Sunday Poster Session
Category: Biliary/Pancreas
P0180 - Main-Duct Intraductal Papillary Mucinous Neoplasm: An Infrequent but Not Uncommon Etiology of Recurrent Acute Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishi Bolla, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Rishi Bolla, MD1, Saraswathi Cappelle, DO2, Mark Friedman, MD2, Schaffer Mok, MD2, Luis Pena, MD2, Anjuli K. Luthra, MD2
1University of South Florida Morsani College of Medicine, Tampa, FL; 2Moffitt Cancer Center, Tampa, FL
Introduction: Acute pancreatitis (AP) remains the most common gastrointestinal (GI) disorder resulting in hospitalization. Of these patients, up to 30% will go on to develop recurrent acute pancreatitis (RAP) following recovery of their index attack (1). While the most common causes are biliary and alcohol use, less common etiologies must remain in the differential (1, 2).
Case Description/
Methods: A 62-year-old man with a history of asthma and Type 2 diabetes presented to his local hospital with nausea, vomiting, and abdominal pain. His workup confirmed a diagnosis of AP with computed tomography (CT) demonstrating a lack of biliary disease with 5mm pancreatic duct (PD) dilation. Given his lack of excessive alcohol consumption and negative laboratory workup, he was treated supportively and discharged with unclear etiology. He went on to develop two subsequent episodes of AP, prompting referral for second opinion six months after his initial presentation with AP. Given incidental finding of PD dilation, endoscopic ultrasound (EUS) was performed. This revealed a fish mouth ampulla with mucin output and PD diameter of 16mm with intraductal papillae and mucin globules concerning for main duct intraductal papillary mucinous neoplasm (MD-IPMN) with atrophic pancreas tail. He thus underwent a Whipple resection with pathology confirming for MD-IPMN with high-grade dysplasia.
Discussion: We present a case of RAP due to previously undiagnosed MD-IPMN with rapid progression. IPMNs of any type may result in AP secondary to PD obstruction from the viscous mucin they produce (1). While an infrequent cause, it is imperative to recognize PD dilation as a concerning feature, particularly in AP and proceed with further diagnostic workup (2).
References
1. Venkatesh PG, Navaneethan U, Vege SS. Intraductal papillary mucinous neoplasm and acute pancreatitis. J Clin Gastroenterol. 2011;45(9):755-8.
2. Ohtsuka T, Fernandez-Del Castillo C, Furukawa T, Hijioka S, Jang JY, Lennon AM, et al. International evidence-based Kyoto guidelines for the management of intraductal papillary mucinous neoplasm of the pancreas. Pancreatology. 2024;24(2):255-70.
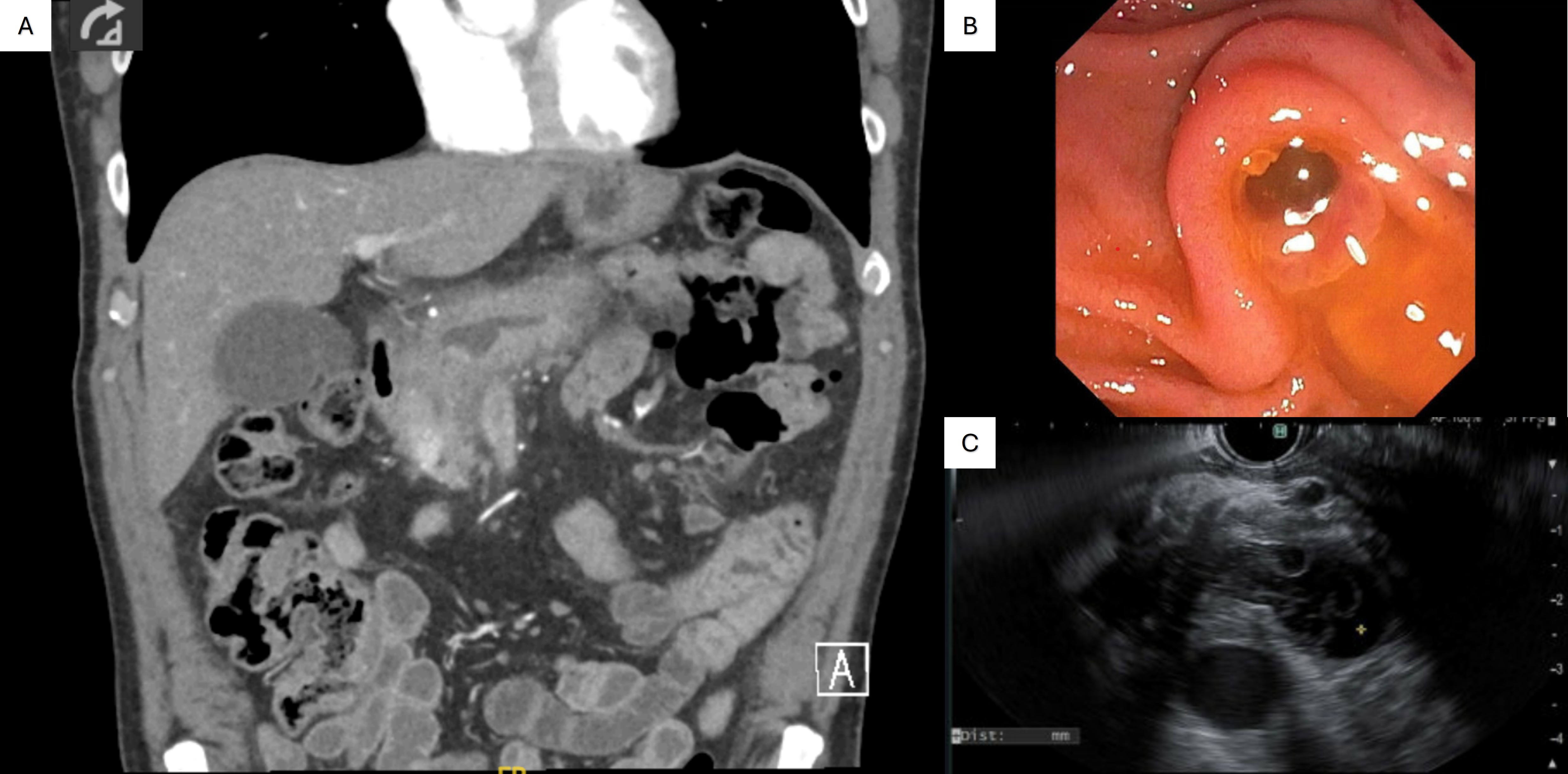
Figure: Figure 1: A) CT scan showing acute pancreatitis with pancreatic duct dilation. B) Endoscopic view of fish-mouth ampulla with mucin output. C) Endoscopic ultrasound view of mucin and papillary structures within the duct.
Disclosures:
Rishi Bolla indicated no relevant financial relationships.
Saraswathi Cappelle: Olympus – Consultant.
Mark Friedman indicated no relevant financial relationships.
Schaffer Mok: Amgen – Consultant. Steris – Consultant.
Luis Pena indicated no relevant financial relationships.
Anjuli Luthra: Boston Scientific – Consultant. Cook Medical – Speakers Bureau.
Rishi Bolla, MD1, Saraswathi Cappelle, DO2, Mark Friedman, MD2, Schaffer Mok, MD2, Luis Pena, MD2, Anjuli K. Luthra, MD2. P0180 - Main-Duct Intraductal Papillary Mucinous Neoplasm: An Infrequent but Not Uncommon Etiology of Recurrent Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2Moffitt Cancer Center, Tampa, FL
Introduction: Acute pancreatitis (AP) remains the most common gastrointestinal (GI) disorder resulting in hospitalization. Of these patients, up to 30% will go on to develop recurrent acute pancreatitis (RAP) following recovery of their index attack (1). While the most common causes are biliary and alcohol use, less common etiologies must remain in the differential (1, 2).
Case Description/
Methods: A 62-year-old man with a history of asthma and Type 2 diabetes presented to his local hospital with nausea, vomiting, and abdominal pain. His workup confirmed a diagnosis of AP with computed tomography (CT) demonstrating a lack of biliary disease with 5mm pancreatic duct (PD) dilation. Given his lack of excessive alcohol consumption and negative laboratory workup, he was treated supportively and discharged with unclear etiology. He went on to develop two subsequent episodes of AP, prompting referral for second opinion six months after his initial presentation with AP. Given incidental finding of PD dilation, endoscopic ultrasound (EUS) was performed. This revealed a fish mouth ampulla with mucin output and PD diameter of 16mm with intraductal papillae and mucin globules concerning for main duct intraductal papillary mucinous neoplasm (MD-IPMN) with atrophic pancreas tail. He thus underwent a Whipple resection with pathology confirming for MD-IPMN with high-grade dysplasia.
Discussion: We present a case of RAP due to previously undiagnosed MD-IPMN with rapid progression. IPMNs of any type may result in AP secondary to PD obstruction from the viscous mucin they produce (1). While an infrequent cause, it is imperative to recognize PD dilation as a concerning feature, particularly in AP and proceed with further diagnostic workup (2).
References
1. Venkatesh PG, Navaneethan U, Vege SS. Intraductal papillary mucinous neoplasm and acute pancreatitis. J Clin Gastroenterol. 2011;45(9):755-8.
2. Ohtsuka T, Fernandez-Del Castillo C, Furukawa T, Hijioka S, Jang JY, Lennon AM, et al. International evidence-based Kyoto guidelines for the management of intraductal papillary mucinous neoplasm of the pancreas. Pancreatology. 2024;24(2):255-70.
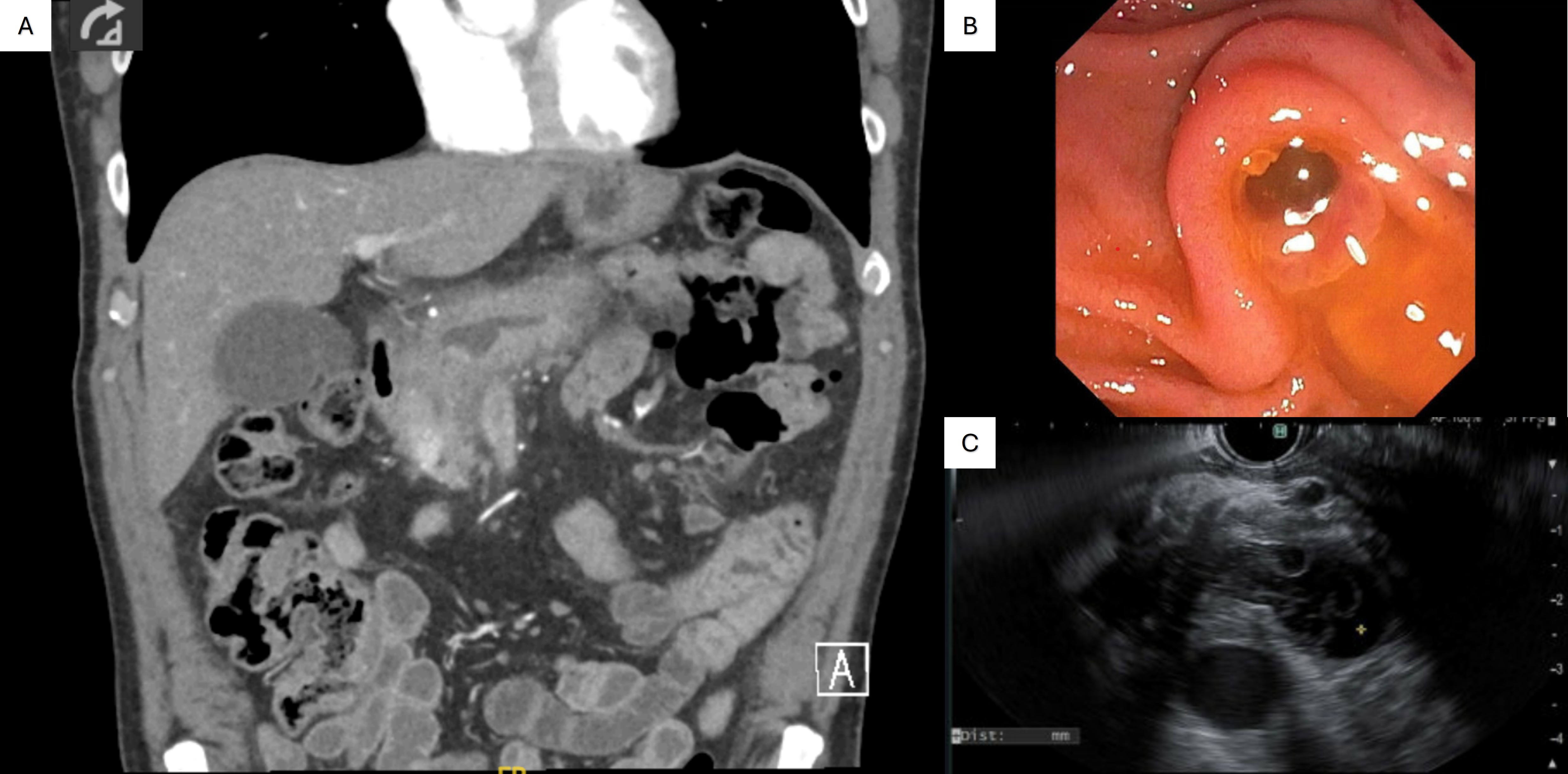
Figure: Figure 1: A) CT scan showing acute pancreatitis with pancreatic duct dilation. B) Endoscopic view of fish-mouth ampulla with mucin output. C) Endoscopic ultrasound view of mucin and papillary structures within the duct.
Disclosures:
Rishi Bolla indicated no relevant financial relationships.
Saraswathi Cappelle: Olympus – Consultant.
Mark Friedman indicated no relevant financial relationships.
Schaffer Mok: Amgen – Consultant. Steris – Consultant.
Luis Pena indicated no relevant financial relationships.
Anjuli Luthra: Boston Scientific – Consultant. Cook Medical – Speakers Bureau.
Rishi Bolla, MD1, Saraswathi Cappelle, DO2, Mark Friedman, MD2, Schaffer Mok, MD2, Luis Pena, MD2, Anjuli K. Luthra, MD2. P0180 - Main-Duct Intraductal Papillary Mucinous Neoplasm: An Infrequent but Not Uncommon Etiology of Recurrent Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
