Sunday Poster Session
Category: Biliary/Pancreas
P0117 - Hereditary Chronic Pancreatitis in a Guatemalan Adolescent: Genetic Diagnosis in a Resource-Limited Setting
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Abel Sanchez, MD, MSc (he/him/his)
Hospital Roosevelt / Gastri-k
Guatemala City, San Marcos, Guatemala
Presenting Author(s)
Bryan Torres, MD1, Kenia Santos, 2, Rafael Orellana, 2, Abel Sanchez, MD, MSc3
1Gastroenterology & Digestive Endoscopy Unit, Roosevelt Hospital, University of San Carlos of Guatemala, Guatemala City, Quetzaltenango, Guatemala; 2Gastroenterology & Digestive Endoscopy Unit, Roosevelt Hospital, University of San Carlos of Guatemala, Guatemala City, Chimaltenango, Guatemala; 3Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction: Hereditary chronic pancreatitis (HCP) is a rare form of chronic pancreatitis associated with PRSS1 gene mutations, typically presenting in childhood. Timely genetic confirmation is challenging in low-resource countries, where limited access to molecular testing may delay diagnosis
Case Description/
Methods: A 14-year-old girl from Guatemala presented to our public tertiary gastroenterology clinic with recurrent episodes of acute pancreatitis since early adolescence. She reported epigastric pain radiating to the back, nausea, and vomiting. Physical examination was unremarkable. Initial lab testing revealed lipase 207 U/L, normal triglycerides and calcium, and no evidence of infection or autoimmune markers. Prior abdominal ultrasound and MRCP were normal. EGD showed hiatal insufficiency and mild gastritis. Cross-sectional imaging ruled out structural causes. Endoscopic ultrasound revealed parenchymal pseudolobulation, hyperechoic strands and foci, and hyperechoic main duct margins—meeting four Rosemont criteria for chronic pancreatitis. Genetic consultation recommended testing for hereditary pancreatitis. A panel revealed a PRSS1 gene mutation, confirming the diagnosis of hereditary chronic pancreatitis. The patient is currently asymptomatic and is under outpatient surveillance for long-term complications
Discussion: This case demonstrates the diagnostic complexity of HCP in resource-limited settings. Despite the rarity of PRSS1 mutations, high clinical suspicion guided the appropriate use of EUS and genetic testing. Early identification allows for monitoring of endocrine and exocrine insufficiency and pancreatic cancer risk. This report underscores the need to increase awareness of HCP and to improve access to genetic testing in developing countries. It also highlights the role of sequential, cost-effective diagnostic steps to reach definitive diagnoses even when high-end resources are scarce
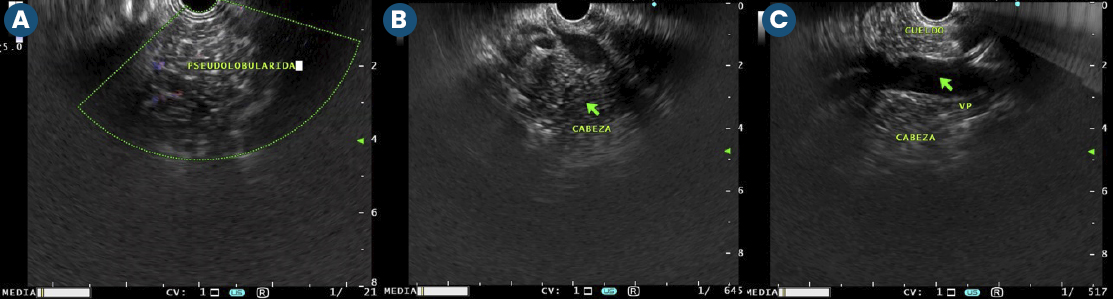
Figure: Figure 1. Endoscopic ultrasound (EUS) images showing parenchymal and ductal changes consistent with chronic pancreatitis. A: Pseudolobular pattern with hyperechoic strands. B: Hyperechoic foci and lobularity in the pancreatic head. C: Hyperechoic main pancreatic duct wall and irregular contour (CBD: common bile duct; VP: portal vein). These findings meet four Rosemont criteria for chronic pancreatitis.
Disclosures:
Bryan Torres indicated no relevant financial relationships.
Kenia Santos indicated no relevant financial relationships.
Rafael Orellana indicated no relevant financial relationships.
Abel Sanchez indicated no relevant financial relationships.
Bryan Torres, MD1, Kenia Santos, 2, Rafael Orellana, 2, Abel Sanchez, MD, MSc3. P0117 - Hereditary Chronic Pancreatitis in a Guatemalan Adolescent: Genetic Diagnosis in a Resource-Limited Setting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Gastroenterology & Digestive Endoscopy Unit, Roosevelt Hospital, University of San Carlos of Guatemala, Guatemala City, Quetzaltenango, Guatemala; 2Gastroenterology & Digestive Endoscopy Unit, Roosevelt Hospital, University of San Carlos of Guatemala, Guatemala City, Chimaltenango, Guatemala; 3Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction: Hereditary chronic pancreatitis (HCP) is a rare form of chronic pancreatitis associated with PRSS1 gene mutations, typically presenting in childhood. Timely genetic confirmation is challenging in low-resource countries, where limited access to molecular testing may delay diagnosis
Case Description/
Methods: A 14-year-old girl from Guatemala presented to our public tertiary gastroenterology clinic with recurrent episodes of acute pancreatitis since early adolescence. She reported epigastric pain radiating to the back, nausea, and vomiting. Physical examination was unremarkable. Initial lab testing revealed lipase 207 U/L, normal triglycerides and calcium, and no evidence of infection or autoimmune markers. Prior abdominal ultrasound and MRCP were normal. EGD showed hiatal insufficiency and mild gastritis. Cross-sectional imaging ruled out structural causes. Endoscopic ultrasound revealed parenchymal pseudolobulation, hyperechoic strands and foci, and hyperechoic main duct margins—meeting four Rosemont criteria for chronic pancreatitis. Genetic consultation recommended testing for hereditary pancreatitis. A panel revealed a PRSS1 gene mutation, confirming the diagnosis of hereditary chronic pancreatitis. The patient is currently asymptomatic and is under outpatient surveillance for long-term complications
Discussion: This case demonstrates the diagnostic complexity of HCP in resource-limited settings. Despite the rarity of PRSS1 mutations, high clinical suspicion guided the appropriate use of EUS and genetic testing. Early identification allows for monitoring of endocrine and exocrine insufficiency and pancreatic cancer risk. This report underscores the need to increase awareness of HCP and to improve access to genetic testing in developing countries. It also highlights the role of sequential, cost-effective diagnostic steps to reach definitive diagnoses even when high-end resources are scarce
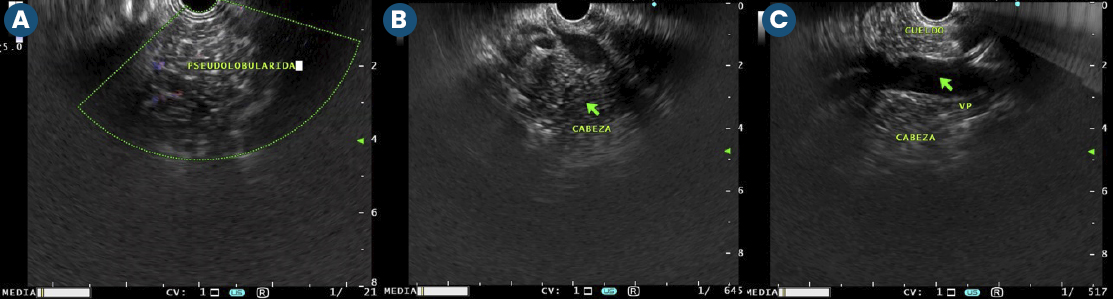
Figure: Figure 1. Endoscopic ultrasound (EUS) images showing parenchymal and ductal changes consistent with chronic pancreatitis. A: Pseudolobular pattern with hyperechoic strands. B: Hyperechoic foci and lobularity in the pancreatic head. C: Hyperechoic main pancreatic duct wall and irregular contour (CBD: common bile duct; VP: portal vein). These findings meet four Rosemont criteria for chronic pancreatitis.
Disclosures:
Bryan Torres indicated no relevant financial relationships.
Kenia Santos indicated no relevant financial relationships.
Rafael Orellana indicated no relevant financial relationships.
Abel Sanchez indicated no relevant financial relationships.
Bryan Torres, MD1, Kenia Santos, 2, Rafael Orellana, 2, Abel Sanchez, MD, MSc3. P0117 - Hereditary Chronic Pancreatitis in a Guatemalan Adolescent: Genetic Diagnosis in a Resource-Limited Setting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
