Sunday Poster Session
Category: Biliary/Pancreas
P0146 - When Lymphoma Meets the Pancreas: A Case of Burkitt's in an Unlikely Location
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- DB
David W. Berry, DO
East Tennessee State University
Johnson City, VA
Presenting Author(s)
David W. Berry, DO1, McKenna Andrews, MD2, Syed Madeeha Sadiq, DO3, Noah Hall, MD4
1East Tennessee State University, Johnson City, TN; 2East Tennessee State University, Kingsport, TN; 3ETSU Gastroenterology, Kingsport, TN; 4Mountain Home VA Medical Center, Jonesborough, TN
Introduction: Pancreatic cancer is the third leading cause of cancer-related death in the U.S., with most cases diagnosed at advanced stages. Pancreatic ductal adenocarcinoma (PDAC) accounts for over 90% of cases. In contrast, primary pancreatic lymphoma is rare (< 0.5% of pancreatic malignancies), with diffuse large B-cell lymphoma being most common. We present a rare case of primary pancreatic Burkitt lymphoma, highlighting its aggressive nature and strikingly rapid progression.
Case Description/
Methods: A 68-year-old male with a history of pancreatitis, hypertension, and prior splenectomy presented to the emergency room due to abnormal computed tomography imaging (Fig. 1) and ongoing epigastric pain, nausea, and fatigue. On presentation, he was hemodynamically stable with scleral icterus and epigastric tenderness noted on exam. Initial labs favored a cholestatic pattern of liver injury with a total bilirubin of 6.4 mg/dL and alkaline phosphatase of 588 U/L. Abdominal magnetic resonance imaging (MRI) revealed a pancreatic head mass measuring 5.9 x 5.9 cm.
He underwent endoscopic retrograde cholangiopancreatography (ERCP) for stent placement due to obstructive jaundice and an endoscopic ultrasound-guided biopsy of the pancreatic mass. Despite intervention, his liver enzymes worsened. Repeat MRI two weeks later showed rapid disease progression with mass growth, regional invasion, and increased nodal and metastatic burden. A repeat endoscopy (Fig. 2) revealed a severe duodenal stricture and biliary stent migration requiring repositioning. Biopsy confirmed Burkitt lymphoma. Due to rapid clinical decline, the patient opted for comfort care and passed away shortly thereafter.
Discussion: This case highlights a rare presentation of Burkitt lymphoma with primary pancreatic involvement. Rapid mass enlargement, duodenal stricture formation, and widespread disease in less than three weeks underscores its aggressiveness. Initial endoscopy noted edema in the second portion of the duodenum, which progressed to a tight, infiltrative stricture within six days.
Unlike PDAC, pancreatic lymphomas are often chemosensitive and potentially curable, but timely recognition is essential. Rapidly growing pancreatic lesions with unusual characteristics should prompt consideration of alternative diagnoses, including lymphoma, as illustrated by this case. Early biopsy and diagnosis can significantly impact treatment, particularly in frail patients where delays may preclude curative therapy.
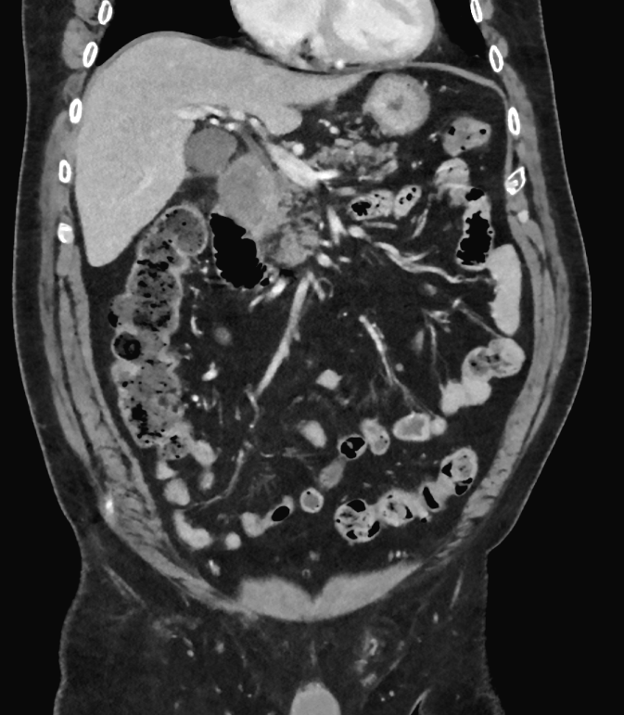
Figure: Fig 1. Coronal contrast-enhanced abdominal CT showing an ill-defined pancreatic head mass (3.8 x 3.4cm) abutting the duodenum and likely involving the common bile duct.
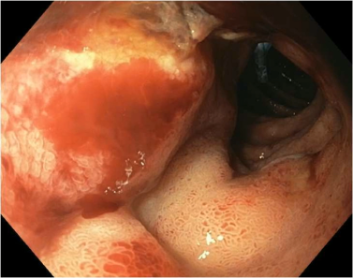
Figure: Fig 2. Upper gastrointestinal endoscopy demonstrating a tight duodenal stricture involving the duodenal sweep and proximal second portion of the duodenum.
Disclosures:
David Berry indicated no relevant financial relationships.
McKenna Andrews indicated no relevant financial relationships.
Syed Madeeha Sadiq indicated no relevant financial relationships.
Noah Hall indicated no relevant financial relationships.
David W. Berry, DO1, McKenna Andrews, MD2, Syed Madeeha Sadiq, DO3, Noah Hall, MD4. P0146 - When Lymphoma Meets the Pancreas: A Case of Burkitt's in an Unlikely Location, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1East Tennessee State University, Johnson City, TN; 2East Tennessee State University, Kingsport, TN; 3ETSU Gastroenterology, Kingsport, TN; 4Mountain Home VA Medical Center, Jonesborough, TN
Introduction: Pancreatic cancer is the third leading cause of cancer-related death in the U.S., with most cases diagnosed at advanced stages. Pancreatic ductal adenocarcinoma (PDAC) accounts for over 90% of cases. In contrast, primary pancreatic lymphoma is rare (< 0.5% of pancreatic malignancies), with diffuse large B-cell lymphoma being most common. We present a rare case of primary pancreatic Burkitt lymphoma, highlighting its aggressive nature and strikingly rapid progression.
Case Description/
Methods: A 68-year-old male with a history of pancreatitis, hypertension, and prior splenectomy presented to the emergency room due to abnormal computed tomography imaging (Fig. 1) and ongoing epigastric pain, nausea, and fatigue. On presentation, he was hemodynamically stable with scleral icterus and epigastric tenderness noted on exam. Initial labs favored a cholestatic pattern of liver injury with a total bilirubin of 6.4 mg/dL and alkaline phosphatase of 588 U/L. Abdominal magnetic resonance imaging (MRI) revealed a pancreatic head mass measuring 5.9 x 5.9 cm.
He underwent endoscopic retrograde cholangiopancreatography (ERCP) for stent placement due to obstructive jaundice and an endoscopic ultrasound-guided biopsy of the pancreatic mass. Despite intervention, his liver enzymes worsened. Repeat MRI two weeks later showed rapid disease progression with mass growth, regional invasion, and increased nodal and metastatic burden. A repeat endoscopy (Fig. 2) revealed a severe duodenal stricture and biliary stent migration requiring repositioning. Biopsy confirmed Burkitt lymphoma. Due to rapid clinical decline, the patient opted for comfort care and passed away shortly thereafter.
Discussion: This case highlights a rare presentation of Burkitt lymphoma with primary pancreatic involvement. Rapid mass enlargement, duodenal stricture formation, and widespread disease in less than three weeks underscores its aggressiveness. Initial endoscopy noted edema in the second portion of the duodenum, which progressed to a tight, infiltrative stricture within six days.
Unlike PDAC, pancreatic lymphomas are often chemosensitive and potentially curable, but timely recognition is essential. Rapidly growing pancreatic lesions with unusual characteristics should prompt consideration of alternative diagnoses, including lymphoma, as illustrated by this case. Early biopsy and diagnosis can significantly impact treatment, particularly in frail patients where delays may preclude curative therapy.
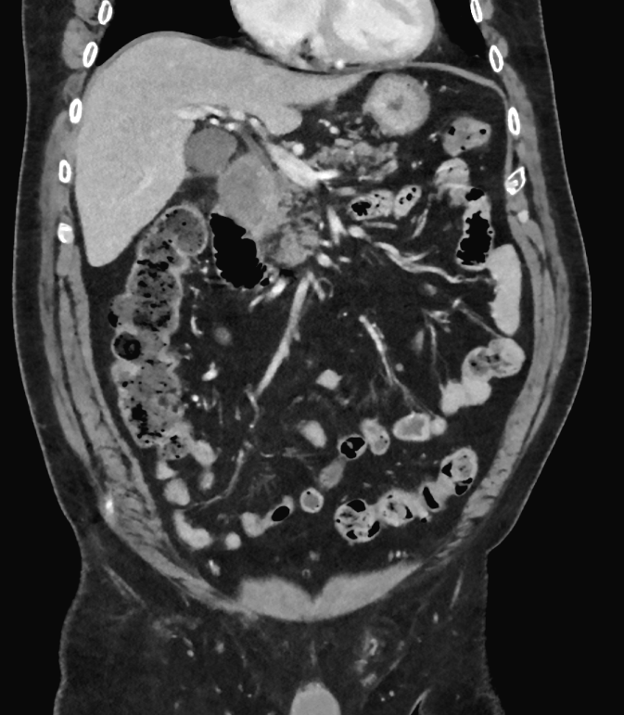
Figure: Fig 1. Coronal contrast-enhanced abdominal CT showing an ill-defined pancreatic head mass (3.8 x 3.4cm) abutting the duodenum and likely involving the common bile duct.
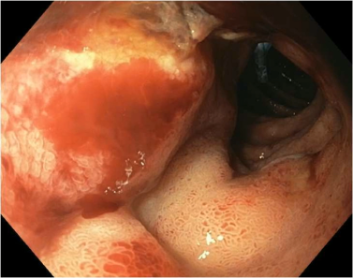
Figure: Fig 2. Upper gastrointestinal endoscopy demonstrating a tight duodenal stricture involving the duodenal sweep and proximal second portion of the duodenum.
Disclosures:
David Berry indicated no relevant financial relationships.
McKenna Andrews indicated no relevant financial relationships.
Syed Madeeha Sadiq indicated no relevant financial relationships.
Noah Hall indicated no relevant financial relationships.
David W. Berry, DO1, McKenna Andrews, MD2, Syed Madeeha Sadiq, DO3, Noah Hall, MD4. P0146 - When Lymphoma Meets the Pancreas: A Case of Burkitt's in an Unlikely Location, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
