Sunday Poster Session
Category: Biliary/Pancreas
P0108 - Histological Mimicry of Autoimmune Pancreatitis in a Case of Pancreatic Adenocarcinoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tasneem Jamal Al-Din, MD
Cleveland Clinic Florida
Weston, FL
Presenting Author(s)
Tasneem Jamal Al-Din, MD, Zaid Ansari, MD, Akram Ahmad, MD, Tilak Shah, MD
Cleveland Clinic Florida, Weston, FL
Introduction: Differentiating autoimmune pancreatitis (AIP) from pancreatic cancer (PC) poses significant challenges due to overlapping clinical, serological, and imaging features. Both may present with painless jaundice, weight loss, new-onset diabetes, and a pancreatic mass, making initial clinical distinction difficult. We present a case of pancreatic adenocarcinoma initially misdiagnosed as AIP based on imaging and histopathology.
Case Description/
Methods: A 71-year-old female with a known history of ulcerative colitis (on mesalamine) presented with two months of dull epigastric pain without weight loss or jaundice. She consumed 1–2 glasses of wine daily and was a former smoker. Labs revealed elevated lipase (220 U/L), but normal CBC, CMP, and IgG4. Contrast-enhanced CT showed a diffusely enlarged pancreas without a mass or ductal dilation (Figure1). Given the diagnostic uncertainty, Endoscopic ultrasound (EUS) was performed demonstrating diffuse hypoechogenicity with mass-like features (Figure2). Fine needle biopsy (FNB) revealed lymphoplasmacytic infiltration with sclerosis and myxoid changes, suggestive of AIP. She was started on prednisone 40 mg daily for 4 weeks. Symptoms improved, but follow-up CT showed pancreatic atrophy and irregular ductal dilation (Figure3). CA 19-9 was elevated at 196. Repeat EUS identified a poorly defined, 30×24 mm hypoechoic mass in the pancreatic head (Figure4). FNB confirmed pancreatic adenocarcinoma. She underwent laparoscopic pancreaticoduodenectomy with cholecystectomy. Pathology confirmed adenocarcinoma with perineural and lymphovascular invasion and metastases in 9 of 13 lymph nodes.
Discussion: Initial findings including subacute pain, elevated lipase, and diffuse pancreatic changes were consistent with AIP. Despite normal IgG4, 20–25% of AIP cases show normal levels, especially in type 2 AIP, which is associated with inflammatory bowel disease. Steroid response was partial, raising suspicion for malignancy. AIP usually responds rapidly to steroids (~97% response rate). Progression of imaging and tumor marker elevation prompted repeat evaluation and diagnosis of adenocarcinoma. AIP accounts for 1.6% of resected cases initially suspected to be PC, and up to 9.5% of PC cases may show AIP-like histology. This case highlights the diagnostic complexity and need for close follow-up in suspected AIP. Clinicians should maintain a high index of suspicion and pursue repeat evaluation if clinical or radiologic findings worsen despite therapy.
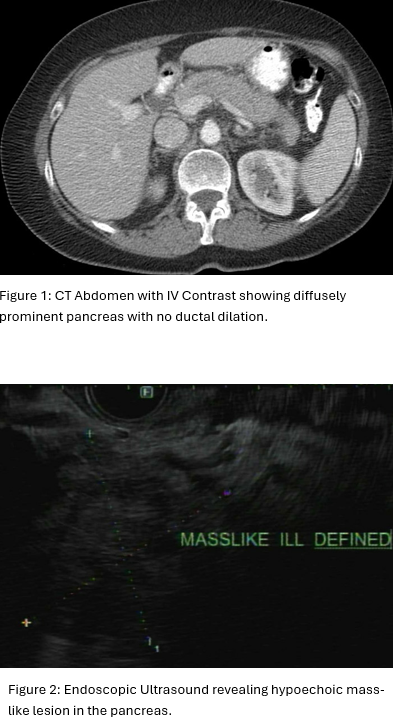
Figure: Figure 1 and Figure 2
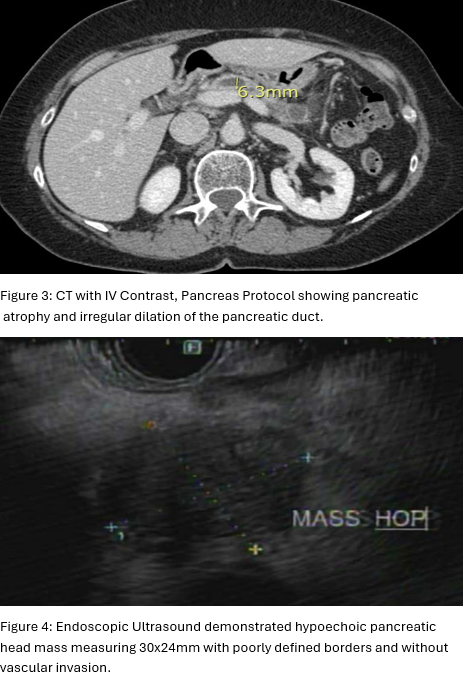
Figure: Figure 3 and 4
Disclosures:
Tasneem Jamal Al-Din indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Tilak Shah: Steris – Consultant.
Tasneem Jamal Al-Din, MD, Zaid Ansari, MD, Akram Ahmad, MD, Tilak Shah, MD. P0108 - Histological Mimicry of Autoimmune Pancreatitis in a Case of Pancreatic Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Cleveland Clinic Florida, Weston, FL
Introduction: Differentiating autoimmune pancreatitis (AIP) from pancreatic cancer (PC) poses significant challenges due to overlapping clinical, serological, and imaging features. Both may present with painless jaundice, weight loss, new-onset diabetes, and a pancreatic mass, making initial clinical distinction difficult. We present a case of pancreatic adenocarcinoma initially misdiagnosed as AIP based on imaging and histopathology.
Case Description/
Methods: A 71-year-old female with a known history of ulcerative colitis (on mesalamine) presented with two months of dull epigastric pain without weight loss or jaundice. She consumed 1–2 glasses of wine daily and was a former smoker. Labs revealed elevated lipase (220 U/L), but normal CBC, CMP, and IgG4. Contrast-enhanced CT showed a diffusely enlarged pancreas without a mass or ductal dilation (Figure1). Given the diagnostic uncertainty, Endoscopic ultrasound (EUS) was performed demonstrating diffuse hypoechogenicity with mass-like features (Figure2). Fine needle biopsy (FNB) revealed lymphoplasmacytic infiltration with sclerosis and myxoid changes, suggestive of AIP. She was started on prednisone 40 mg daily for 4 weeks. Symptoms improved, but follow-up CT showed pancreatic atrophy and irregular ductal dilation (Figure3). CA 19-9 was elevated at 196. Repeat EUS identified a poorly defined, 30×24 mm hypoechoic mass in the pancreatic head (Figure4). FNB confirmed pancreatic adenocarcinoma. She underwent laparoscopic pancreaticoduodenectomy with cholecystectomy. Pathology confirmed adenocarcinoma with perineural and lymphovascular invasion and metastases in 9 of 13 lymph nodes.
Discussion: Initial findings including subacute pain, elevated lipase, and diffuse pancreatic changes were consistent with AIP. Despite normal IgG4, 20–25% of AIP cases show normal levels, especially in type 2 AIP, which is associated with inflammatory bowel disease. Steroid response was partial, raising suspicion for malignancy. AIP usually responds rapidly to steroids (~97% response rate). Progression of imaging and tumor marker elevation prompted repeat evaluation and diagnosis of adenocarcinoma. AIP accounts for 1.6% of resected cases initially suspected to be PC, and up to 9.5% of PC cases may show AIP-like histology. This case highlights the diagnostic complexity and need for close follow-up in suspected AIP. Clinicians should maintain a high index of suspicion and pursue repeat evaluation if clinical or radiologic findings worsen despite therapy.
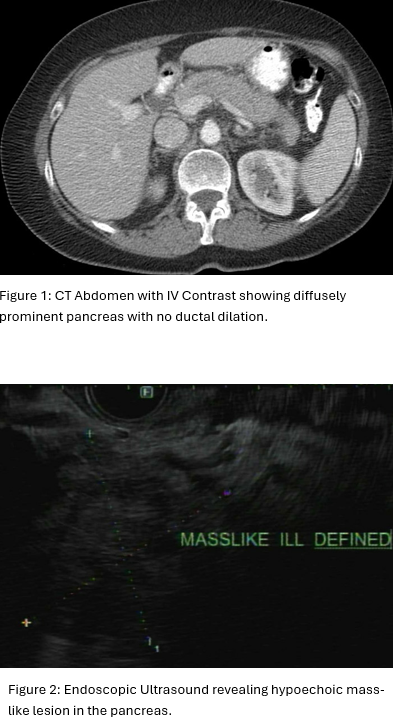
Figure: Figure 1 and Figure 2
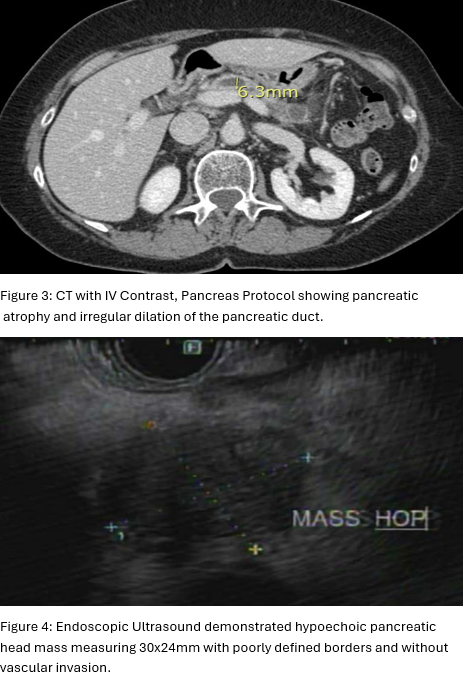
Figure: Figure 3 and 4
Disclosures:
Tasneem Jamal Al-Din indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Tilak Shah: Steris – Consultant.
Tasneem Jamal Al-Din, MD, Zaid Ansari, MD, Akram Ahmad, MD, Tilak Shah, MD. P0108 - Histological Mimicry of Autoimmune Pancreatitis in a Case of Pancreatic Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
