Sunday Poster Session
Category: Biliary/Pancreas
P0163 - Pancreaticopleural Fistula Presenting as Refractory Pleural Effusion: A Rare but Treatable Complication of Alcoholic Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Aaqid Siraj Syed, MD (he/him/his)
Mobile Infirmary Medical Centre
Mobile, AL
Presenting Author(s)
Aaqid Siraj Syed, MD1, Akif Siraj Syed, 2, James Byrd, MD1
1Mobile Infirmary Medical Centre, Mobile, AL; 2R.N.T. Medical College, Udaipur, Rajasthan, India
Introduction: Pancreaticopleural fistula (PPF) is an uncommon complication of chronic pancreatitis, characterized by an abnormal ductal communication with the pleural cavity. It typically presents with recurrent pleural effusions and respiratory symptoms, often delaying diagnosis. Timely identification and multidisciplinary intervention are critical to successful outcomes.
Case Description/
Methods: A 34-year-old man with asthma and significant alcohol use disorder presented with a 3-day history of cough, shortness of breath, nausea, and vomiting. Imaging revealed a large left pleural effusion causing near-complete left lung collapse and a CT abdomen consistent with acute pancreatitis and pancreatic head necrosis. Pleural fluid obtained by thoracentesis was dark brown and exudative, with markedly elevated amylase (6689 U/L), raising concern for a PPF.
Despite thoracentesis (2200 mL) and chest tube drainage (1700 mL), effusion persisted. MRCP demonstrated a dilated pancreatic duct with abrupt tapering at the head and suspected fistulous communication. ERCP confirmed ductal disruption, and a plastic stent was placed after sphincterotomy. Subsequent ERCP involved stone extraction and placement of a fully covered metal stent. The stent was left in place for 6-8 weeks to allow spontaneous closure of the fistula by promoting ductal decompression and epithelial healing.
Due to loculated fluid and persistent effusion, video-assisted thoracoscopic surgery (VATS) with decortication and drainage was performed. The patient improved significantly, with normalization of amylase/lipase, resolution of pneumonia, and chest tube removal. He was discharged in stable condition and remained asymptomatic on follow-up.
Discussion: This case underscores the importance of considering PPF in young males with recurrent pleural effusions and a history of pancreatitis. The diagnosis hinges on high pleural fluid amylase levels and imaging modalities such as MRCP and ERCP. While medical management with NPO and octreotide may be trialed, endoscopic stenting remains the first-line definitive treatment. VATS is reserved for refractory cases or complicated effusions. Our patient's outcome highlights the benefit of timely ERCP with ductal stenting followed by surgical intervention for definitive fistula resolution.

Figure: MRCP demonstrating pancreatic ductal pathology in a patient with pancreaticopleural fistula.
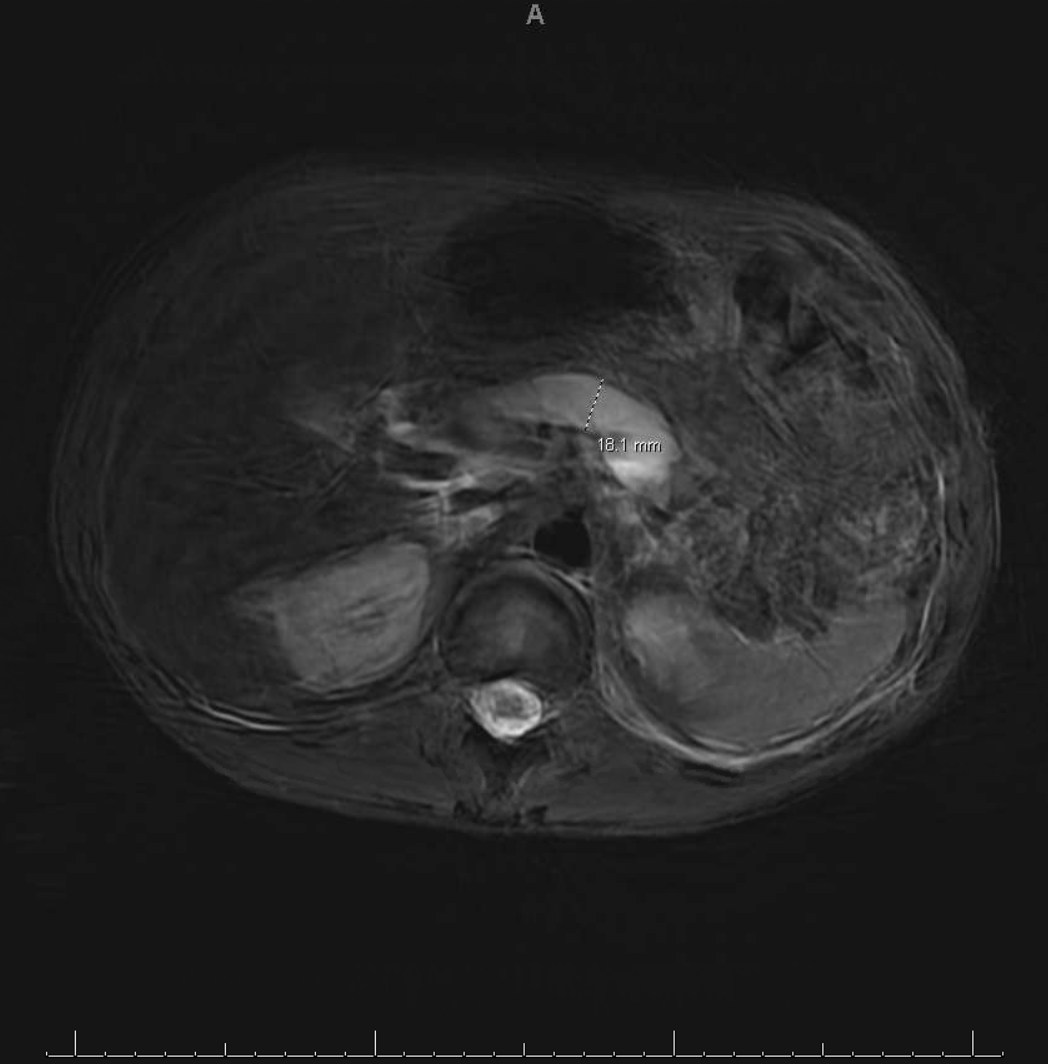
Figure: Upstream pancreatic duct dilation to 18.1 mm, suggestive of a stricture or obstruction at the pancreatic head, correlating with fistula formation.
Disclosures:
Aaqid Siraj Syed indicated no relevant financial relationships.
Akif Siraj Syed indicated no relevant financial relationships.
James Byrd indicated no relevant financial relationships.
Aaqid Siraj Syed, MD1, Akif Siraj Syed, 2, James Byrd, MD1. P0163 - Pancreaticopleural Fistula Presenting as Refractory Pleural Effusion: A Rare but Treatable Complication of Alcoholic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mobile Infirmary Medical Centre, Mobile, AL; 2R.N.T. Medical College, Udaipur, Rajasthan, India
Introduction: Pancreaticopleural fistula (PPF) is an uncommon complication of chronic pancreatitis, characterized by an abnormal ductal communication with the pleural cavity. It typically presents with recurrent pleural effusions and respiratory symptoms, often delaying diagnosis. Timely identification and multidisciplinary intervention are critical to successful outcomes.
Case Description/
Methods: A 34-year-old man with asthma and significant alcohol use disorder presented with a 3-day history of cough, shortness of breath, nausea, and vomiting. Imaging revealed a large left pleural effusion causing near-complete left lung collapse and a CT abdomen consistent with acute pancreatitis and pancreatic head necrosis. Pleural fluid obtained by thoracentesis was dark brown and exudative, with markedly elevated amylase (6689 U/L), raising concern for a PPF.
Despite thoracentesis (2200 mL) and chest tube drainage (1700 mL), effusion persisted. MRCP demonstrated a dilated pancreatic duct with abrupt tapering at the head and suspected fistulous communication. ERCP confirmed ductal disruption, and a plastic stent was placed after sphincterotomy. Subsequent ERCP involved stone extraction and placement of a fully covered metal stent. The stent was left in place for 6-8 weeks to allow spontaneous closure of the fistula by promoting ductal decompression and epithelial healing.
Due to loculated fluid and persistent effusion, video-assisted thoracoscopic surgery (VATS) with decortication and drainage was performed. The patient improved significantly, with normalization of amylase/lipase, resolution of pneumonia, and chest tube removal. He was discharged in stable condition and remained asymptomatic on follow-up.
Discussion: This case underscores the importance of considering PPF in young males with recurrent pleural effusions and a history of pancreatitis. The diagnosis hinges on high pleural fluid amylase levels and imaging modalities such as MRCP and ERCP. While medical management with NPO and octreotide may be trialed, endoscopic stenting remains the first-line definitive treatment. VATS is reserved for refractory cases or complicated effusions. Our patient's outcome highlights the benefit of timely ERCP with ductal stenting followed by surgical intervention for definitive fistula resolution.

Figure: MRCP demonstrating pancreatic ductal pathology in a patient with pancreaticopleural fistula.
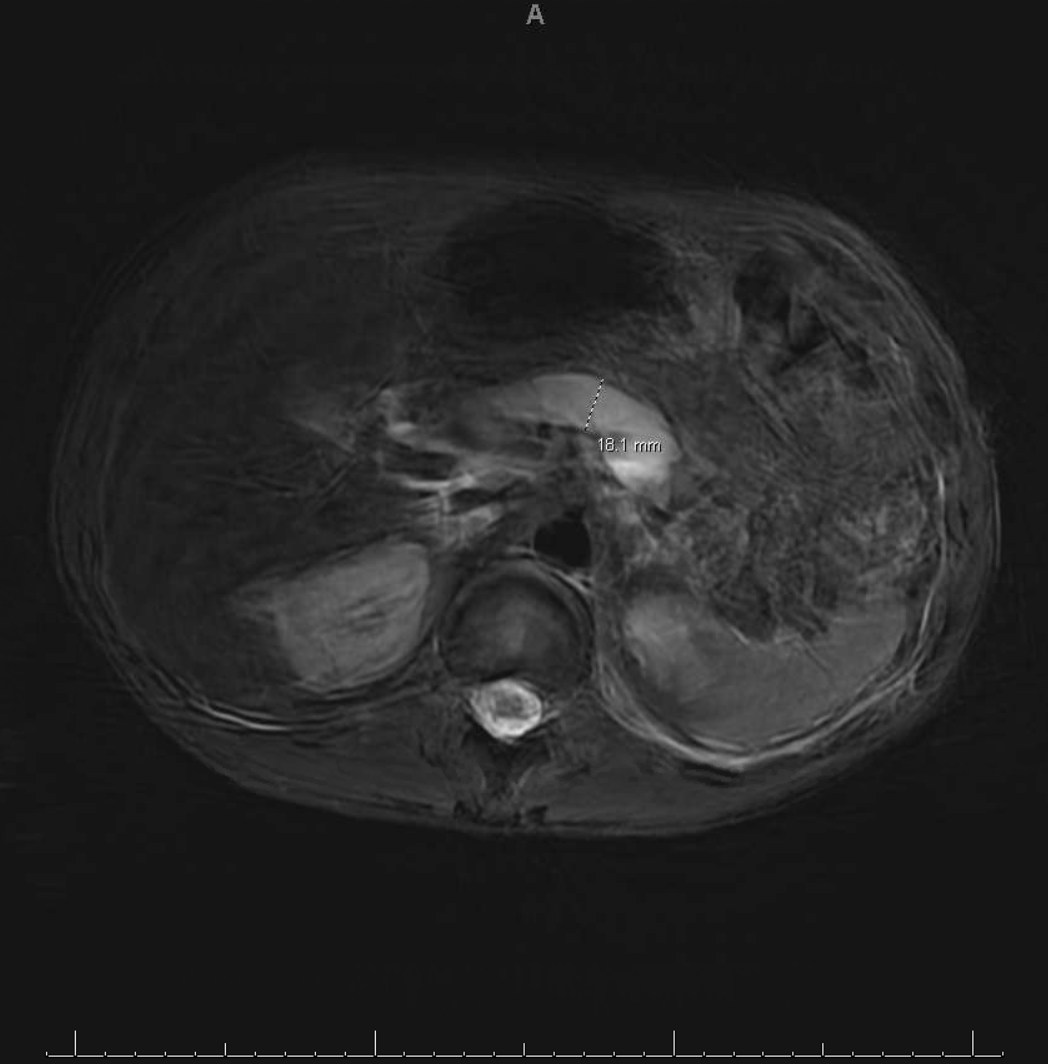
Figure: Upstream pancreatic duct dilation to 18.1 mm, suggestive of a stricture or obstruction at the pancreatic head, correlating with fistula formation.
Disclosures:
Aaqid Siraj Syed indicated no relevant financial relationships.
Akif Siraj Syed indicated no relevant financial relationships.
James Byrd indicated no relevant financial relationships.
Aaqid Siraj Syed, MD1, Akif Siraj Syed, 2, James Byrd, MD1. P0163 - Pancreaticopleural Fistula Presenting as Refractory Pleural Effusion: A Rare but Treatable Complication of Alcoholic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

