholestasis and undifferentiated shock. Liver and bone marrow biopsies revealed 35-50% ductal loss consistent with VBDS and Myelodysplastic syndrome (MDS). She started minoxidil for HTN in March 2024, with her ALP rising by May. VBDS was suspected to be drug induced from minoxidil or azathioprine. Both were discontinued and ursodiol was initiated with mild improvement in ALP but worsening bilirubin. After a complex course, she passed away from cardiac arrest before recovery from VBDS could be appreciated.
Discussion: With a negative infectious and autoimmune workup, and no known association between MDS and VBDS, medication was the most likely cause. Minoxidil was considered due to its temporal association with rising ALP. Azathioprine is also associated with both acute cholestatic injury and chronic hepatotoxicity. Both drugs have rarely been linked to VBDS. ALP improvement following cessation of both medications and initiation of ursodiol supports our conclusion. Identifying the offending agent is difficult with multiple potential causes. Drug induced VBDS follows a variable clinical course. The only treatment is cessation of the offending agent and ursodiol. Our case highlights the diagnostic uncertainty of VBDS.
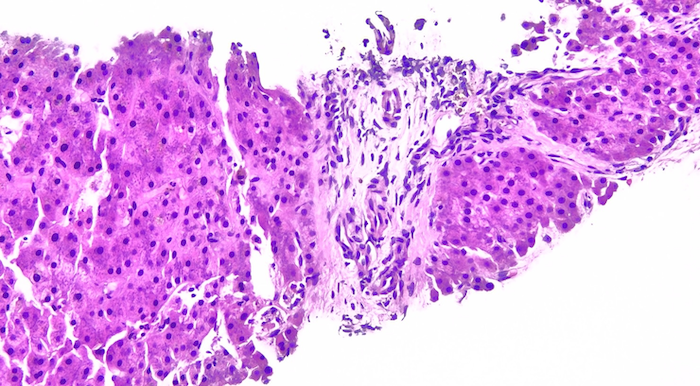
Figure: Figure 1: Liver Biopsy with Mild Ductopenia (H and E 200x)
Disclosures:
Davood Karimi Hosseini indicated no relevant financial relationships.
Ethan Burg indicated no relevant financial relationships.
Max Edeson indicated no relevant financial relationships.
Gabrielle Sharbin indicated no relevant financial relationships.
Lahari Kota indicated no relevant financial relationships.
Katherine Panagos indicated no relevant financial relationships.
Chinmay Trivedi indicated no relevant financial relationships.
Colin Westman indicated no relevant financial relationships.
Jose Garcia indicated no relevant financial relationships.
Hanieh K. Hosseini indicated no relevant financial relationships.
Shil Patel indicated no relevant financial relationships.
Hongfa Zhu indicated no relevant financial relationships.
Jonathan Weinberger indicated no relevant financial relationships.
Shalom Frager indicated no relevant financial relationships.
Rosario Ligresti indicated no relevant financial relationships.
Davood Karimi Hosseini, MD1, Ethan Burg, MS1, Max Edeson, BA1, Gabrielle Sharbin, MS1, Lahari Kota, MD1, Katherine Panagos, MD1, Chinmay Trivedi, MD1, Colin Westman, DO1, Jose P. Garcia, MD2, Hanieh K. Hosseini, PharmD1, Shil Patel, DO1, Hongfa Zhu, MD1, Jonathan Weinberger, MD1, Shalom Frager, MD1, Rosario Ligresti, MD1. P0203 - Vanishing Bile Duct Syndrome: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hackensack University Medical Center, Hackensack, NJ; 2Hackensack University Medical Center, Saddle River, NJ
Introduction: Vanishing bile duct syndrome (VBDS) is a rare, acquired form of cholestatic liver disease associated with hepatic ductopenia. Causes of VBDS include infections, autoimmune disease malignancy, idiopathic causes and drugs. Identifying the cause is essential for treatment. We present a case of suspected drug induced VBDS to increase awareness and discuss differential causes.
Case Description/
Methods: A 52 year old female with a history of hypertension (HTN), type I diabetes complicated by End Stage Renal Disease status post pancreatic (2007) and kidney transplant (2005) on azathioprine, presented with worsening fatigue and jaundice for 6-12 months. She endorsed weight loss, dyspnea and lower extremity (LE) edema. She denied abdominal pain or nausea/vomiting. She had rising leukocytosis over the past year with no clear source. Exam was significant for jaundice, scleral icterus, bilateral LE edema and rales. Labs showed significant leukocytosis, significantly elevated bilirubin (direct predominant) and alkaline phosphatase (ALP) with mild transaminemia.
Infectious and autoimmune work up of her cholestatic liver injury was negative. Imaging showed lithiasis with no ductal dilation or inflammation. She continued to deteriorate, developing worsening cholestasis and undifferentiated shock. Liver and bone marrow biopsies revealed 35-50% ductal loss consistent with VBDS and Myelodysplastic syndrome (MDS). She started minoxidil for HTN in March 2024, with her ALP rising by May. VBDS was suspected to be drug induced from minoxidil or azathioprine. Both were discontinued and ursodiol was initiated with mild improvement in ALP but worsening bilirubin. After a complex course, she passed away from cardiac arrest before recovery from VBDS could be appreciated.
Discussion: With a negative infectious and autoimmune workup, and no known association between MDS and VBDS, medication was the most likely cause. Minoxidil was considered due to its temporal association with rising ALP. Azathioprine is also associated with both acute cholestatic injury and chronic hepatotoxicity. Both drugs have rarely been linked to VBDS. ALP improvement following cessation of both medications and initiation of ursodiol supports our conclusion. Identifying the offending agent is difficult with multiple potential causes. Drug induced VBDS follows a variable clinical course. The only treatment is cessation of the offending agent and ursodiol. Our case highlights the diagnostic uncertainty of VBDS.
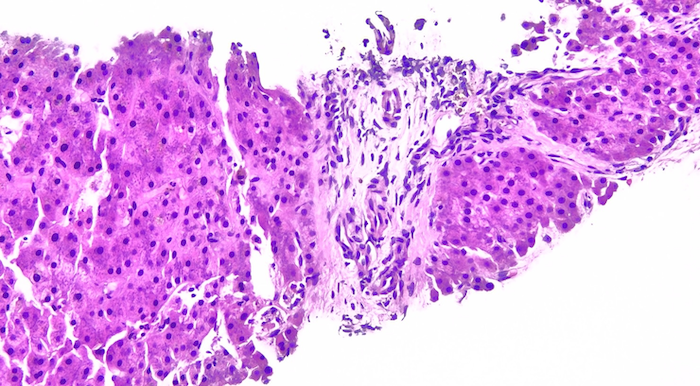
Figure: Figure 1: Liver Biopsy with Mild Ductopenia (H and E 200x)
Disclosures:
Davood Karimi Hosseini indicated no relevant financial relationships.
Ethan Burg indicated no relevant financial relationships.
Max Edeson indicated no relevant financial relationships.
Gabrielle Sharbin indicated no relevant financial relationships.
Lahari Kota indicated no relevant financial relationships.
Katherine Panagos indicated no relevant financial relationships.
Chinmay Trivedi indicated no relevant financial relationships.
Colin Westman indicated no relevant financial relationships.
Jose Garcia indicated no relevant financial relationships.
Hanieh K. Hosseini indicated no relevant financial relationships.
Shil Patel indicated no relevant financial relationships.
Hongfa Zhu indicated no relevant financial relationships.
Jonathan Weinberger indicated no relevant financial relationships.
Shalom Frager indicated no relevant financial relationships.
Rosario Ligresti indicated no relevant financial relationships.
Davood Karimi Hosseini, MD1, Ethan Burg, MS1, Max Edeson, BA1, Gabrielle Sharbin, MS1, Lahari Kota, MD1, Katherine Panagos, MD1, Chinmay Trivedi, MD1, Colin Westman, DO1, Jose P. Garcia, MD2, Hanieh K. Hosseini, PharmD1, Shil Patel, DO1, Hongfa Zhu, MD1, Jonathan Weinberger, MD1, Shalom Frager, MD1, Rosario Ligresti, MD1. P0203 - Vanishing Bile Duct Syndrome: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
