Sunday Poster Session
Category: Biliary/Pancreas
P0090 - Deep Learning for Lymph Node Detection and Malignancy Risk Stratification in EUS: A Multicenter Proof of Concept Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MM
Miguel Martins, MD (he/him/his)
Centro Hospitalar Universitário São João
Porto, Porto, Portugal
Presenting Author(s)
Award: ACG Presidential Poster Award
Miguel Martins, MD1, Miguel Mascarenhas Saraiva, MD, PhD1, Belen Agudo, MD2, Francisco Mendes, MD1, António Costa, MD2, Tiago Ribeiro, MD1, Joana Mota, MD1, Maria João Almeida, MD3, Pedro Cardoso, MD1, João Afonso, MD1, Daniel De la Iglesia Garcia, MD, PhD2, Carlos Esteban Fernández-Zarza, MD2, Ana Garcia Garcia de Paredes, MD4, Maria Moris, MD5, Matheus Ferreira de Carvalho, MD6, Marcos Eduardo Lera dos Santos, MD6, João Ferreira, PhD7, Jessica Widmer, DO8, Filipe Vilas Boas, MD, PhD3, Pedro Moutinho Ribeiro, MD, PhD3, Susana Lopes, MD, PhD3, Mariano Gonzalez Haba, MD2, Eduardo Hourneaux De Moura, MD, PhD9, Guilherme Macedo, MD, PhD1
1Centro Hospitalar Universitário São João, Porto, Porto, Portugal; 2Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Madrid, Spain; 3Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 4Hospital Universitario Ramón y Cajal, Madrid, Madrid, Spain; 5Hospital Universitario Marqués de Valdecilla, GI, Santander, Spain,, Santander, Cantabria, Spain; 6Hospital das Clínicas da Faculdade de Medicina da Universidade de Sao Paulo, São Paulo, Sao Paulo, Brazil; 7Faculdade de Engenharia da Universidade do Porto, Porto, Porto, Portugal; 8NYU Langone Health, Mineola, NY; 9Hospital das Clínicas da Faculdade de Medicina da USP, São Paulo, Sao Paulo, Brazil
Introduction: Endoscopic ultrasound (EUS) is important for accurate lymph node (LN) characterization, being essential to guide treatment in suspected malignant involvement. Features like hypoechoic structures, sharply demarcated borders, rounded contours and size over 10 mm suggest malignancy, with 80-100% accuracy when combined, but this complete profile is uncommon. While EUS-guided fineneedle aspiration/biopsy (FNA/FNB) aids diagnosis, its accuracy can be limited. Artificial intelligence (AI) shows potential in improving diagnostic precision in EUS. However, data on convolutional neural network (CNN) application to EUS for LN malignancy prediction remains scarce. This multicenter study aims to evaluate a CNN’s effectiveness in predicting LN malignancy from EUS images.
Methods: This multicenter study included EUS images from nine centers and four countries. Lesions were classified as malignant or benign and delimited with bounding boxes. Definitive diagnoses were based on positive FNA/FNB or surgical specimen and, if negative, a minimum six-month clinical follow-up was required. A CNN was developed including both detection and characterization modules. Performance metrics included detection rate (DR), sensitivity, specificity, accuracy, and AUC were calculated.
Results: 59988 images from 108 patients were used to develop the model. The CNN distinguished malignant from benign LNs with a sensitivity of 93.7%, a specificity of 98.3% and an overall accuracy of 95.8%. The AUC was 0.95.
Discussion: To our knowledge, this study is one of the first to evaluate the performance of deep learning systems for LN assessment using EUS imaging, highlighting CNNs' potential to improve diagnostic accuracy and support clinical decisions. Preoperative LN status assessment is crucial for adjusting treatment plans based on metastatic involvement. This AI-powered imaging model with diverse demographic data showed excellent detecting and classification capabilities, highlighting its potential to provide a valuable tool to refine LN assessment with EUS, ultimately supporting more tailored and efficient patient care.
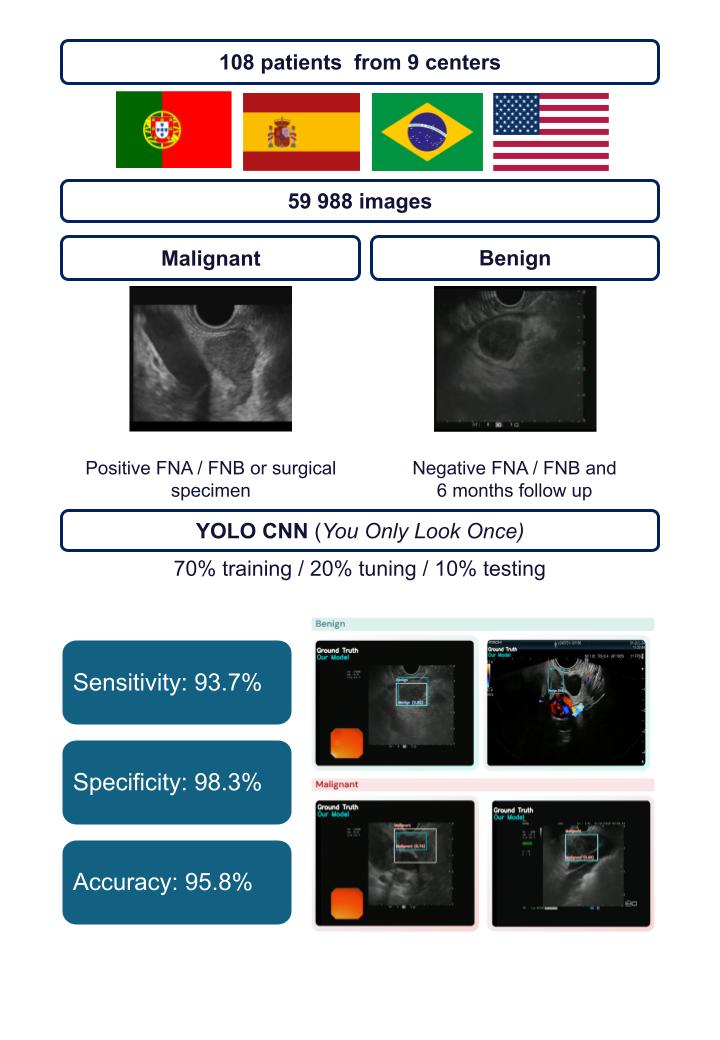
Figure: Study design and main findings
Disclosures:
Miguel Martins indicated no relevant financial relationships.
Miguel Mascarenhas Saraiva indicated no relevant financial relationships.
Belen Agudo indicated no relevant financial relationships.
Francisco Mendes indicated no relevant financial relationships.
António Costa indicated no relevant financial relationships.
Tiago Ribeiro indicated no relevant financial relationships.
Joana Mota indicated no relevant financial relationships.
Maria João Almeida indicated no relevant financial relationships.
Pedro Cardoso indicated no relevant financial relationships.
João Afonso indicated no relevant financial relationships.
Daniel De la Iglesia Garcia indicated no relevant financial relationships.
Carlos Esteban Fernández-Zarza indicated no relevant financial relationships.
Ana Garcia Garcia de Paredes indicated no relevant financial relationships.
Maria Moris indicated no relevant financial relationships.
Matheus Ferreira de Carvalho indicated no relevant financial relationships.
Marcos Eduardo Lera dos Santos indicated no relevant financial relationships.
João Ferreira indicated no relevant financial relationships.
Jessica Widmer indicated no relevant financial relationships.
Filipe Vilas Boas indicated no relevant financial relationships.
Pedro Moutinho Ribeiro indicated no relevant financial relationships.
Susana Lopes indicated no relevant financial relationships.
Mariano Gonzalez Haba indicated no relevant financial relationships.
Eduardo Hourneaux De Moura indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Miguel Martins, MD1, Miguel Mascarenhas Saraiva, MD, PhD1, Belen Agudo, MD2, Francisco Mendes, MD1, António Costa, MD2, Tiago Ribeiro, MD1, Joana Mota, MD1, Maria João Almeida, MD3, Pedro Cardoso, MD1, João Afonso, MD1, Daniel De la Iglesia Garcia, MD, PhD2, Carlos Esteban Fernández-Zarza, MD2, Ana Garcia Garcia de Paredes, MD4, Maria Moris, MD5, Matheus Ferreira de Carvalho, MD6, Marcos Eduardo Lera dos Santos, MD6, João Ferreira, PhD7, Jessica Widmer, DO8, Filipe Vilas Boas, MD, PhD3, Pedro Moutinho Ribeiro, MD, PhD3, Susana Lopes, MD, PhD3, Mariano Gonzalez Haba, MD2, Eduardo Hourneaux De Moura, MD, PhD9, Guilherme Macedo, MD, PhD1. P0090 - Deep Learning for Lymph Node Detection and Malignancy Risk Stratification in EUS: A Multicenter Proof of Concept Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Miguel Martins, MD1, Miguel Mascarenhas Saraiva, MD, PhD1, Belen Agudo, MD2, Francisco Mendes, MD1, António Costa, MD2, Tiago Ribeiro, MD1, Joana Mota, MD1, Maria João Almeida, MD3, Pedro Cardoso, MD1, João Afonso, MD1, Daniel De la Iglesia Garcia, MD, PhD2, Carlos Esteban Fernández-Zarza, MD2, Ana Garcia Garcia de Paredes, MD4, Maria Moris, MD5, Matheus Ferreira de Carvalho, MD6, Marcos Eduardo Lera dos Santos, MD6, João Ferreira, PhD7, Jessica Widmer, DO8, Filipe Vilas Boas, MD, PhD3, Pedro Moutinho Ribeiro, MD, PhD3, Susana Lopes, MD, PhD3, Mariano Gonzalez Haba, MD2, Eduardo Hourneaux De Moura, MD, PhD9, Guilherme Macedo, MD, PhD1
1Centro Hospitalar Universitário São João, Porto, Porto, Portugal; 2Hospital Universitario Puerta de Hierro Majadahonda, Madrid, Madrid, Spain; 3Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 4Hospital Universitario Ramón y Cajal, Madrid, Madrid, Spain; 5Hospital Universitario Marqués de Valdecilla, GI, Santander, Spain,, Santander, Cantabria, Spain; 6Hospital das Clínicas da Faculdade de Medicina da Universidade de Sao Paulo, São Paulo, Sao Paulo, Brazil; 7Faculdade de Engenharia da Universidade do Porto, Porto, Porto, Portugal; 8NYU Langone Health, Mineola, NY; 9Hospital das Clínicas da Faculdade de Medicina da USP, São Paulo, Sao Paulo, Brazil
Introduction: Endoscopic ultrasound (EUS) is important for accurate lymph node (LN) characterization, being essential to guide treatment in suspected malignant involvement. Features like hypoechoic structures, sharply demarcated borders, rounded contours and size over 10 mm suggest malignancy, with 80-100% accuracy when combined, but this complete profile is uncommon. While EUS-guided fineneedle aspiration/biopsy (FNA/FNB) aids diagnosis, its accuracy can be limited. Artificial intelligence (AI) shows potential in improving diagnostic precision in EUS. However, data on convolutional neural network (CNN) application to EUS for LN malignancy prediction remains scarce. This multicenter study aims to evaluate a CNN’s effectiveness in predicting LN malignancy from EUS images.
Methods: This multicenter study included EUS images from nine centers and four countries. Lesions were classified as malignant or benign and delimited with bounding boxes. Definitive diagnoses were based on positive FNA/FNB or surgical specimen and, if negative, a minimum six-month clinical follow-up was required. A CNN was developed including both detection and characterization modules. Performance metrics included detection rate (DR), sensitivity, specificity, accuracy, and AUC were calculated.
Results: 59988 images from 108 patients were used to develop the model. The CNN distinguished malignant from benign LNs with a sensitivity of 93.7%, a specificity of 98.3% and an overall accuracy of 95.8%. The AUC was 0.95.
Discussion: To our knowledge, this study is one of the first to evaluate the performance of deep learning systems for LN assessment using EUS imaging, highlighting CNNs' potential to improve diagnostic accuracy and support clinical decisions. Preoperative LN status assessment is crucial for adjusting treatment plans based on metastatic involvement. This AI-powered imaging model with diverse demographic data showed excellent detecting and classification capabilities, highlighting its potential to provide a valuable tool to refine LN assessment with EUS, ultimately supporting more tailored and efficient patient care.
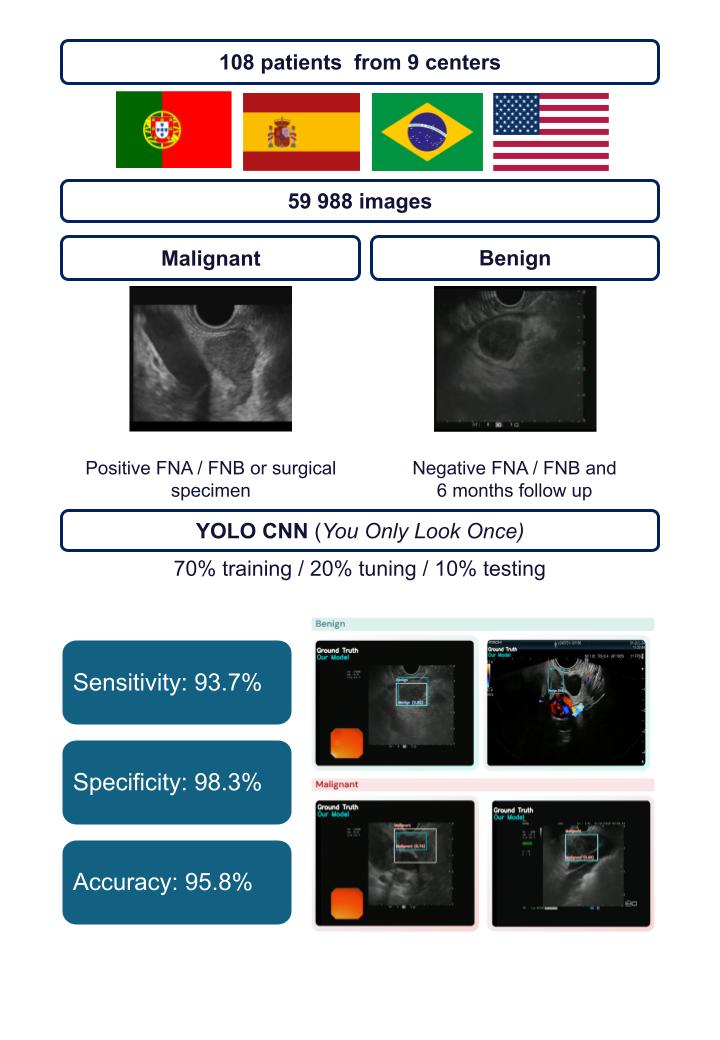
Figure: Study design and main findings
Disclosures:
Miguel Martins indicated no relevant financial relationships.
Miguel Mascarenhas Saraiva indicated no relevant financial relationships.
Belen Agudo indicated no relevant financial relationships.
Francisco Mendes indicated no relevant financial relationships.
António Costa indicated no relevant financial relationships.
Tiago Ribeiro indicated no relevant financial relationships.
Joana Mota indicated no relevant financial relationships.
Maria João Almeida indicated no relevant financial relationships.
Pedro Cardoso indicated no relevant financial relationships.
João Afonso indicated no relevant financial relationships.
Daniel De la Iglesia Garcia indicated no relevant financial relationships.
Carlos Esteban Fernández-Zarza indicated no relevant financial relationships.
Ana Garcia Garcia de Paredes indicated no relevant financial relationships.
Maria Moris indicated no relevant financial relationships.
Matheus Ferreira de Carvalho indicated no relevant financial relationships.
Marcos Eduardo Lera dos Santos indicated no relevant financial relationships.
João Ferreira indicated no relevant financial relationships.
Jessica Widmer indicated no relevant financial relationships.
Filipe Vilas Boas indicated no relevant financial relationships.
Pedro Moutinho Ribeiro indicated no relevant financial relationships.
Susana Lopes indicated no relevant financial relationships.
Mariano Gonzalez Haba indicated no relevant financial relationships.
Eduardo Hourneaux De Moura indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Miguel Martins, MD1, Miguel Mascarenhas Saraiva, MD, PhD1, Belen Agudo, MD2, Francisco Mendes, MD1, António Costa, MD2, Tiago Ribeiro, MD1, Joana Mota, MD1, Maria João Almeida, MD3, Pedro Cardoso, MD1, João Afonso, MD1, Daniel De la Iglesia Garcia, MD, PhD2, Carlos Esteban Fernández-Zarza, MD2, Ana Garcia Garcia de Paredes, MD4, Maria Moris, MD5, Matheus Ferreira de Carvalho, MD6, Marcos Eduardo Lera dos Santos, MD6, João Ferreira, PhD7, Jessica Widmer, DO8, Filipe Vilas Boas, MD, PhD3, Pedro Moutinho Ribeiro, MD, PhD3, Susana Lopes, MD, PhD3, Mariano Gonzalez Haba, MD2, Eduardo Hourneaux De Moura, MD, PhD9, Guilherme Macedo, MD, PhD1. P0090 - Deep Learning for Lymph Node Detection and Malignancy Risk Stratification in EUS: A Multicenter Proof of Concept Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

