Sunday Poster Session
Category: Biliary/Pancreas
P0172 - AI-Driven Endoscopic Ultrasound – a Case Series of Applications in Multiple Clinical Settings
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Miguel Mascarenhas, MD, PhD
Centro Hospitalar Universitário São João
Porto, Porto, Portugal
Presenting Author(s)
Award: ACG Presidential Poster Award
Francisco Mendes, MD1, Mariano Gonzalez Haba, MD2, Jessica Widmer, DO3, Miguel Martins, MD1, António Costa, MD2, Tiago Ribeiro, MD1, Belen Agudo, MD2, Matheus Ferreira de Carvalho, MD4, Marcos Eduardo Lera dos Santos, MD4, Eduardo Hourneaux De Moura, MD, PhD5, Filipe Vilas Boas, MD, PhD6, Pedro Moutinho Ribeiro, MD, PhD6, Susana Lopes, MD, PhD6, João Ferreira, PhD7, Miguel Mascarenhas Saraiva, MD, PhD1, Guilherme Macedo, MD, PhD1
1Centro Hospitalar Universitário São João, Porto, Porto, Portugal; 2Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Madrid, Spain; 3NYU Langone Health, Mineola, NY; 4Hospital das Clínicas da Faculdade de Medicina da Universidade de Sao Paulo, São Paulo, Sao Paulo, Brazil; 5Hospital das Clínicas da Faculdade de Medicina da USP, São Paulo, Sao Paulo, Brazil; 6Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 7Faculdade de Engenharia da Universidade do Porto, Porto, Porto, Portugal
Introduction: Endoscopic ultrasound (EUS) can be performed in a wide range of clinical scenarios, being particularly fundamental for the assessment of pancreatic cystic and solid lesions, as well as for the evaluation of chronic pancreatitis. Additionally, EUS plays a key role in lymph node assessment for staging of gastrointestinal and lung cancers. Thanks to its proximity to target structures and the ability to obtain tissue samples, EUS can directly inform patient management. However, its diagnostic accuracy remains suboptimal and is affected by high interobserver variability in lesion interpretation and sampling.
This case series illustrates how a previously published AI-based tool can be integrated into EUS in three distinct clinical scenarios. Importantly, model predictions and AI outputs did not influence clinical decision-making during the procedures.
Case Description/
Methods: In case 1, A 64-year-old patient with jaundice and weight loss underwent EUS, which revealed a solid-cystic mass in the head of the pancreas. The AI-based cystic component analysis predicted a probability over 90% of a mucinous cystic lesion. Evaluation of the solid component yielded a probability over 85% of adenocarcinoma. Targeted sampling confirmed the presence of adenocarcinoma arising from a intraductal papillary mucinous neoplasm (IPMN) in the head of pancreas. In case 2, during evaluation of a 50-year-old patient with chronic pancreatitis and normal tumor markers, EUS identified an 18 mm peripancreatic lymph node. AI-based lymph node analysis predicted a benign/reactive profile, which was later confirmed by histology and clinical follow-up. In case 3, a 65-year-old female with fatigue and weight loss underwent EUS due to suspicious celiac lymph nodes identified on CT imaging. During the EUS, AI analysis predicted malignancy in one of the lymph nodes. Given the endoscopic appearance, the node was biopsied, and histology confirmed metastatic lung cancer.
Discussion: This multicenter case series highlights the potential of AI integration into EUS clinical practice, offering real-time support in diagnostic evaluation and lesion sampling. Applications include the assessment of pancreatic focal lesions, evaluation of patients with chronic pancreatitis, and lymph node characterization. Although AI-assisted EUS is not intended to replace histopathological diagnosis, it may play a pivotal role in clinical decision-making, transforming the management of patients undergoing this procedure.
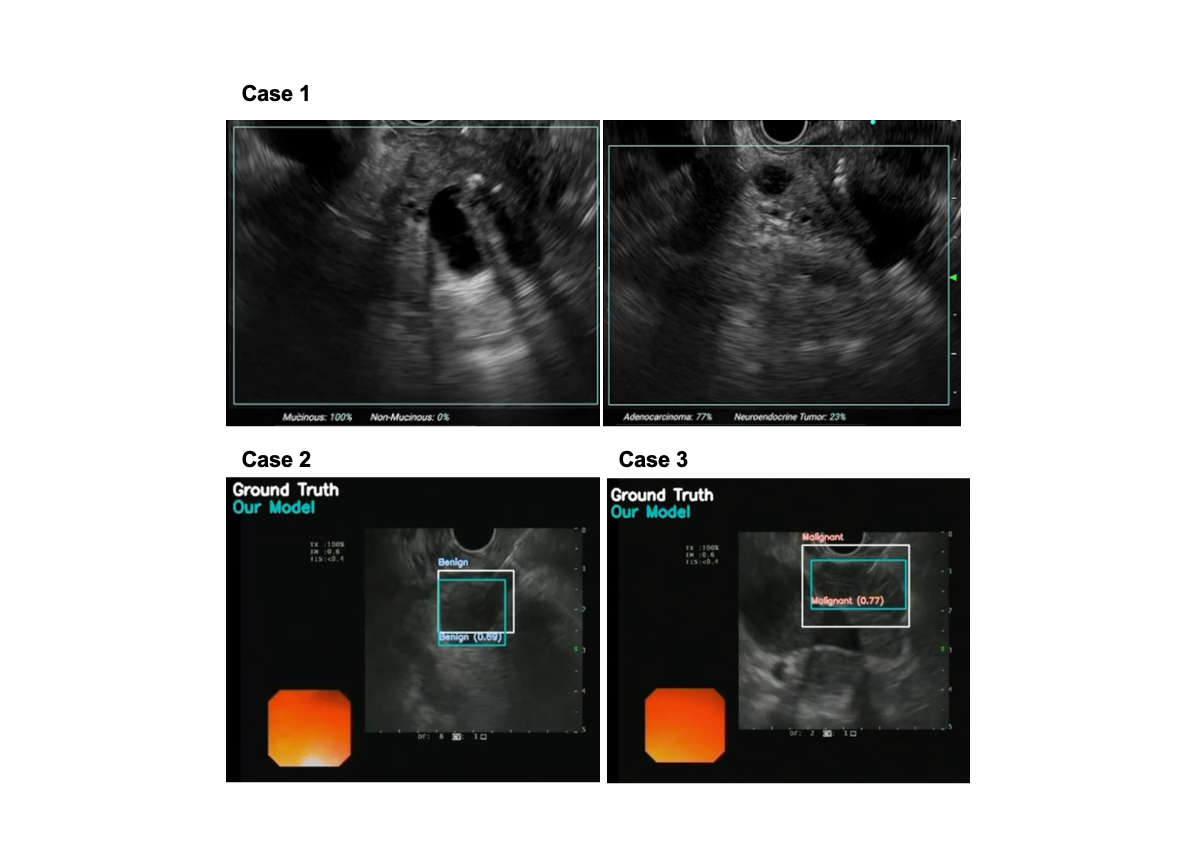
Figure: Figure 1 – Clinical Case Application of Artificial Intelligence during Endoscopic Ultrasound
Case 1) Evaluation of pancreatic cystic and solid lesions
Case 2) Lymph node assessment in a patient with chronic pancreatitis
Case 3) Lymph node assessment in a patient with metastatic lung cancer
Disclosures:
Francisco Mendes indicated no relevant financial relationships.
Mariano Gonzalez Haba indicated no relevant financial relationships.
Jessica Widmer indicated no relevant financial relationships.
Miguel Martins indicated no relevant financial relationships.
António Costa indicated no relevant financial relationships.
Tiago Ribeiro indicated no relevant financial relationships.
Belen Agudo indicated no relevant financial relationships.
Matheus Ferreira de Carvalho indicated no relevant financial relationships.
Marcos Eduardo Lera dos Santos indicated no relevant financial relationships.
Eduardo Hourneaux De Moura indicated no relevant financial relationships.
Filipe Vilas Boas indicated no relevant financial relationships.
Pedro Moutinho Ribeiro indicated no relevant financial relationships.
Susana Lopes indicated no relevant financial relationships.
João Ferreira indicated no relevant financial relationships.
Miguel Mascarenhas Saraiva indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Francisco Mendes, MD1, Mariano Gonzalez Haba, MD2, Jessica Widmer, DO3, Miguel Martins, MD1, António Costa, MD2, Tiago Ribeiro, MD1, Belen Agudo, MD2, Matheus Ferreira de Carvalho, MD4, Marcos Eduardo Lera dos Santos, MD4, Eduardo Hourneaux De Moura, MD, PhD5, Filipe Vilas Boas, MD, PhD6, Pedro Moutinho Ribeiro, MD, PhD6, Susana Lopes, MD, PhD6, João Ferreira, PhD7, Miguel Mascarenhas Saraiva, MD, PhD1, Guilherme Macedo, MD, PhD1. P0172 - AI-Driven Endoscopic Ultrasound – a Case Series of Applications in Multiple Clinical Settings, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Francisco Mendes, MD1, Mariano Gonzalez Haba, MD2, Jessica Widmer, DO3, Miguel Martins, MD1, António Costa, MD2, Tiago Ribeiro, MD1, Belen Agudo, MD2, Matheus Ferreira de Carvalho, MD4, Marcos Eduardo Lera dos Santos, MD4, Eduardo Hourneaux De Moura, MD, PhD5, Filipe Vilas Boas, MD, PhD6, Pedro Moutinho Ribeiro, MD, PhD6, Susana Lopes, MD, PhD6, João Ferreira, PhD7, Miguel Mascarenhas Saraiva, MD, PhD1, Guilherme Macedo, MD, PhD1
1Centro Hospitalar Universitário São João, Porto, Porto, Portugal; 2Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Madrid, Spain; 3NYU Langone Health, Mineola, NY; 4Hospital das Clínicas da Faculdade de Medicina da Universidade de Sao Paulo, São Paulo, Sao Paulo, Brazil; 5Hospital das Clínicas da Faculdade de Medicina da USP, São Paulo, Sao Paulo, Brazil; 6Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 7Faculdade de Engenharia da Universidade do Porto, Porto, Porto, Portugal
Introduction: Endoscopic ultrasound (EUS) can be performed in a wide range of clinical scenarios, being particularly fundamental for the assessment of pancreatic cystic and solid lesions, as well as for the evaluation of chronic pancreatitis. Additionally, EUS plays a key role in lymph node assessment for staging of gastrointestinal and lung cancers. Thanks to its proximity to target structures and the ability to obtain tissue samples, EUS can directly inform patient management. However, its diagnostic accuracy remains suboptimal and is affected by high interobserver variability in lesion interpretation and sampling.
This case series illustrates how a previously published AI-based tool can be integrated into EUS in three distinct clinical scenarios. Importantly, model predictions and AI outputs did not influence clinical decision-making during the procedures.
Case Description/
Methods: In case 1, A 64-year-old patient with jaundice and weight loss underwent EUS, which revealed a solid-cystic mass in the head of the pancreas. The AI-based cystic component analysis predicted a probability over 90% of a mucinous cystic lesion. Evaluation of the solid component yielded a probability over 85% of adenocarcinoma. Targeted sampling confirmed the presence of adenocarcinoma arising from a intraductal papillary mucinous neoplasm (IPMN) in the head of pancreas. In case 2, during evaluation of a 50-year-old patient with chronic pancreatitis and normal tumor markers, EUS identified an 18 mm peripancreatic lymph node. AI-based lymph node analysis predicted a benign/reactive profile, which was later confirmed by histology and clinical follow-up. In case 3, a 65-year-old female with fatigue and weight loss underwent EUS due to suspicious celiac lymph nodes identified on CT imaging. During the EUS, AI analysis predicted malignancy in one of the lymph nodes. Given the endoscopic appearance, the node was biopsied, and histology confirmed metastatic lung cancer.
Discussion: This multicenter case series highlights the potential of AI integration into EUS clinical practice, offering real-time support in diagnostic evaluation and lesion sampling. Applications include the assessment of pancreatic focal lesions, evaluation of patients with chronic pancreatitis, and lymph node characterization. Although AI-assisted EUS is not intended to replace histopathological diagnosis, it may play a pivotal role in clinical decision-making, transforming the management of patients undergoing this procedure.
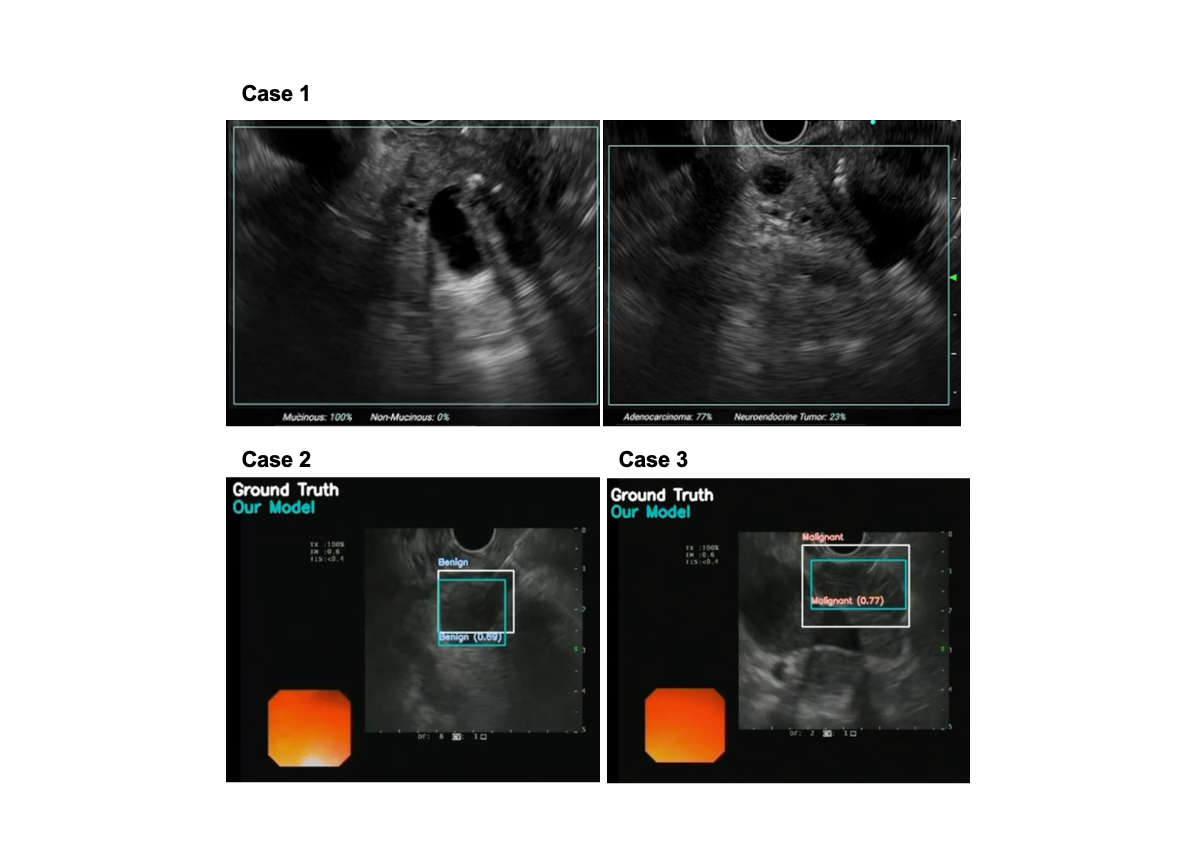
Figure: Figure 1 – Clinical Case Application of Artificial Intelligence during Endoscopic Ultrasound
Case 1) Evaluation of pancreatic cystic and solid lesions
Case 2) Lymph node assessment in a patient with chronic pancreatitis
Case 3) Lymph node assessment in a patient with metastatic lung cancer
Disclosures:
Francisco Mendes indicated no relevant financial relationships.
Mariano Gonzalez Haba indicated no relevant financial relationships.
Jessica Widmer indicated no relevant financial relationships.
Miguel Martins indicated no relevant financial relationships.
António Costa indicated no relevant financial relationships.
Tiago Ribeiro indicated no relevant financial relationships.
Belen Agudo indicated no relevant financial relationships.
Matheus Ferreira de Carvalho indicated no relevant financial relationships.
Marcos Eduardo Lera dos Santos indicated no relevant financial relationships.
Eduardo Hourneaux De Moura indicated no relevant financial relationships.
Filipe Vilas Boas indicated no relevant financial relationships.
Pedro Moutinho Ribeiro indicated no relevant financial relationships.
Susana Lopes indicated no relevant financial relationships.
João Ferreira indicated no relevant financial relationships.
Miguel Mascarenhas Saraiva indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Francisco Mendes, MD1, Mariano Gonzalez Haba, MD2, Jessica Widmer, DO3, Miguel Martins, MD1, António Costa, MD2, Tiago Ribeiro, MD1, Belen Agudo, MD2, Matheus Ferreira de Carvalho, MD4, Marcos Eduardo Lera dos Santos, MD4, Eduardo Hourneaux De Moura, MD, PhD5, Filipe Vilas Boas, MD, PhD6, Pedro Moutinho Ribeiro, MD, PhD6, Susana Lopes, MD, PhD6, João Ferreira, PhD7, Miguel Mascarenhas Saraiva, MD, PhD1, Guilherme Macedo, MD, PhD1. P0172 - AI-Driven Endoscopic Ultrasound – a Case Series of Applications in Multiple Clinical Settings, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

