Sunday Poster Session
Category: Biliary/Pancreas
P0169 - Unmasking the Ampulla: A Case of Painless Jaundice and Adenocarcinoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Stephanie Colon-Marrero, MD (she/her/hers)
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Stephanie Colon-Marrero, MD1, Frances N.. Connor-Recio, MD2, Juan G. Feliciano-Figueroa, MD1
1VA Caribbean Healthcare System, San Juan, Puerto Rico; 2VA Caribbean Healthcare System, Guaynabo, Puerto Rico
Introduction: Ampullary adenocarcinoma is a rare malignancy accounting for approximately 0.2% of gastrointestinal cancers and 6% of all periampullary cancers. It commonly presents with obstructive jaundice due to its anatomical location. Early diagnosis and treatment are crucial as the prognosis is more favorable compared to other periampullary cancers.
Case Description/
Methods: A 61-year-old male with medical history of gastroesophageal reflux disease presented with jaundice one day prior to arrival. Patient also reported dark urine, pale colored soft stools, and increased itching all over body. He denied nausea, vomiting, abdominal pain, undesired weight loss, new medications or toxic habits. Physical exam revealed scleral icterus, jaundice, and a benign abdomen. Laboratories were remarkable for cholestatic liver injury and a normal CA 19-9. Abdominal ultrasound revealed intra and extrahepatic biliary duct dilation with a hydropic gallbladder. CT scan showed biliary ducts dilation but did not identify any gallstone or mass for which an endoscopic retrograde cholangiopancreatography (ERCP) was performed. ERCP showed prominent, indurated, and ulcerated major papilla causing biliary obstruction, and a plastic stent was placed (Figure 1). Biopsies reported moderately differentiated adenocarcinoma. PET scan did not identify no significant FDG avid lesions (Figure 2). The patient underwent a pancreaticoduodenectomy (Whipple procedure) and the histopathology confirmed invasive ampullary adenocarcinoma with positive lymph nodes (T3N1, stage IIIa). Due to young age, the patient is scheduled for adjuvant chemotherapy.
Discussion: This case emphasizes the importance of including ampullary adenocarcinoma in the differential diagnosis for patients presenting with painless jaundice and cholestatic liver enzyme elevation, even in the absence of a mass on initial imaging. ERCP with biopsy is a key diagnostic tool when imaging is inconclusive. Surgical resection remains the mainstay of treatment, and adjuvant chemotherapy is recommended in lymph node-positive disease. However, the risk of disease progression despite aggressive chemotherapy highlights the need for continued surveillance and multidisciplinary care. This case illustrates the diagnostic and therapeutic challenges of this rare gastrointestinal malignancy and the importance of a multidisciplinary approach in its management. Despite surgical and chemotherapeutic advances, recurrence risk remains significant, warranting close surveillance.
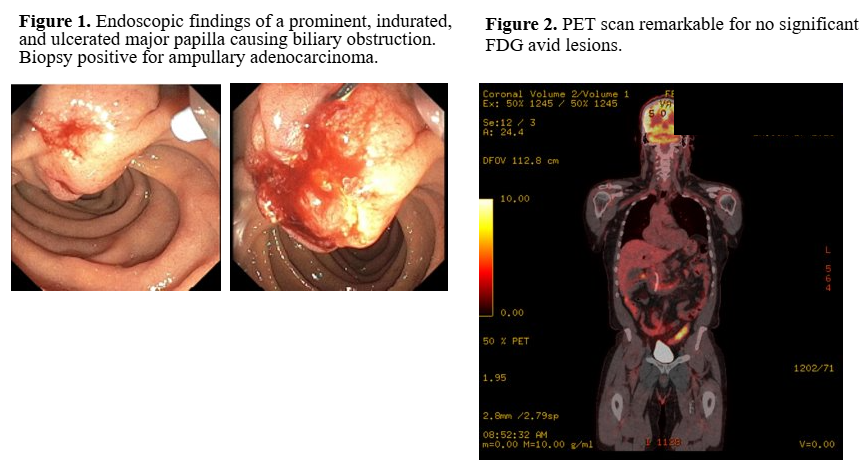
Figure: Ampullary adenocarcinoma with lymph node metastasis and a negative PET scan.
Disclosures:
Stephanie Colon-Marrero indicated no relevant financial relationships.
Frances Connor-Recio indicated no relevant financial relationships.
Juan G. Feliciano-Figueroa indicated no relevant financial relationships.
Stephanie Colon-Marrero, MD1, Frances N.. Connor-Recio, MD2, Juan G. Feliciano-Figueroa, MD1. P0169 - Unmasking the Ampulla: A Case of Painless Jaundice and Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1VA Caribbean Healthcare System, San Juan, Puerto Rico; 2VA Caribbean Healthcare System, Guaynabo, Puerto Rico
Introduction: Ampullary adenocarcinoma is a rare malignancy accounting for approximately 0.2% of gastrointestinal cancers and 6% of all periampullary cancers. It commonly presents with obstructive jaundice due to its anatomical location. Early diagnosis and treatment are crucial as the prognosis is more favorable compared to other periampullary cancers.
Case Description/
Methods: A 61-year-old male with medical history of gastroesophageal reflux disease presented with jaundice one day prior to arrival. Patient also reported dark urine, pale colored soft stools, and increased itching all over body. He denied nausea, vomiting, abdominal pain, undesired weight loss, new medications or toxic habits. Physical exam revealed scleral icterus, jaundice, and a benign abdomen. Laboratories were remarkable for cholestatic liver injury and a normal CA 19-9. Abdominal ultrasound revealed intra and extrahepatic biliary duct dilation with a hydropic gallbladder. CT scan showed biliary ducts dilation but did not identify any gallstone or mass for which an endoscopic retrograde cholangiopancreatography (ERCP) was performed. ERCP showed prominent, indurated, and ulcerated major papilla causing biliary obstruction, and a plastic stent was placed (Figure 1). Biopsies reported moderately differentiated adenocarcinoma. PET scan did not identify no significant FDG avid lesions (Figure 2). The patient underwent a pancreaticoduodenectomy (Whipple procedure) and the histopathology confirmed invasive ampullary adenocarcinoma with positive lymph nodes (T3N1, stage IIIa). Due to young age, the patient is scheduled for adjuvant chemotherapy.
Discussion: This case emphasizes the importance of including ampullary adenocarcinoma in the differential diagnosis for patients presenting with painless jaundice and cholestatic liver enzyme elevation, even in the absence of a mass on initial imaging. ERCP with biopsy is a key diagnostic tool when imaging is inconclusive. Surgical resection remains the mainstay of treatment, and adjuvant chemotherapy is recommended in lymph node-positive disease. However, the risk of disease progression despite aggressive chemotherapy highlights the need for continued surveillance and multidisciplinary care. This case illustrates the diagnostic and therapeutic challenges of this rare gastrointestinal malignancy and the importance of a multidisciplinary approach in its management. Despite surgical and chemotherapeutic advances, recurrence risk remains significant, warranting close surveillance.
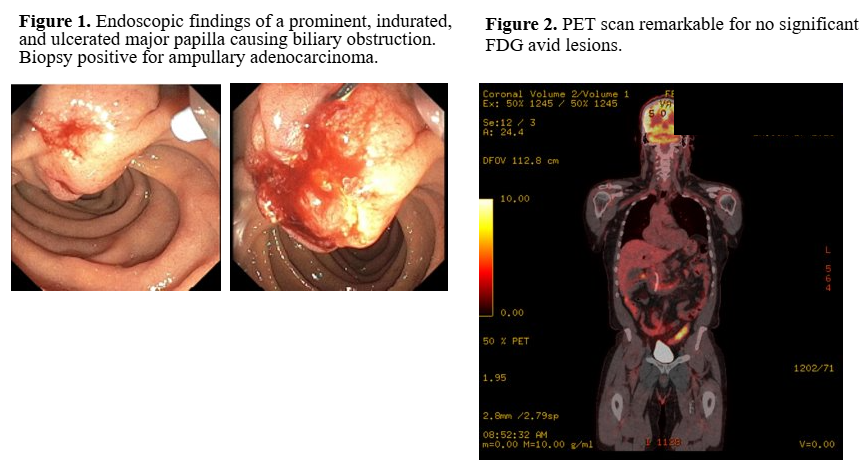
Figure: Ampullary adenocarcinoma with lymph node metastasis and a negative PET scan.
Disclosures:
Stephanie Colon-Marrero indicated no relevant financial relationships.
Frances Connor-Recio indicated no relevant financial relationships.
Juan G. Feliciano-Figueroa indicated no relevant financial relationships.
Stephanie Colon-Marrero, MD1, Frances N.. Connor-Recio, MD2, Juan G. Feliciano-Figueroa, MD1. P0169 - Unmasking the Ampulla: A Case of Painless Jaundice and Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
