Sunday Poster Session
Category: Biliary/Pancreas
P0197 - Cardiac Tamponade: An Atypical Presentation of Type 1 Autoimmune Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Francisco Pascual, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Francisco Pascual, MD, Bhargav Kansara, BS, Romy Bareket, MD, Pushpak Taunk, MD
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Autoimmune pancreatitis (AIP) is a rare condition. Type 1 AIP is often associated with extra-pancreatic organ involvement, commonly the liver, bile ducts, salivary glands, and kidneys. Herein, we present a unique case of Type 1 AIP, with an initial presentation of cardiac tamponade.
Case Description/
Methods: A 46-year-old Haitian male presented to the hospital with one week of cough, chest pain, and intermittent syncope. On admission, he was febrile and tachycardic, but otherwise, physical exam was unremarkable. His EKG demonstrated inferior ST segment elevations, and subsequent echocardiogram displayed a large pericardial effusion with tamponade physiology, requiring emergent pericardiocentesis. Ischemic cardiac evaluation was negative. Pericardial fluid studies revealed an exudative effusion, prompting a broad infectious workup. While there was concern for Mycobacterium tuberculosis (TB) infection, given that he was from an endemic area, TB pericardial fluid PCR testing was negative. A CT abdomen and pelvis was obtained and revealed a hypo-enhancing pancreatic body lesion encasing the main portal vein and celiac trifurcation. Follow-up MRI was notable for decreased pancreatic body and tail T1 signal and a large area of decreased enhancement in the body with focal loss of normal acinar parenchyma. There was also evidence of peripancreatic and intrapancreatic edematous changes, as well as poorly organized peripancreatic fluid with normal-caliber ducts. Further serologic testing revealed elevated serum IgG4 of 353.4 mg/dL. EUS with FNB was performed, demonstrating diffuse echogenicity, hyperechoic strands, hyperechoic foci, and shadowing foci. FNB pathology displayed fibrotic pancreatic tissue with up to 7 IgG4/CD183+ plasma cells and no evidence of malignancy. Given the high likelihood of AIP, he was referred to our pancreatic specialist to consider steroid therapy.
Discussion: AIP can be challenging to diagnose; traditionally, patients present with clinical features of abdominal pain, unexplained weight loss, elevated liver tests, or evidence of biliary obstruction. However, confirmatory diagnosis requires supporting evidence on imaging, serological testing, histology, and secondary organ involvement. While pericardial manifestations have been reported with IgG4-related disease, this case highlights a unique, atypical presentation in that the etiology of the cardiac tamponade was only elucidated after imaging, serology, and biopsy of the pancreas supported AIP.
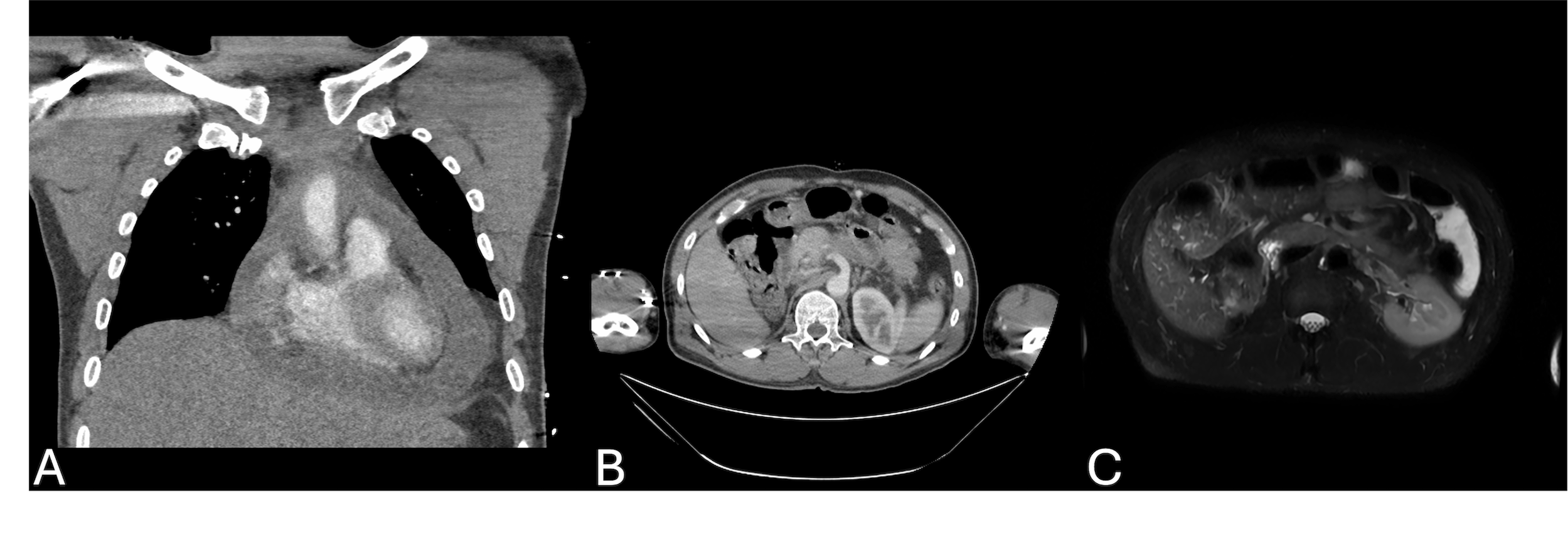
Figure: Figure 1.
A. CT angiography of the chest displaying a large pericardial effusion.
B. CT abdomen image of pancreatic body lesion.
C. MRI T2-weighted fat-suppressed breath-hold image of pancreatic mass.
Disclosures:
Francisco Pascual indicated no relevant financial relationships.
Bhargav Kansara indicated no relevant financial relationships.
Romy Bareket indicated no relevant financial relationships.
Pushpak Taunk: Boston Scientific – Consultant. Endo Therapeutics – Consultant. Neptune Medical – Consultant.
Francisco Pascual, MD, Bhargav Kansara, BS, Romy Bareket, MD, Pushpak Taunk, MD. P0197 - Cardiac Tamponade: An Atypical Presentation of Type 1 Autoimmune Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Autoimmune pancreatitis (AIP) is a rare condition. Type 1 AIP is often associated with extra-pancreatic organ involvement, commonly the liver, bile ducts, salivary glands, and kidneys. Herein, we present a unique case of Type 1 AIP, with an initial presentation of cardiac tamponade.
Case Description/
Methods: A 46-year-old Haitian male presented to the hospital with one week of cough, chest pain, and intermittent syncope. On admission, he was febrile and tachycardic, but otherwise, physical exam was unremarkable. His EKG demonstrated inferior ST segment elevations, and subsequent echocardiogram displayed a large pericardial effusion with tamponade physiology, requiring emergent pericardiocentesis. Ischemic cardiac evaluation was negative. Pericardial fluid studies revealed an exudative effusion, prompting a broad infectious workup. While there was concern for Mycobacterium tuberculosis (TB) infection, given that he was from an endemic area, TB pericardial fluid PCR testing was negative. A CT abdomen and pelvis was obtained and revealed a hypo-enhancing pancreatic body lesion encasing the main portal vein and celiac trifurcation. Follow-up MRI was notable for decreased pancreatic body and tail T1 signal and a large area of decreased enhancement in the body with focal loss of normal acinar parenchyma. There was also evidence of peripancreatic and intrapancreatic edematous changes, as well as poorly organized peripancreatic fluid with normal-caliber ducts. Further serologic testing revealed elevated serum IgG4 of 353.4 mg/dL. EUS with FNB was performed, demonstrating diffuse echogenicity, hyperechoic strands, hyperechoic foci, and shadowing foci. FNB pathology displayed fibrotic pancreatic tissue with up to 7 IgG4/CD183+ plasma cells and no evidence of malignancy. Given the high likelihood of AIP, he was referred to our pancreatic specialist to consider steroid therapy.
Discussion: AIP can be challenging to diagnose; traditionally, patients present with clinical features of abdominal pain, unexplained weight loss, elevated liver tests, or evidence of biliary obstruction. However, confirmatory diagnosis requires supporting evidence on imaging, serological testing, histology, and secondary organ involvement. While pericardial manifestations have been reported with IgG4-related disease, this case highlights a unique, atypical presentation in that the etiology of the cardiac tamponade was only elucidated after imaging, serology, and biopsy of the pancreas supported AIP.
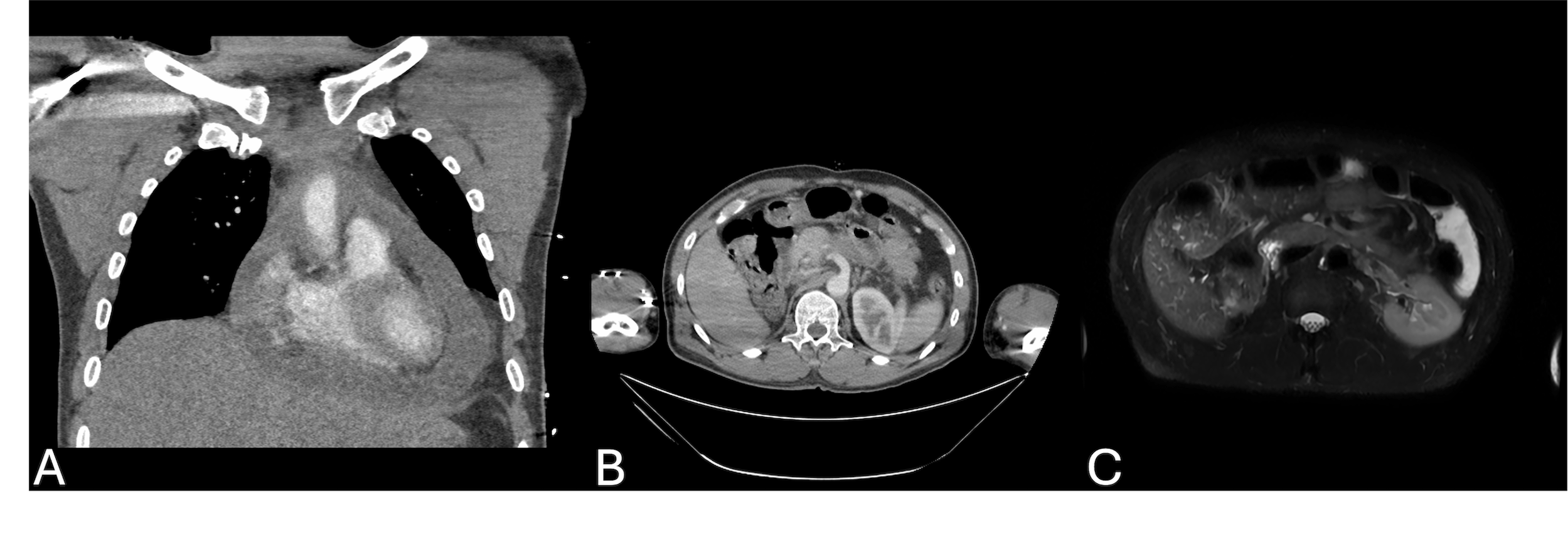
Figure: Figure 1.
A. CT angiography of the chest displaying a large pericardial effusion.
B. CT abdomen image of pancreatic body lesion.
C. MRI T2-weighted fat-suppressed breath-hold image of pancreatic mass.
Disclosures:
Francisco Pascual indicated no relevant financial relationships.
Bhargav Kansara indicated no relevant financial relationships.
Romy Bareket indicated no relevant financial relationships.
Pushpak Taunk: Boston Scientific – Consultant. Endo Therapeutics – Consultant. Neptune Medical – Consultant.
Francisco Pascual, MD, Bhargav Kansara, BS, Romy Bareket, MD, Pushpak Taunk, MD. P0197 - Cardiac Tamponade: An Atypical Presentation of Type 1 Autoimmune Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
