Sunday Poster Session
Category: Biliary/Pancreas
P0182 - Pancreatic NET in a Patient With NF1: Diagnostic Challenges and Long-Term Management
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Bianca Thakkar, DO
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Bianca Thakkar, DO1, Teresa Da Cunha, MD2, Steven Goldenberg, MD1
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health, Hartford, CT
Introduction: Neurofibromatosis type 1 (NF1) is an autosomal dominant disorder predisposing to a spectrum of gastrointestinal neoplasms, including periampullary and pancreatic neuroendocrine tumors (NETs). While duodenal and periampullary NETs are more common in NF1, pancreatic NETs are rare but clinically significant, often presenting with nonspecific symptoms or incidentally during evaluation for abnormal liver function tests. The risk of multifocal and synchronous tumors in NF1 necessitates a high index of suspicion and comprehensive evaluation.
Case Description/
Methods: A 50-year-old man with NF1, epilepsy, and a history of a well-differentiated pancreatic NET presented with elevated liver enzymes. Magnetic resonance cholangiopancreatography (MRCP) showed mild intrahepatic and extrahepatic biliary dilatation. Follow-up abdominal MRI revealed no additional findings. Endoscopic retrograde cholangiopancreatography (ERCP) identified a 3 cm mass at the major papilla with biliary stricture; biopsy confirmed a well-differentiated NET. He underwent a Whipple procedure, which revealed a 2.5 cm well-differentiated NET without metastases. PET imaging was negative for distant disease. Postoperatively, the patient was monitored with clinical follow-up every 6–12 months and annual imaging.
Six years later, a positive Cologuard test prompted colonoscopy, which identified and removed three polyps: a 12 mm polyp in the descending colon, a 9 mm polyp in the proximal sigmoid, and a 20 mm polyp in the distal sigmoid. Pathology confirmed benign adenomas. An upper endoscopy was performed to evaluate for additional NETs or gastrointestinal stromal tumors (GISTs) and was unremarkable.
Discussion: Patients with NF1 are at increased risk for gastrointestinal NETs, including rare pancreatic NETs, which may arise independently or synchronously with other tumors. Current guidelines recommend surgical resection for well-differentiated periampullary or pancreatic NETs >2 cm or with local invasion, as in this case. In NF1, a Whipple procedure is preferred due to higher risk of nodal involvement and multifocal disease. Long-term surveillance is crucial, given the potential for late recurrence and new primary tumors. This case underscores the importance of multidisciplinary management and vigilant follow-up in NF1 patients with gastrointestinal neoplasms.
References:
1.Katzka DA, Pandolfino JE, Kahrilas PJ. Gastroenterology, January 2013; 144(1): 27–38. Phenotypes of achalasia: beyond the Chicago classification.
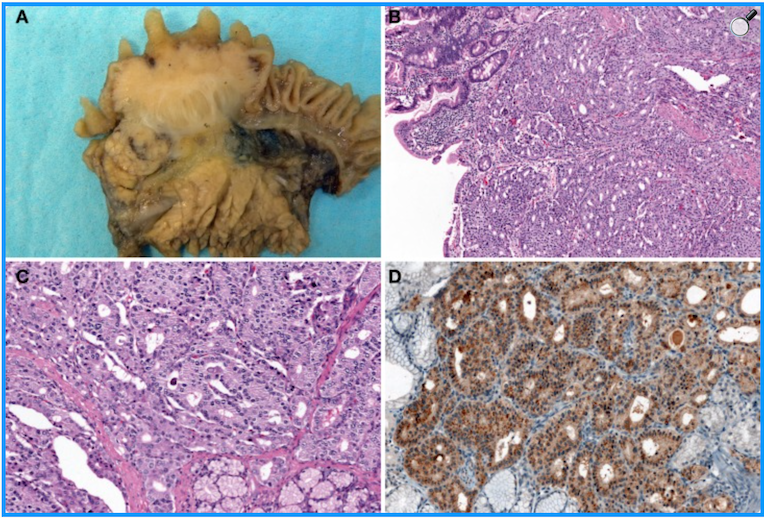
Figure: Figure 1. ERCP: a large fungating mass measuring 30mm in diameter was found at the major papilla. A severe malignant-appearing biliary stricture was found. A pancreatic duct stricture was found. The ampullary mass was biopsied.
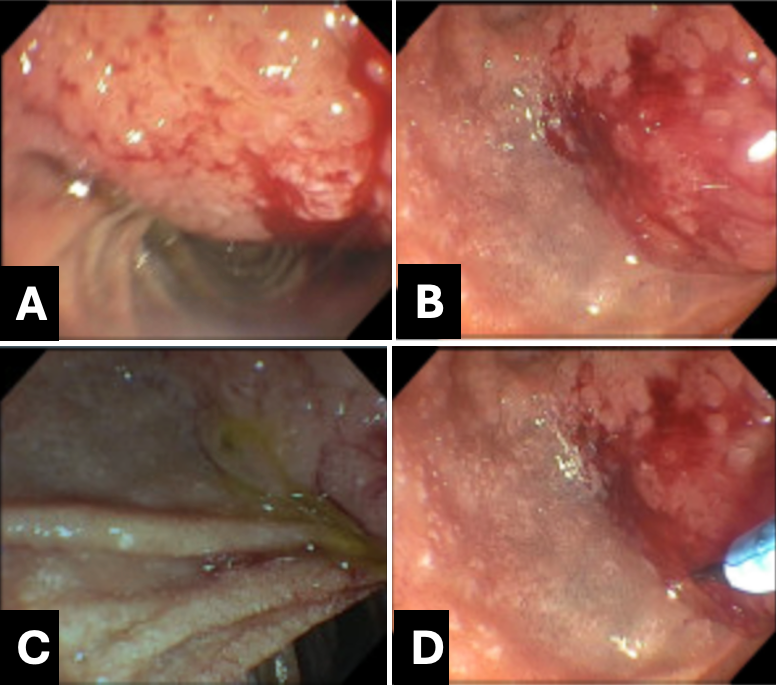
Figure: An example of Somatostatin-producing NETs arising from the major papilla (biopsy images from our case are pending). Macroscopic findings show the solid, polypoid mass in the papilla of Vater (A). The tumor is arranged in a trabecular pattern with pseudoglandular structures (H and E stain, B: low power view, C: high power view). Immunohistochemically, the tumor cells are positive for somatostatin (D), like our patient [1].
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Teresa Da Cunha indicated no relevant financial relationships.
Steven Goldenberg indicated no relevant financial relationships.
Bianca Thakkar, DO1, Teresa Da Cunha, MD2, Steven Goldenberg, MD1. P0182 - Pancreatic NET in a Patient With NF1: Diagnostic Challenges and Long-Term Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut Health, Hartford, CT
Introduction: Neurofibromatosis type 1 (NF1) is an autosomal dominant disorder predisposing to a spectrum of gastrointestinal neoplasms, including periampullary and pancreatic neuroendocrine tumors (NETs). While duodenal and periampullary NETs are more common in NF1, pancreatic NETs are rare but clinically significant, often presenting with nonspecific symptoms or incidentally during evaluation for abnormal liver function tests. The risk of multifocal and synchronous tumors in NF1 necessitates a high index of suspicion and comprehensive evaluation.
Case Description/
Methods: A 50-year-old man with NF1, epilepsy, and a history of a well-differentiated pancreatic NET presented with elevated liver enzymes. Magnetic resonance cholangiopancreatography (MRCP) showed mild intrahepatic and extrahepatic biliary dilatation. Follow-up abdominal MRI revealed no additional findings. Endoscopic retrograde cholangiopancreatography (ERCP) identified a 3 cm mass at the major papilla with biliary stricture; biopsy confirmed a well-differentiated NET. He underwent a Whipple procedure, which revealed a 2.5 cm well-differentiated NET without metastases. PET imaging was negative for distant disease. Postoperatively, the patient was monitored with clinical follow-up every 6–12 months and annual imaging.
Six years later, a positive Cologuard test prompted colonoscopy, which identified and removed three polyps: a 12 mm polyp in the descending colon, a 9 mm polyp in the proximal sigmoid, and a 20 mm polyp in the distal sigmoid. Pathology confirmed benign adenomas. An upper endoscopy was performed to evaluate for additional NETs or gastrointestinal stromal tumors (GISTs) and was unremarkable.
Discussion: Patients with NF1 are at increased risk for gastrointestinal NETs, including rare pancreatic NETs, which may arise independently or synchronously with other tumors. Current guidelines recommend surgical resection for well-differentiated periampullary or pancreatic NETs >2 cm or with local invasion, as in this case. In NF1, a Whipple procedure is preferred due to higher risk of nodal involvement and multifocal disease. Long-term surveillance is crucial, given the potential for late recurrence and new primary tumors. This case underscores the importance of multidisciplinary management and vigilant follow-up in NF1 patients with gastrointestinal neoplasms.
References:
1.Katzka DA, Pandolfino JE, Kahrilas PJ. Gastroenterology, January 2013; 144(1): 27–38. Phenotypes of achalasia: beyond the Chicago classification.
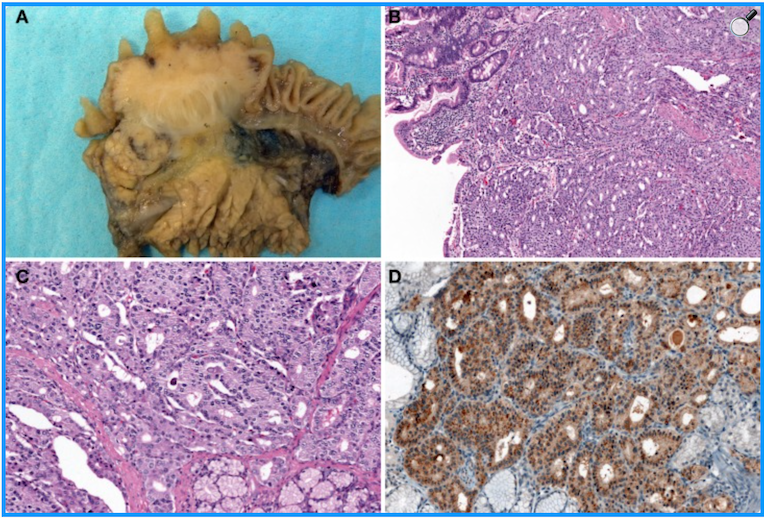
Figure: Figure 1. ERCP: a large fungating mass measuring 30mm in diameter was found at the major papilla. A severe malignant-appearing biliary stricture was found. A pancreatic duct stricture was found. The ampullary mass was biopsied.
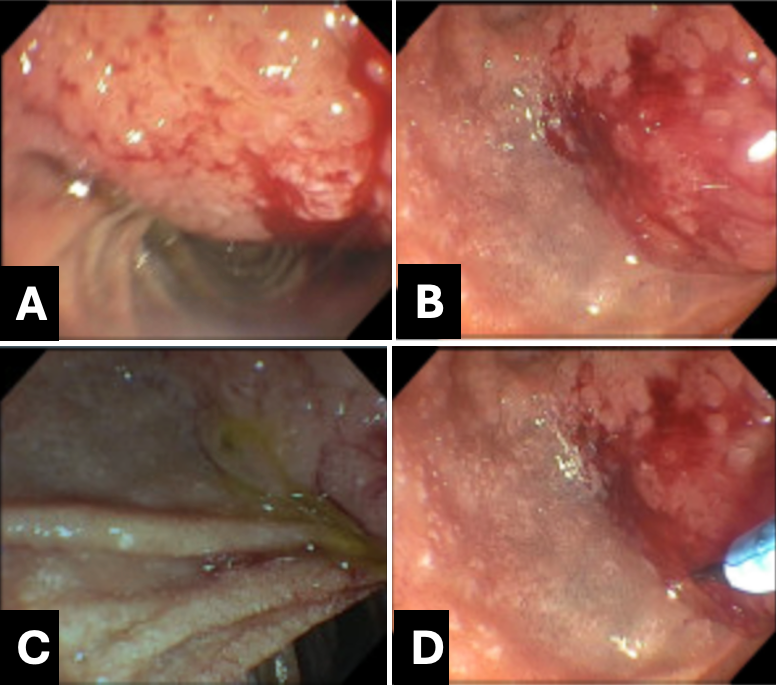
Figure: An example of Somatostatin-producing NETs arising from the major papilla (biopsy images from our case are pending). Macroscopic findings show the solid, polypoid mass in the papilla of Vater (A). The tumor is arranged in a trabecular pattern with pseudoglandular structures (H and E stain, B: low power view, C: high power view). Immunohistochemically, the tumor cells are positive for somatostatin (D), like our patient [1].
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Teresa Da Cunha indicated no relevant financial relationships.
Steven Goldenberg indicated no relevant financial relationships.
Bianca Thakkar, DO1, Teresa Da Cunha, MD2, Steven Goldenberg, MD1. P0182 - Pancreatic NET in a Patient With NF1: Diagnostic Challenges and Long-Term Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
