Sunday Poster Session
Category: Biliary/Pancreas
P0160 - From Pancreas to Groin: Scrotal Abscess Following Pancreatic Fully Covered Self-Expandable Metal Stent Placement
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jameel Alp, MD (he/him/his)
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Jameel Alp, MD, James Mallery, MD, Guru Trikudanathan, MD, Martin Freeman, MD
University of Minnesota, Minneapolis, MN
Introduction: Fully covered self-expandable metal stents (FCSEMSs) have gained popularity in the endoscopic management of pancreatic duct strictures (PDS), particularly in refractory cases. Although they may offer potential advantages over plastic stents (PSs), recent studies have raised concerns about increased rates of stent-related complications, including migration, secondary strictures, and bile duct obstruction. We present a rare case of scrotal abscess caused by contiguous spread of infected necrosis following FCSEMS placement.
Case Description/
Methods: A 49-year-old man with alcohol-related chronic pancreatitis (CP) underwent placement of a FCSEMS at an outside facility for a benign pancreatic head stricture during routine exchange of PSs, which were found to be partially occluded. He was asymptomatic at the time and remained so for 3 months post-placement. He then presented to our tertiary care center with acute-on-chronic abdominal discomfort and new-onset right groin pain. Computed tomography (CT) revealed a large peripancreatic necrotic collection extending along the right paracolic gutter into the inguinal canal, resulting in a scrotal abscess (Fig. 1). The patient was started on empiric antibiotics and underwent bilateral scrotal incision and drainage (I&D), along with percutaneous drainage of the peripancreatic and paracolic abscesses. Cultures from all 3 sites grew identical organisms, consistent with contiguous spread. The FCSEMS was found to be occluded with food and purulent material; it was removed and replaced with 2 single-pigtail, unflanged PSs (Fig. 2). The patient improved with drainage and antibiotics but required a month-long hospitalization and multiple interventions, including scrotal exploration, repeated debridement, I&D, orchiopexy, and hernia repair. At follow-up 2 months after discharge, he reported feeling well, and CT showed resolution of all abscesses and passed PSs.
Discussion: This case illustrates a rare but serious infectious complication of FCSEMS placement for PDS. Possible mechanisms include not only luminal but also side branch obstruction caused by the FCSEMS, which likely led to an upstream necrosis and extrapancreatic spread, including multiple intraabdominal and scrotal abscesses. While FCSEMSs may benefit select refractory cases, they carry underappreciated risks and should not be routinely used. Our case supports the need for individualized stent selection and further prospective studies to evaluate FCSEMS safety in CP.
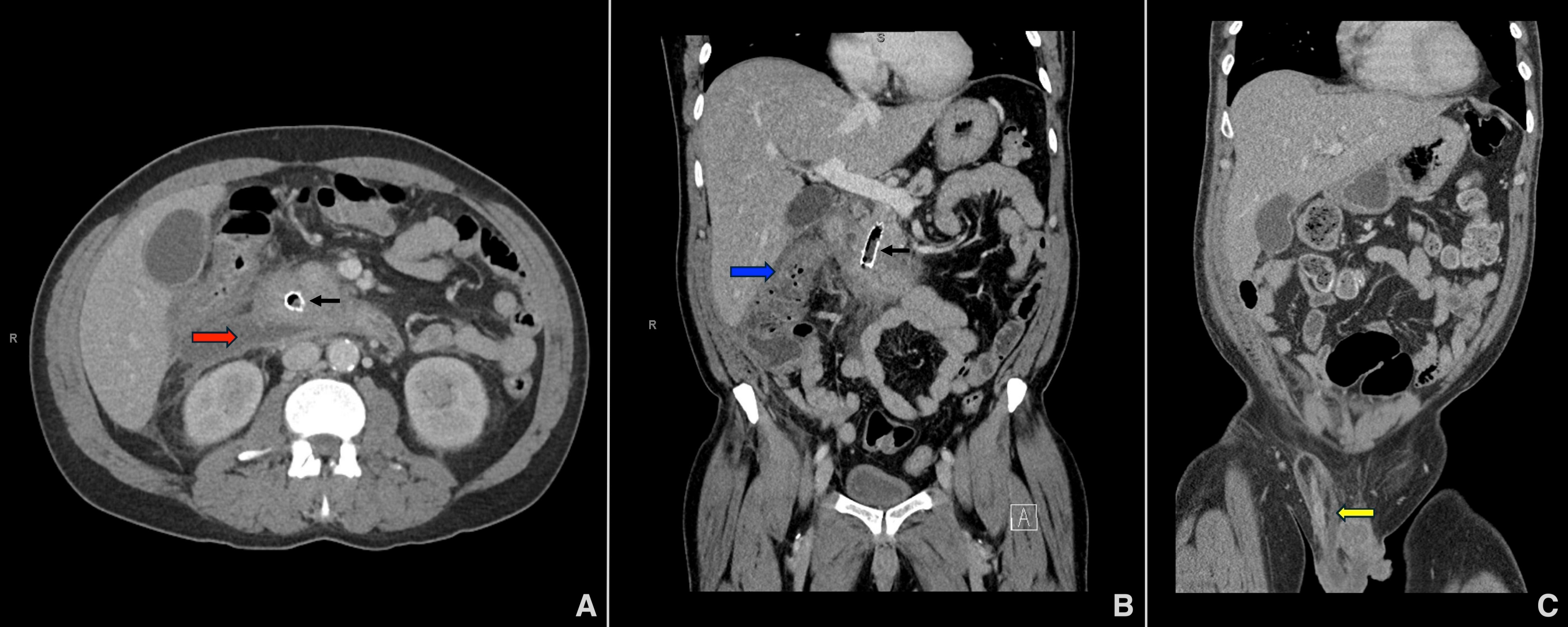
Figure: Figure 1: Multiple CT scans revealed extensive abscesses, including (A) an infected peripancreatic acute necrotic collection (red arrow), (B) duodenitis and colitis at the hepatic flexure (blue arrow) extending into the region of the cecum and the right hemiscrotum, resulting in (C) an abscess in the inguinal canal and spermatic cord (yellow arrow). The FCSEMS is also visible (black arrows).

Figure: Figure 2: In the course of the endoscopic retrograde cholangiopancreatography, (A) the FCSEMS (Viabil®, W.L. Gore & Associates, Flagstaff, AZ, USA) was found to be fully obstructed with food, pus, and debris. (B) Following the clearance of all obstructions using a balloon, the FCSEMS was successfully extracted. (C) Subsequently, two short 7 Fr unflanged plastic stents, each with a complete external pigtail, (Hobbs Medical, Stafford Springs, CT, USA) were inserted into the main pancreatic duct.
Disclosures:
Jameel Alp indicated no relevant financial relationships.
James Mallery indicated no relevant financial relationships.
Guru Trikudanathan: AbbVie – Grant/Research Support. Boston Scientific – Consultant.
Martin Freeman indicated no relevant financial relationships.
Jameel Alp, MD, James Mallery, MD, Guru Trikudanathan, MD, Martin Freeman, MD. P0160 - From Pancreas to Groin: Scrotal Abscess Following Pancreatic Fully Covered Self-Expandable Metal Stent Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Minnesota, Minneapolis, MN
Introduction: Fully covered self-expandable metal stents (FCSEMSs) have gained popularity in the endoscopic management of pancreatic duct strictures (PDS), particularly in refractory cases. Although they may offer potential advantages over plastic stents (PSs), recent studies have raised concerns about increased rates of stent-related complications, including migration, secondary strictures, and bile duct obstruction. We present a rare case of scrotal abscess caused by contiguous spread of infected necrosis following FCSEMS placement.
Case Description/
Methods: A 49-year-old man with alcohol-related chronic pancreatitis (CP) underwent placement of a FCSEMS at an outside facility for a benign pancreatic head stricture during routine exchange of PSs, which were found to be partially occluded. He was asymptomatic at the time and remained so for 3 months post-placement. He then presented to our tertiary care center with acute-on-chronic abdominal discomfort and new-onset right groin pain. Computed tomography (CT) revealed a large peripancreatic necrotic collection extending along the right paracolic gutter into the inguinal canal, resulting in a scrotal abscess (Fig. 1). The patient was started on empiric antibiotics and underwent bilateral scrotal incision and drainage (I&D), along with percutaneous drainage of the peripancreatic and paracolic abscesses. Cultures from all 3 sites grew identical organisms, consistent with contiguous spread. The FCSEMS was found to be occluded with food and purulent material; it was removed and replaced with 2 single-pigtail, unflanged PSs (Fig. 2). The patient improved with drainage and antibiotics but required a month-long hospitalization and multiple interventions, including scrotal exploration, repeated debridement, I&D, orchiopexy, and hernia repair. At follow-up 2 months after discharge, he reported feeling well, and CT showed resolution of all abscesses and passed PSs.
Discussion: This case illustrates a rare but serious infectious complication of FCSEMS placement for PDS. Possible mechanisms include not only luminal but also side branch obstruction caused by the FCSEMS, which likely led to an upstream necrosis and extrapancreatic spread, including multiple intraabdominal and scrotal abscesses. While FCSEMSs may benefit select refractory cases, they carry underappreciated risks and should not be routinely used. Our case supports the need for individualized stent selection and further prospective studies to evaluate FCSEMS safety in CP.
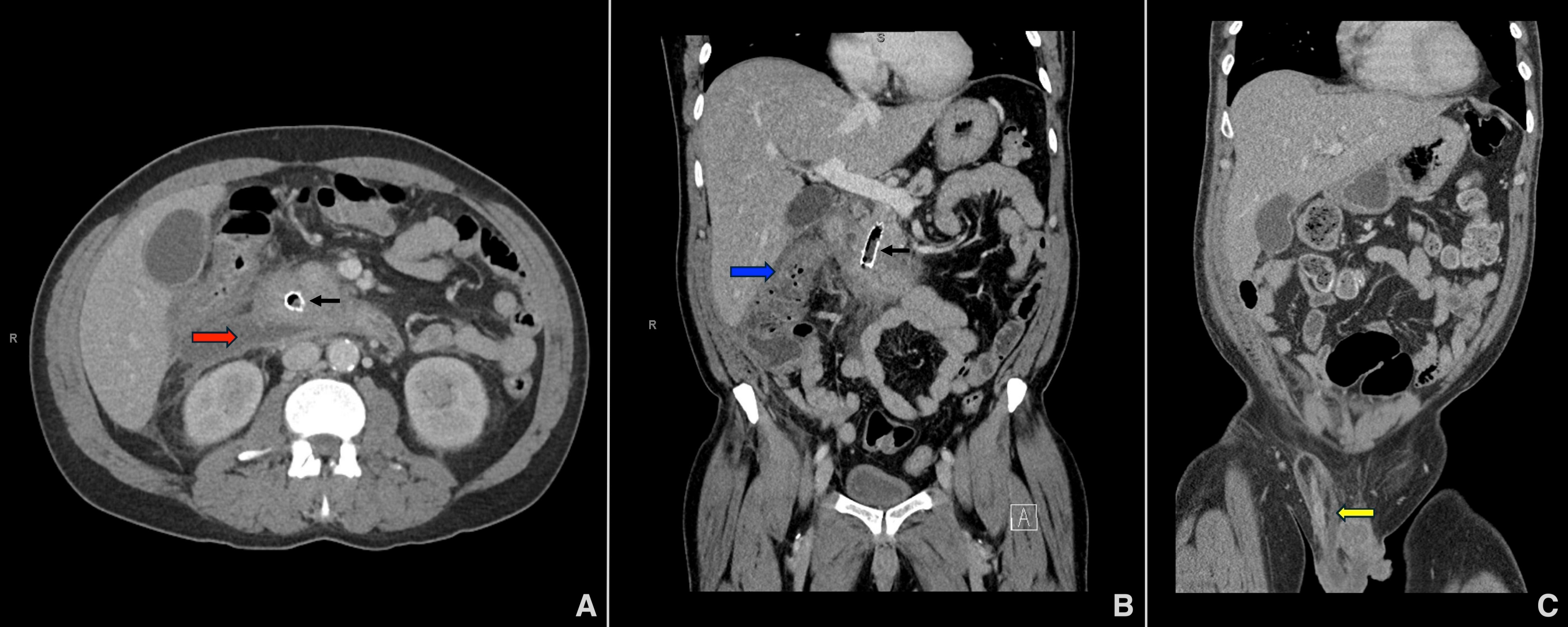
Figure: Figure 1: Multiple CT scans revealed extensive abscesses, including (A) an infected peripancreatic acute necrotic collection (red arrow), (B) duodenitis and colitis at the hepatic flexure (blue arrow) extending into the region of the cecum and the right hemiscrotum, resulting in (C) an abscess in the inguinal canal and spermatic cord (yellow arrow). The FCSEMS is also visible (black arrows).

Figure: Figure 2: In the course of the endoscopic retrograde cholangiopancreatography, (A) the FCSEMS (Viabil®, W.L. Gore & Associates, Flagstaff, AZ, USA) was found to be fully obstructed with food, pus, and debris. (B) Following the clearance of all obstructions using a balloon, the FCSEMS was successfully extracted. (C) Subsequently, two short 7 Fr unflanged plastic stents, each with a complete external pigtail, (Hobbs Medical, Stafford Springs, CT, USA) were inserted into the main pancreatic duct.
Disclosures:
Jameel Alp indicated no relevant financial relationships.
James Mallery indicated no relevant financial relationships.
Guru Trikudanathan: AbbVie – Grant/Research Support. Boston Scientific – Consultant.
Martin Freeman indicated no relevant financial relationships.
Jameel Alp, MD, James Mallery, MD, Guru Trikudanathan, MD, Martin Freeman, MD. P0160 - From Pancreas to Groin: Scrotal Abscess Following Pancreatic Fully Covered Self-Expandable Metal Stent Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

