Sunday Poster Session
Category: Biliary/Pancreas
P0093 - Can We Walk Away From Pancreatic Duct Stents? Assessing Frequency, Predictors, and Need for Endoscopic Removal
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Xiang Yu Gao, BS (he/him/his)
Washington State University Elson S. Floyd School of Medicine
Spokane Valley, WA
Presenting Author(s)
Xiang Yu Gao, BS1, Nishant Puri, MD, FACG2, Jack Brandabur, MD3, Wichit Srikureja, MD4, Divyanshoo Kohli, MD, FACG2
1Washington State University Elson S. Floyd School of Medicine, Spokane Valley, WA; 2Washington State University Elson S. Floyd School of Medicine, Spokane, WA; 3Prosser Memorial Health, Prosser, WA; 4Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Pancreatic duct (PD) stents are often placed with the intent of spontaneous passage or prolonged retention. We assessed the frequency and risk factors associated with spontaneous migration or inappropriate retention of PD stents after 4 weeks of endoscopic retrograde cholangiopancreatography (ERCP).
Methods: Consecutive patients who underwent ERCP with PD stent placement at our tertiary care center from 2019 through 2024 were identified and categorized into those with retention or spontaneous migration at 4 weeks after ERCP. All patients were contacted to ensure compliance with follow up imaging or procedures. PD stents without an internal flange were presumed to be placed with the intent of spontaneous passage. Spontaneous passage was defined by the absence of PD stent on imaging performed within 4 weeks. Inappropriate retention was defined by the presence of a non-flanged PD stent within the PD seen on imaging after 4 weeks of ERCP. Primary endpoint was PD stent retention 4 weeks after ERCP. Secondary endpoints included risk factors for retention and need for endoscopic removal of PD stents.
Results: Of the 501 patients who met selection criteria, 482 patients underwent ERCP for biliary (289), pancreatic (181), or both biliary and pancreatic (12) indications (Figure 1). PD stents without internal flanges were used more frequently for biliary indications vs pancreatic indications (74.4% vs 31.5%, P< 0.001). Follow-up in 425 patients demonstrated that retention of PD stents occurred more frequently in the presence of internal flanges, ERCP performed for pancreatic disorders, and greater stent length and diameter (Table 1). Post-ERCP adverse events were similar in both groups.
Inappropriate retention of stents without an internal flange occurred in 29 (12.5%) patients, and only 5 (2%) required endoscopic removal (Figure 1). These 5 patients had a concomitant covered metal stent in the bile duct (n=3), anomalous pancreas-biliary junction (1), or a transgastric jejunal feeding tube traversing the ampulla (1).
Discussion: The frequency of inappropriate retention of PD stents without internal flange is low, occurs due the mechanical obstruction at the ampulla, and requires endoscopic removal very rarely. A single, thin, short, PD stent without an internal flange has a minimal risk of inappropriate retention.
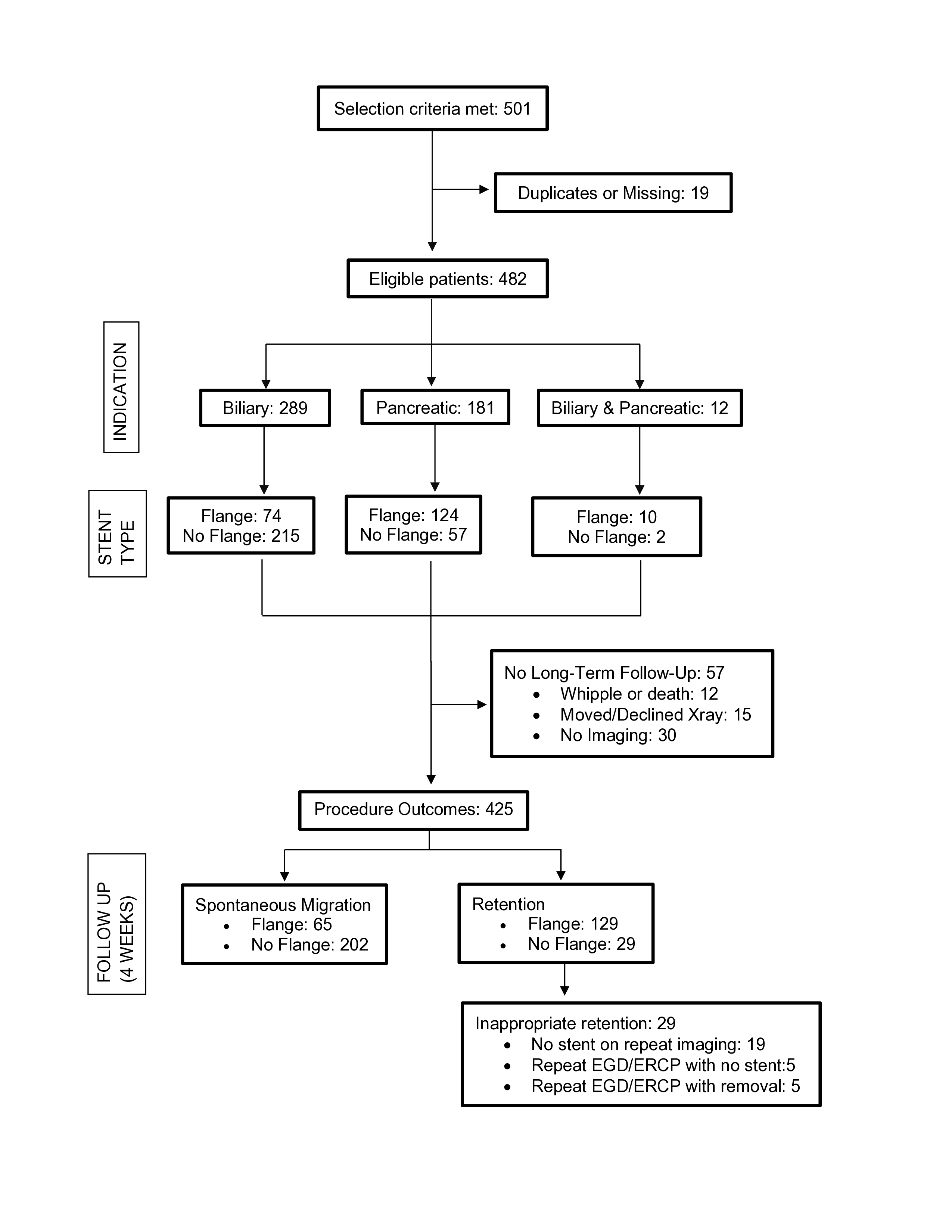
Figure: Figure 1. Flowchart of patients and ouctomes
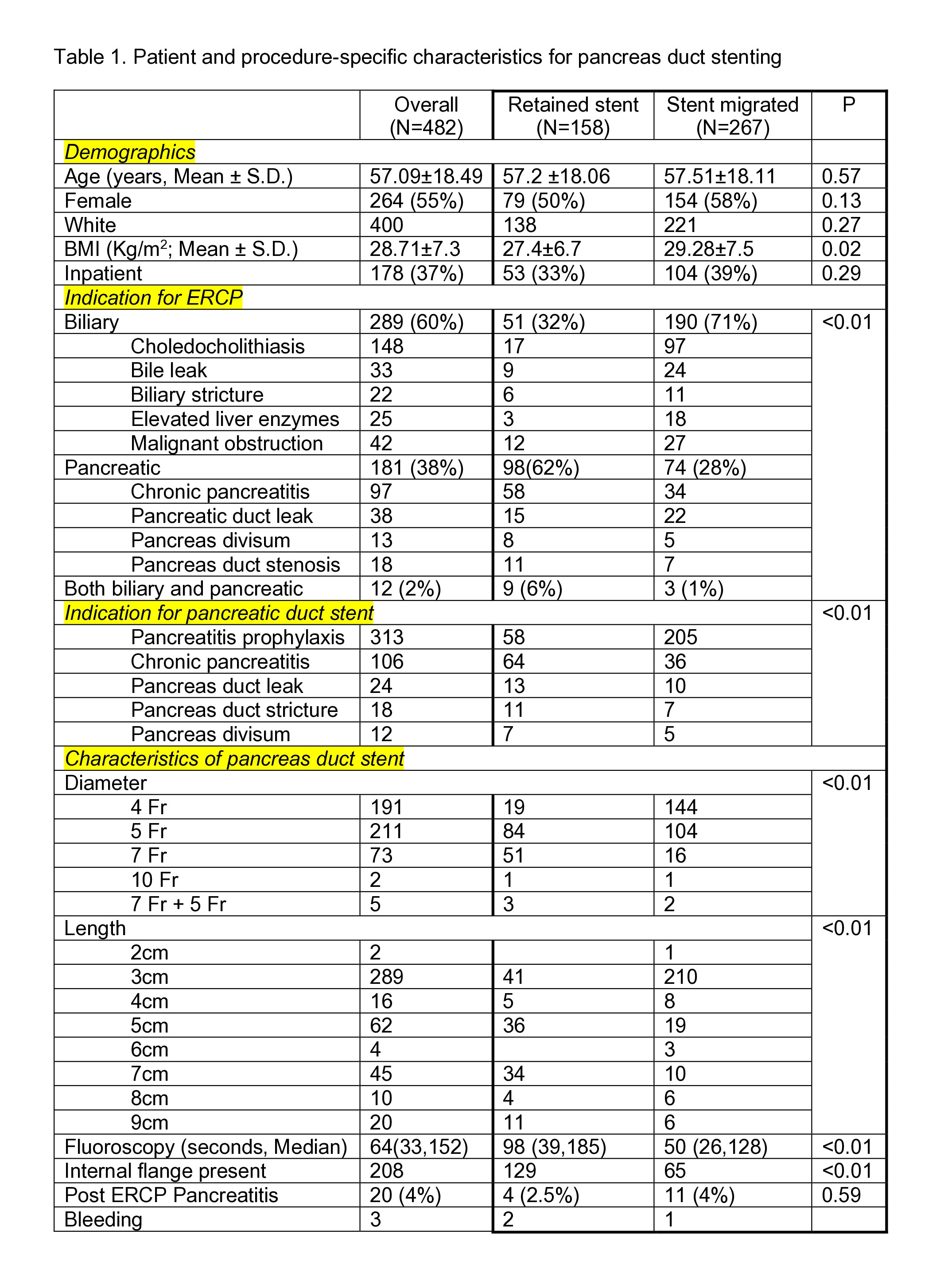
Figure: Table 1. Patient and procedure-specific characteristics for pancreas duct stenting
Disclosures:
Xiang Yu Gao indicated no relevant financial relationships.
Nishant Puri indicated no relevant financial relationships.
Jack Brandabur indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Divyanshoo Kohli: American Board of Internal Medicine – Advisory Committee/Board Member. Fujifilm – Grant/Research Support. Olympus Corporation of the Americas – Consultant.
Xiang Yu Gao, BS1, Nishant Puri, MD, FACG2, Jack Brandabur, MD3, Wichit Srikureja, MD4, Divyanshoo Kohli, MD, FACG2. P0093 - Can We Walk Away From Pancreatic Duct Stents? Assessing Frequency, Predictors, and Need for Endoscopic Removal, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Washington State University Elson S. Floyd School of Medicine, Spokane Valley, WA; 2Washington State University Elson S. Floyd School of Medicine, Spokane, WA; 3Prosser Memorial Health, Prosser, WA; 4Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Pancreatic duct (PD) stents are often placed with the intent of spontaneous passage or prolonged retention. We assessed the frequency and risk factors associated with spontaneous migration or inappropriate retention of PD stents after 4 weeks of endoscopic retrograde cholangiopancreatography (ERCP).
Methods: Consecutive patients who underwent ERCP with PD stent placement at our tertiary care center from 2019 through 2024 were identified and categorized into those with retention or spontaneous migration at 4 weeks after ERCP. All patients were contacted to ensure compliance with follow up imaging or procedures. PD stents without an internal flange were presumed to be placed with the intent of spontaneous passage. Spontaneous passage was defined by the absence of PD stent on imaging performed within 4 weeks. Inappropriate retention was defined by the presence of a non-flanged PD stent within the PD seen on imaging after 4 weeks of ERCP. Primary endpoint was PD stent retention 4 weeks after ERCP. Secondary endpoints included risk factors for retention and need for endoscopic removal of PD stents.
Results: Of the 501 patients who met selection criteria, 482 patients underwent ERCP for biliary (289), pancreatic (181), or both biliary and pancreatic (12) indications (Figure 1). PD stents without internal flanges were used more frequently for biliary indications vs pancreatic indications (74.4% vs 31.5%, P< 0.001). Follow-up in 425 patients demonstrated that retention of PD stents occurred more frequently in the presence of internal flanges, ERCP performed for pancreatic disorders, and greater stent length and diameter (Table 1). Post-ERCP adverse events were similar in both groups.
Inappropriate retention of stents without an internal flange occurred in 29 (12.5%) patients, and only 5 (2%) required endoscopic removal (Figure 1). These 5 patients had a concomitant covered metal stent in the bile duct (n=3), anomalous pancreas-biliary junction (1), or a transgastric jejunal feeding tube traversing the ampulla (1).
Discussion: The frequency of inappropriate retention of PD stents without internal flange is low, occurs due the mechanical obstruction at the ampulla, and requires endoscopic removal very rarely. A single, thin, short, PD stent without an internal flange has a minimal risk of inappropriate retention.
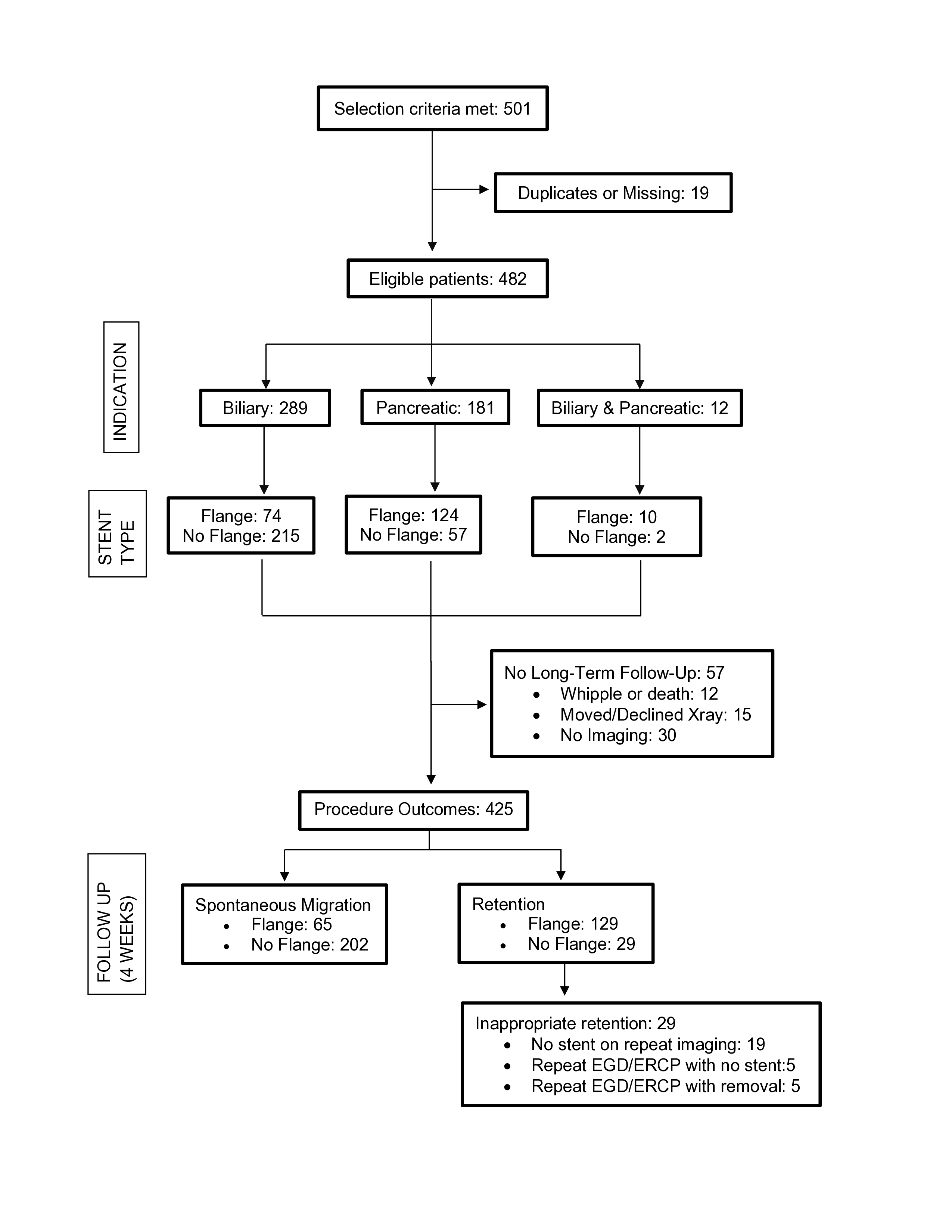
Figure: Figure 1. Flowchart of patients and ouctomes
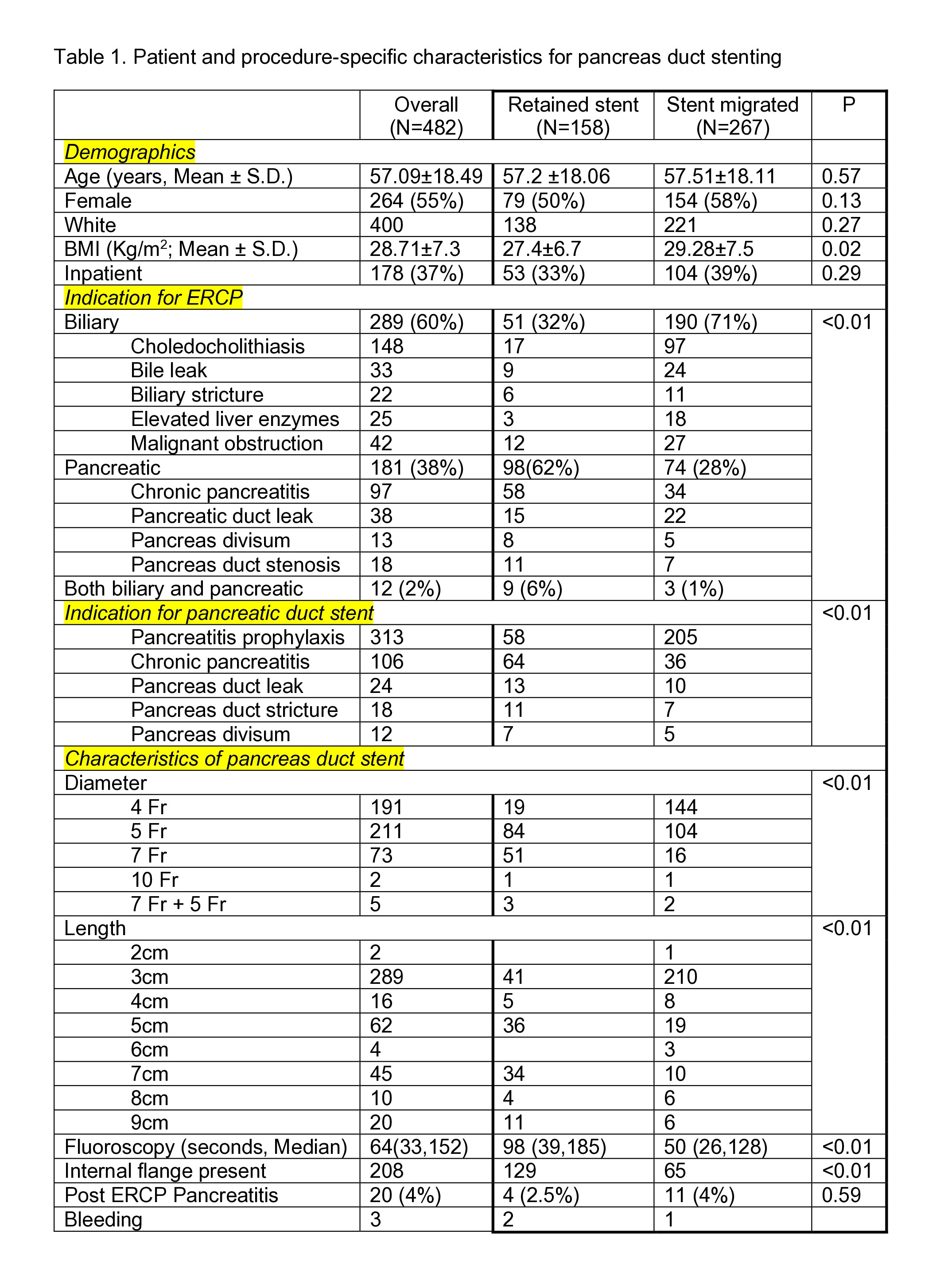
Figure: Table 1. Patient and procedure-specific characteristics for pancreas duct stenting
Disclosures:
Xiang Yu Gao indicated no relevant financial relationships.
Nishant Puri indicated no relevant financial relationships.
Jack Brandabur indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Divyanshoo Kohli: American Board of Internal Medicine – Advisory Committee/Board Member. Fujifilm – Grant/Research Support. Olympus Corporation of the Americas – Consultant.
Xiang Yu Gao, BS1, Nishant Puri, MD, FACG2, Jack Brandabur, MD3, Wichit Srikureja, MD4, Divyanshoo Kohli, MD, FACG2. P0093 - Can We Walk Away From Pancreatic Duct Stents? Assessing Frequency, Predictors, and Need for Endoscopic Removal, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

