Sunday Poster Session
Category: Biliary/Pancreas
P0194 - Cavernous Transformation and Variceal Bleeding Following Portal Vein Thrombosis in Necrotizing Pancreatitis: A Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SH
Shahd Hazim, DO
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Shahd Hazim, DO, Abdullah Khalid, MD, Ebubekir Daglilar, MD, Nisar Amin, MD
Charleston Area Medical Center, Charleston, WV
Introduction: Non-cirrhotic, non-malignant portal vein thrombosis (PVT) is thrombus formation within the portal vein or its intra-hepatic branches without cirrhosis or malignancy. Although rare, about one third of cases are associated with inflammatory conditions, like pancreatitis. Complications of PVT include cavernous transformation and portal hypertension. Management of these complications is challenging and depends on multiple factors, especially considering the increased bleeding risk in these patients. A combination of medical, endovascular, and endoscopic interventions is often required. This case highlights the importance of imaging and clinical context in guiding management decisions for a patient with cavernous transformation and portal hypertension.
Case Description/
Methods: A 55-year-old male presented with gallstone-associated pancreatitis. During the initial admission, he developed necrotizing pancreatitis and had cholecystectomy. He was readmitted two months later for recurrent necrotizing pancreatitis requiring peripancreatic drainage and necrosectomy. Imaging during this admission showed an incidental PVT, and he was started on an anticoagulant. He returned one month later with signs of peripancreatic infection and gastrointestinal bleeding. Imaging showed cavernous transformation of the portal vein, and anticoagulation was discontinued due to bleeding concerns. Approximately nine months after initial presentation, the patient presented with esophageal variceal bleeding which necessitated band ligation. He experienced another episode of variceal bleeding 30 months after the initial PVT diagnosis and was again treated with endoscopic therapy.
Discussion: A key complication of necrotizing pancreatitis is non-cirrhotic, non-malignant PVT, which may progress to cavernous transformation and portal hypertension. Timely anticoagulation is often necessary but needs to be weighed against the risk of bleeding in such patients. If thrombosis persists, interventional techniques like TIPS may be needed to reduce the risk of portal hypertension and variceal bleeding. Routine endoscopic and imaging surveillance can be invaluable in these patients. The presented case demonstrated the complexities of clinical decision making for patients with cavernous transformation and portal hypertension and highlights the importance of a tailored approach to management.
Willington AJ,et al. Current concepts in the management of non-cirrhotic non-malignant portal vein thrombosis. World J Hepatol. 2024 May 27;16(5):751-765
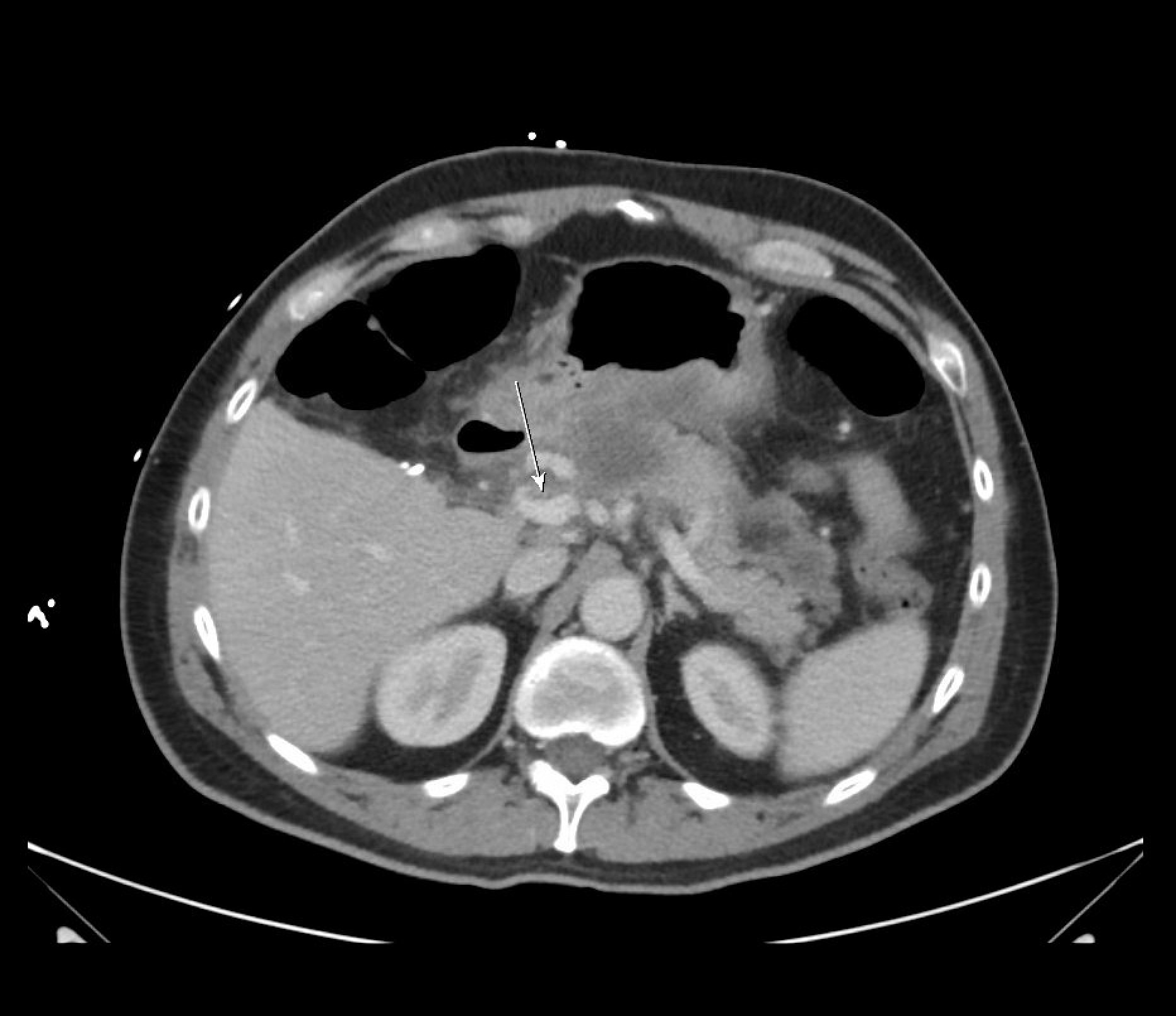
Figure: Contrast-enhanced CT of the abdomen (portal venous phase) showing an incidental non-occlusive thrombus within the portal vein.

Figure: Repeat contrast-enhanced CT of the abdomen during readmission showing cavernous transformation, with new collateral vessels replacing the thrombosed portal vein.
Disclosures:
Shahd Hazim indicated no relevant financial relationships.
Abdullah Khalid indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Shahd Hazim, DO, Abdullah Khalid, MD, Ebubekir Daglilar, MD, Nisar Amin, MD. P0194 - Cavernous Transformation and Variceal Bleeding Following Portal Vein Thrombosis in Necrotizing Pancreatitis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Charleston Area Medical Center, Charleston, WV
Introduction: Non-cirrhotic, non-malignant portal vein thrombosis (PVT) is thrombus formation within the portal vein or its intra-hepatic branches without cirrhosis or malignancy. Although rare, about one third of cases are associated with inflammatory conditions, like pancreatitis. Complications of PVT include cavernous transformation and portal hypertension. Management of these complications is challenging and depends on multiple factors, especially considering the increased bleeding risk in these patients. A combination of medical, endovascular, and endoscopic interventions is often required. This case highlights the importance of imaging and clinical context in guiding management decisions for a patient with cavernous transformation and portal hypertension.
Case Description/
Methods: A 55-year-old male presented with gallstone-associated pancreatitis. During the initial admission, he developed necrotizing pancreatitis and had cholecystectomy. He was readmitted two months later for recurrent necrotizing pancreatitis requiring peripancreatic drainage and necrosectomy. Imaging during this admission showed an incidental PVT, and he was started on an anticoagulant. He returned one month later with signs of peripancreatic infection and gastrointestinal bleeding. Imaging showed cavernous transformation of the portal vein, and anticoagulation was discontinued due to bleeding concerns. Approximately nine months after initial presentation, the patient presented with esophageal variceal bleeding which necessitated band ligation. He experienced another episode of variceal bleeding 30 months after the initial PVT diagnosis and was again treated with endoscopic therapy.
Discussion: A key complication of necrotizing pancreatitis is non-cirrhotic, non-malignant PVT, which may progress to cavernous transformation and portal hypertension. Timely anticoagulation is often necessary but needs to be weighed against the risk of bleeding in such patients. If thrombosis persists, interventional techniques like TIPS may be needed to reduce the risk of portal hypertension and variceal bleeding. Routine endoscopic and imaging surveillance can be invaluable in these patients. The presented case demonstrated the complexities of clinical decision making for patients with cavernous transformation and portal hypertension and highlights the importance of a tailored approach to management.
Willington AJ,et al. Current concepts in the management of non-cirrhotic non-malignant portal vein thrombosis. World J Hepatol. 2024 May 27;16(5):751-765
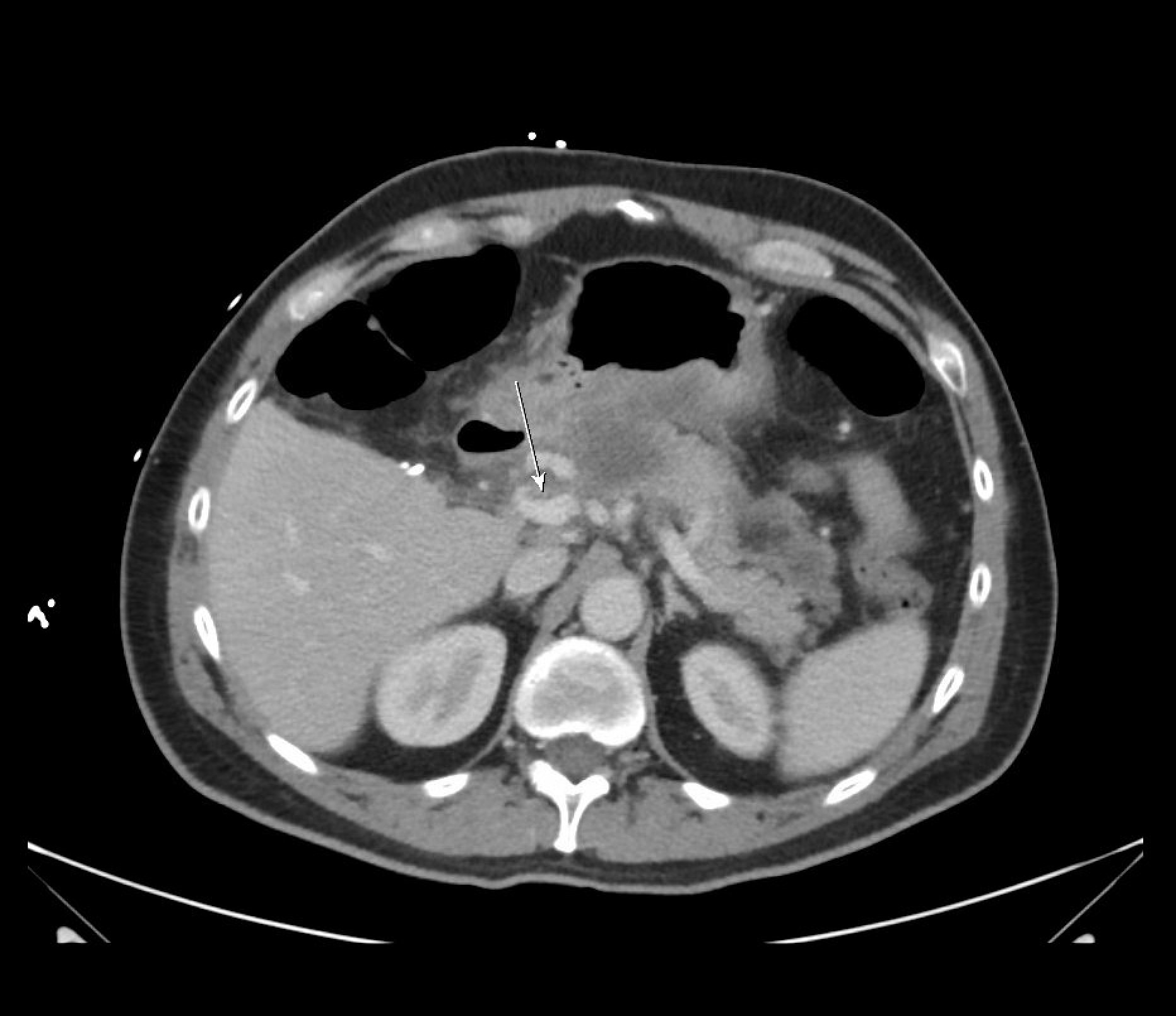
Figure: Contrast-enhanced CT of the abdomen (portal venous phase) showing an incidental non-occlusive thrombus within the portal vein.

Figure: Repeat contrast-enhanced CT of the abdomen during readmission showing cavernous transformation, with new collateral vessels replacing the thrombosed portal vein.
Disclosures:
Shahd Hazim indicated no relevant financial relationships.
Abdullah Khalid indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Shahd Hazim, DO, Abdullah Khalid, MD, Ebubekir Daglilar, MD, Nisar Amin, MD. P0194 - Cavernous Transformation and Variceal Bleeding Following Portal Vein Thrombosis in Necrotizing Pancreatitis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
