Sunday Poster Session
Category: Biliary/Pancreas
P0191 - A Large G2 PanNET with Delayed Metastasis and MEN1 Mutation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Adam Khalaf, MD (he/him/his)
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Adam Khalaf, MD, Alessandra Martorella, DO, Ade Waterman, MBChB, Lavannya Atri, MD, Walid Chalhoub, MD
MedStar Georgetown University Hospital, Washington, DC
Introduction: Pancreatic neuroendocrine tumors (PanNETs) account for less than 3% of pancreatic neoplasms, with an incidence of 0.8 per 100,000, and 15% being functional. They are classified based on proliferation by the Ki-67 index and mitotic count. Grade 2 (G2) tumors (Ki-67 3-20%) comprise up to 30% of PanNETs. While prognosis varies, G2 PanNETs carry a significant metastatic risk of up to 60% at diagnosis. Current risk stratification relies on histologic grade (WHO) and TNM staging (AJCC), but tumor size, while included in staging, is not considered in grading or prognostic models. We report a case of a large G2 PanNET that appeared localized but developed rapid metastatic progression within one month, ultimately revealing an underlying MEN1 mutation.
Case Description/
Methods: A 66-year-old man presented with fever, vomiting, and diarrhea; CT imaging revealed a 9.8x7.2 cm isoattenuating mass in the body and tail of the pancreas (Figure 1). No hepatic lesions or distant metastases were present on follow-up staging. Endoscopic ultrasound confirmed a large heterogeneous pancreatic mass (Figure 2). Fine-needle biopsy revealed a well-differentiated Grade 2 NET (Ki-67: 5-10%). Serum chromogranin A (SCgA) was 288 ng/mL. The patient was scheduled for resection. Approximately 1 month later, a PET scan revealed new multifocal tracer-avid lesions in the liver and a hypodense nodule in the right thyroid lobe. Liver MRI confirmed at least 15 bilobar hepatic metastases (largest 1.4 cm) and splenic vein invasion. SCgA had risen to 625 ng/mL. Surgery was canceled, and the patient was initiated on octreotide therapy. Thyroid ultrasound showed a suspicious right lobe nodule. Genomic profiling of the tumor later revealed a MEN1 mutation with a variant allele frequency of 65%, prompting consideration of de novo MEN1 syndrome.
Discussion: G2 PanNETs can be subclassified into G2a (Ki-67 3–10%), associated with a 30% metastatic risk and usually measuring 1.3–5 cm. Solitary PanNETs in MEN1 patients are rare (< 13%) but tend to be larger ( >2 cm) and nonfunctional, increasing the risk of metastasis. Tumor size remains the most significant risk factor for liver metastases in MEN1-associated PanNETs; however, this nuance is not reflected in current risk stratification or grading systems. In this patient with no prior medical history, a large solitary G2a PanNET with rapid progression and MEN1 mutation highlights the need for integrating tumor size and genetic profiling into individualized risk assessment and staging strategies.
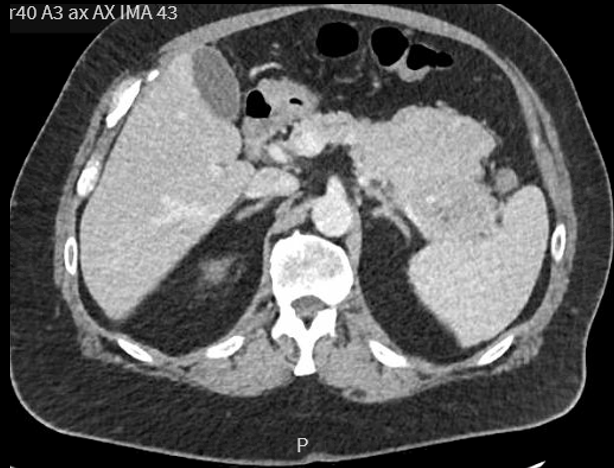
Figure: Figure 1: Axial contrast-enhanced CT image showing a large, heterogeneous soft tissue mass involving the body and tail of the pancreas, displacing adjacent structures and abutting the splenic vein. No hepatic lesions are visualized

Figure: Figure 2: Endoscopic Ultrasound demonstrating a well-circumscribed, hypoechoic mass in the pancreatic tail, consistent with a large neuroendocrine tumor inferior to the pancreatic duct. Fine-needle biopsy confirmed a well-differentiated Grade 2 tumor with a Ki-67 index of 5–10%.
Disclosures:
Adam Khalaf indicated no relevant financial relationships.
Alessandra Martorella indicated no relevant financial relationships.
Ade Waterman indicated no relevant financial relationships.
Lavannya Atri indicated no relevant financial relationships.
Walid Chalhoub indicated no relevant financial relationships.
Adam Khalaf, MD, Alessandra Martorella, DO, Ade Waterman, MBChB, Lavannya Atri, MD, Walid Chalhoub, MD. P0191 - A Large G2 PanNET with Delayed Metastasis and MEN1 Mutation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
MedStar Georgetown University Hospital, Washington, DC
Introduction: Pancreatic neuroendocrine tumors (PanNETs) account for less than 3% of pancreatic neoplasms, with an incidence of 0.8 per 100,000, and 15% being functional. They are classified based on proliferation by the Ki-67 index and mitotic count. Grade 2 (G2) tumors (Ki-67 3-20%) comprise up to 30% of PanNETs. While prognosis varies, G2 PanNETs carry a significant metastatic risk of up to 60% at diagnosis. Current risk stratification relies on histologic grade (WHO) and TNM staging (AJCC), but tumor size, while included in staging, is not considered in grading or prognostic models. We report a case of a large G2 PanNET that appeared localized but developed rapid metastatic progression within one month, ultimately revealing an underlying MEN1 mutation.
Case Description/
Methods: A 66-year-old man presented with fever, vomiting, and diarrhea; CT imaging revealed a 9.8x7.2 cm isoattenuating mass in the body and tail of the pancreas (Figure 1). No hepatic lesions or distant metastases were present on follow-up staging. Endoscopic ultrasound confirmed a large heterogeneous pancreatic mass (Figure 2). Fine-needle biopsy revealed a well-differentiated Grade 2 NET (Ki-67: 5-10%). Serum chromogranin A (SCgA) was 288 ng/mL. The patient was scheduled for resection. Approximately 1 month later, a PET scan revealed new multifocal tracer-avid lesions in the liver and a hypodense nodule in the right thyroid lobe. Liver MRI confirmed at least 15 bilobar hepatic metastases (largest 1.4 cm) and splenic vein invasion. SCgA had risen to 625 ng/mL. Surgery was canceled, and the patient was initiated on octreotide therapy. Thyroid ultrasound showed a suspicious right lobe nodule. Genomic profiling of the tumor later revealed a MEN1 mutation with a variant allele frequency of 65%, prompting consideration of de novo MEN1 syndrome.
Discussion: G2 PanNETs can be subclassified into G2a (Ki-67 3–10%), associated with a 30% metastatic risk and usually measuring 1.3–5 cm. Solitary PanNETs in MEN1 patients are rare (< 13%) but tend to be larger ( >2 cm) and nonfunctional, increasing the risk of metastasis. Tumor size remains the most significant risk factor for liver metastases in MEN1-associated PanNETs; however, this nuance is not reflected in current risk stratification or grading systems. In this patient with no prior medical history, a large solitary G2a PanNET with rapid progression and MEN1 mutation highlights the need for integrating tumor size and genetic profiling into individualized risk assessment and staging strategies.
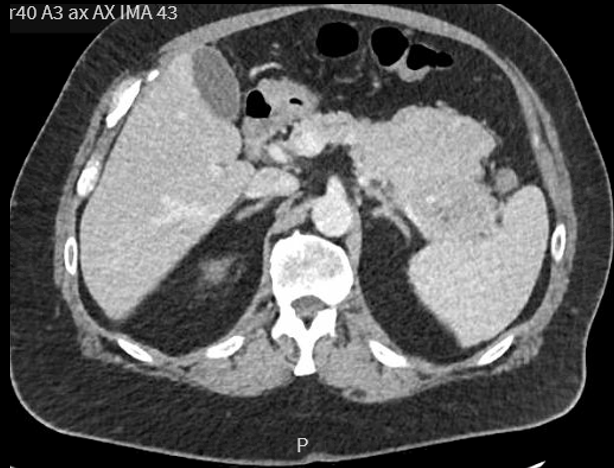
Figure: Figure 1: Axial contrast-enhanced CT image showing a large, heterogeneous soft tissue mass involving the body and tail of the pancreas, displacing adjacent structures and abutting the splenic vein. No hepatic lesions are visualized

Figure: Figure 2: Endoscopic Ultrasound demonstrating a well-circumscribed, hypoechoic mass in the pancreatic tail, consistent with a large neuroendocrine tumor inferior to the pancreatic duct. Fine-needle biopsy confirmed a well-differentiated Grade 2 tumor with a Ki-67 index of 5–10%.
Disclosures:
Adam Khalaf indicated no relevant financial relationships.
Alessandra Martorella indicated no relevant financial relationships.
Ade Waterman indicated no relevant financial relationships.
Lavannya Atri indicated no relevant financial relationships.
Walid Chalhoub indicated no relevant financial relationships.
Adam Khalaf, MD, Alessandra Martorella, DO, Ade Waterman, MBChB, Lavannya Atri, MD, Walid Chalhoub, MD. P0191 - A Large G2 PanNET with Delayed Metastasis and MEN1 Mutation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
