Sunday Poster Session
Category: Biliary/Pancreas
P0193 - Endoscopic Findings of Minor and Major Papillitis in a Patient With Relapsing Pancreatitis: Is It Pancreas Divisum?
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed K. Osman, MD, MPH
NYC Health + Hospitals/Harlem
New York, NY
Presenting Author(s)
Mohamed K.. Osman, MD, MPH1, Esteban Verduzco, MD, MMSc1, Thin Phyu Phyu. Aung, MD2, Joan A.. Culpepper-Morgan, MD, FACG2
1NYC Health + Hospitals/Harlem, New York, NY; 2NYC Health + Hospitals, New York, NY
Introduction: Pancreas divisum (PDiv) is a prevalent (7-18%) congenital variant of the pancreatico-biliary duct junction, but a rare cause of acute pancreatitis. Failure of the main pancreatic duct to fuse with the accessory duct during embryogenesis leads to dual openings for the pancreatic duct (PD) and the common bile duct (CBD) into duodenum. Most patients are asymptomatic with incidental diagnosis. Endoscopic findings of the duodenum showing PDiv during an acute pancreatitis flare are uncommon in the literature. We present such findings due to a flare of pancreatitis that occurred in hospital.
Case Description/
Methods: A 63-year-old man with type 2 diabetes presented with two-months of RUQ pain, anorexia, and 17 lbs weight loss. Pain was moderate, burning, non-radiating, unrelated to food, and better supine. He denied fever, nausea, vomiting, diarrhea, constipation, melena and hematochezia. Pain had been chronic for several years though milder. He denied alcohol. Prior EGD showed H. pylori, but he never completed treatment. Worsening pain led to monthly ED visits over the last year. On this visit, he also complained of dry cough, which prompted CT chest, abdomen, and pelvis. The CT was indeterminate for PE and showed a normal pancreas. He had epigastric and RUQ tenderness. Lipase was normal at 39 U/L. CBC showed a left shift. BUN was 21 and lactate elevated to 5.6. LFTs and lipase were normal. D-dimer was elevated at 972. Ultrasound showed no stones and a 5 mm CBD. On day 3, due to continued concern for PE, a repeat CT-angio ruled out PE, but showed new fat stranding and free fluid around the pancreas. Lipase was now 1101. LFTs remained normal and triglycerides 133. CBC was normal, except for 9.2% eosinophils. Given a concern for penetrating ulcer and untreated H pylori, EGD was done showing no ulcer but greatly engorged minor and major papillae or dual papillitis (fig 1). MRCP showed a separate entrance to the duodenum for CBD and PD consistent with PDiv type I (fig. 2). He received fluids and analgesics. Despite negative H pylori histology, he received quadruple therapy to ensure eradication. By day 13, he was discharged but lost to follow up.
Discussion: Up to 30% of PDiv patients experience recurrent pancreatitis. Edema of the papilla may result from infection, stones, or tumors causing pancreatitis. Observing dual papillitis with pancreatitis implies PDiv. This patient would likely benefit from minor papilla stenting.
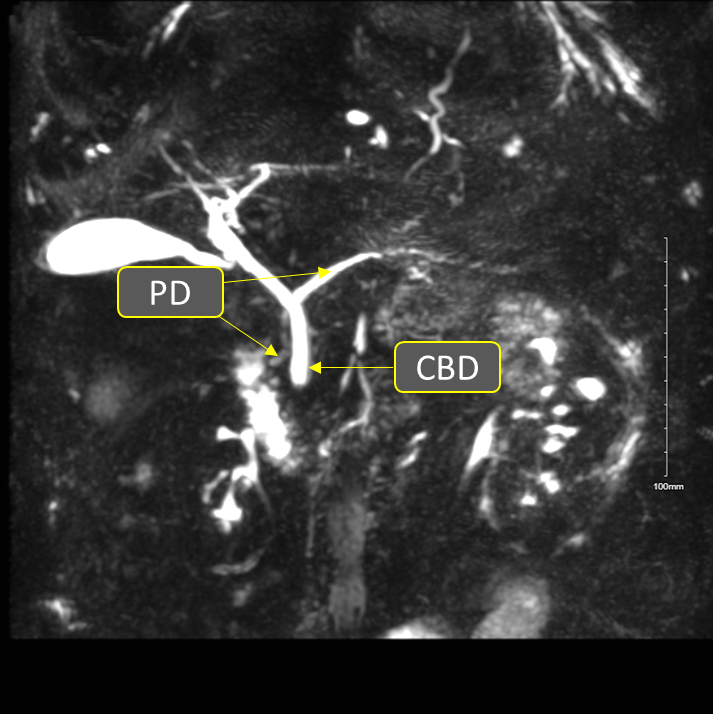
Figure: Figure 1. Dual papillitis with engorged major papilla (arrow) and minor papilla (2 arrows)
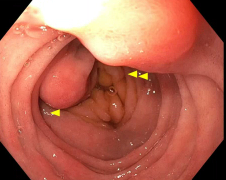
Figure: Figure 2. MRCP showing separate entrance of CBD and PD into duodenum
Disclosures:
Mohamed Osman indicated no relevant financial relationships.
Esteban Verduzco indicated no relevant financial relationships.
Thin Aung indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Mohamed K.. Osman, MD, MPH1, Esteban Verduzco, MD, MMSc1, Thin Phyu Phyu. Aung, MD2, Joan A.. Culpepper-Morgan, MD, FACG2. P0193 - Endoscopic Findings of Minor and Major Papillitis in a Patient With Relapsing Pancreatitis: Is It Pancreas Divisum?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Harlem, New York, NY; 2NYC Health + Hospitals, New York, NY
Introduction: Pancreas divisum (PDiv) is a prevalent (7-18%) congenital variant of the pancreatico-biliary duct junction, but a rare cause of acute pancreatitis. Failure of the main pancreatic duct to fuse with the accessory duct during embryogenesis leads to dual openings for the pancreatic duct (PD) and the common bile duct (CBD) into duodenum. Most patients are asymptomatic with incidental diagnosis. Endoscopic findings of the duodenum showing PDiv during an acute pancreatitis flare are uncommon in the literature. We present such findings due to a flare of pancreatitis that occurred in hospital.
Case Description/
Methods: A 63-year-old man with type 2 diabetes presented with two-months of RUQ pain, anorexia, and 17 lbs weight loss. Pain was moderate, burning, non-radiating, unrelated to food, and better supine. He denied fever, nausea, vomiting, diarrhea, constipation, melena and hematochezia. Pain had been chronic for several years though milder. He denied alcohol. Prior EGD showed H. pylori, but he never completed treatment. Worsening pain led to monthly ED visits over the last year. On this visit, he also complained of dry cough, which prompted CT chest, abdomen, and pelvis. The CT was indeterminate for PE and showed a normal pancreas. He had epigastric and RUQ tenderness. Lipase was normal at 39 U/L. CBC showed a left shift. BUN was 21 and lactate elevated to 5.6. LFTs and lipase were normal. D-dimer was elevated at 972. Ultrasound showed no stones and a 5 mm CBD. On day 3, due to continued concern for PE, a repeat CT-angio ruled out PE, but showed new fat stranding and free fluid around the pancreas. Lipase was now 1101. LFTs remained normal and triglycerides 133. CBC was normal, except for 9.2% eosinophils. Given a concern for penetrating ulcer and untreated H pylori, EGD was done showing no ulcer but greatly engorged minor and major papillae or dual papillitis (fig 1). MRCP showed a separate entrance to the duodenum for CBD and PD consistent with PDiv type I (fig. 2). He received fluids and analgesics. Despite negative H pylori histology, he received quadruple therapy to ensure eradication. By day 13, he was discharged but lost to follow up.
Discussion: Up to 30% of PDiv patients experience recurrent pancreatitis. Edema of the papilla may result from infection, stones, or tumors causing pancreatitis. Observing dual papillitis with pancreatitis implies PDiv. This patient would likely benefit from minor papilla stenting.
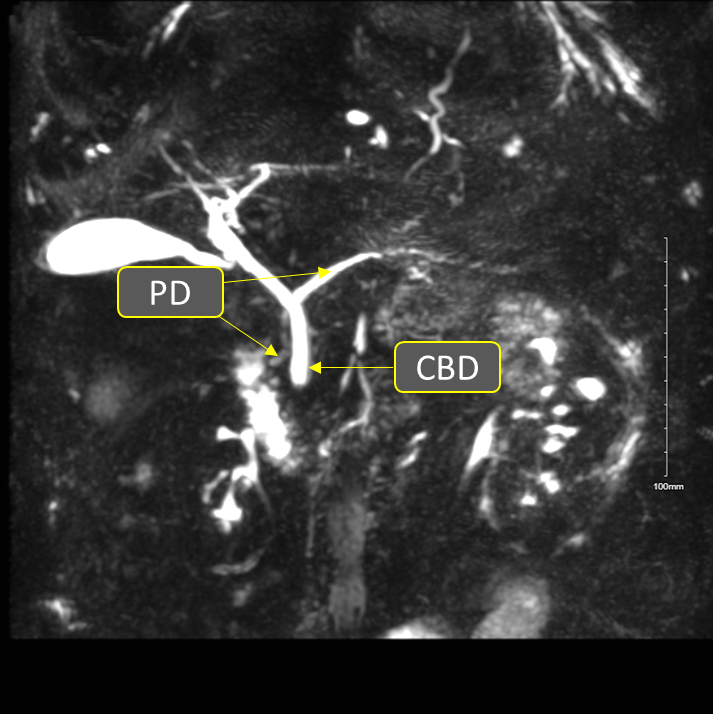
Figure: Figure 1. Dual papillitis with engorged major papilla (arrow) and minor papilla (2 arrows)
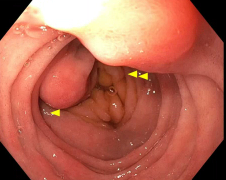
Figure: Figure 2. MRCP showing separate entrance of CBD and PD into duodenum
Disclosures:
Mohamed Osman indicated no relevant financial relationships.
Esteban Verduzco indicated no relevant financial relationships.
Thin Aung indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Mohamed K.. Osman, MD, MPH1, Esteban Verduzco, MD, MMSc1, Thin Phyu Phyu. Aung, MD2, Joan A.. Culpepper-Morgan, MD, FACG2. P0193 - Endoscopic Findings of Minor and Major Papillitis in a Patient With Relapsing Pancreatitis: Is It Pancreas Divisum?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
