Sunday Poster Session
Category: Biliary/Pancreas
P0088 - Rethinking Severity: SIRS Score Outperforms Ranson Criteria in Predicting Pancreatitis Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Dilman Natt, MD
Nassau University Medical Center
East Meadow, New York
Presenting Author(s)
Dilman Natt, MD, Rajmohan Rammohan, MD, Sai Reshma Magam, MD, Achal Patel, MD, Wing Hang Lau, DO, Venkata Panchagnula, MD, Amina Zafar, MD, Amilcar Guaschino, MD, Sri Harsha Boppana, MD, Sindhuja Giridharan, MD, Cesar Orlando Ortiz Bernard, MD, Leeza E. Pannikodu, MD, Paul Mustacchia, MD
Nassau University Medical Center, East Meadow, NY
Introduction: Acute pancreatitis varies in severity and requires early risk assessment. Traditional Ranson criteria are limited by delayed accuracy. This study evaluates the Systemic Inflammatory Response Syndrome (SIRS) score as an early predictor of outcomes, using HCUP data (2019–2024) to assess its link to LOS and readmission.
Methods: In our study, we performed a retrospective analysis of the HCUP National Database from 2019 to 2024 to identify patients with acute pancreatitis using specific ICD codes. We collected data on comorbidities, insurance status, educational levels, and hospital admissions. SIRS criteria were assessed on days 1, 2, and 3 of hospital admission. We applied binary logistic regression to identify independent risk factors for readmission. Further, we used area under the receiver operating characteristic curve (AUROC) and relationship mapping techniques to evaluate the risk and predictive accuracy of various variables in the logistic regression model.
Results: Data from the Healthcare Cost and Utilization Project (HCUP) National Database were used to analyze hospital admissions from 2019 to 2024, encompassing a total of 2,858,576 adults. Among these, 58,546 patients were diagnosed with pancreatitis, with 21,015 (approximately 44%) being female. The analysis revealed that patients with higher Systemic Inflammatory Response Syndrome (SIRS) scores on day 1 experienced increased Length of Stay (LOS) (p=0.012). Similarly, higher SIRS scores on day 2 were associated with increased LOS (p=0.0234), while lower SIRS scores corresponded to reduced LOS (p=0.031). These findings suggest that SIRS criteria could serve as an alternative to the Ranson score for predicting LOS in patients with acute pancreatitis.
Discussion: The findings from our study using the HCUP National Database indicate that the Systemic Inflammatory Response Syndrome (SIRS) score effectively predicts hospital outcomes, such as length of stay, in acute pancreatitis patients. Our data shows that higher SIRS scores correlate with increased length of stay, supporting the score’s utility as an early, dynamic assessment tool in clinical settings. The results emphasize the need for further research into integrating SIRS scores into standard practice, potentially enhancing management strategies and improving outcomes by enabling more targeted and timely interventions for acute pancreatitis.
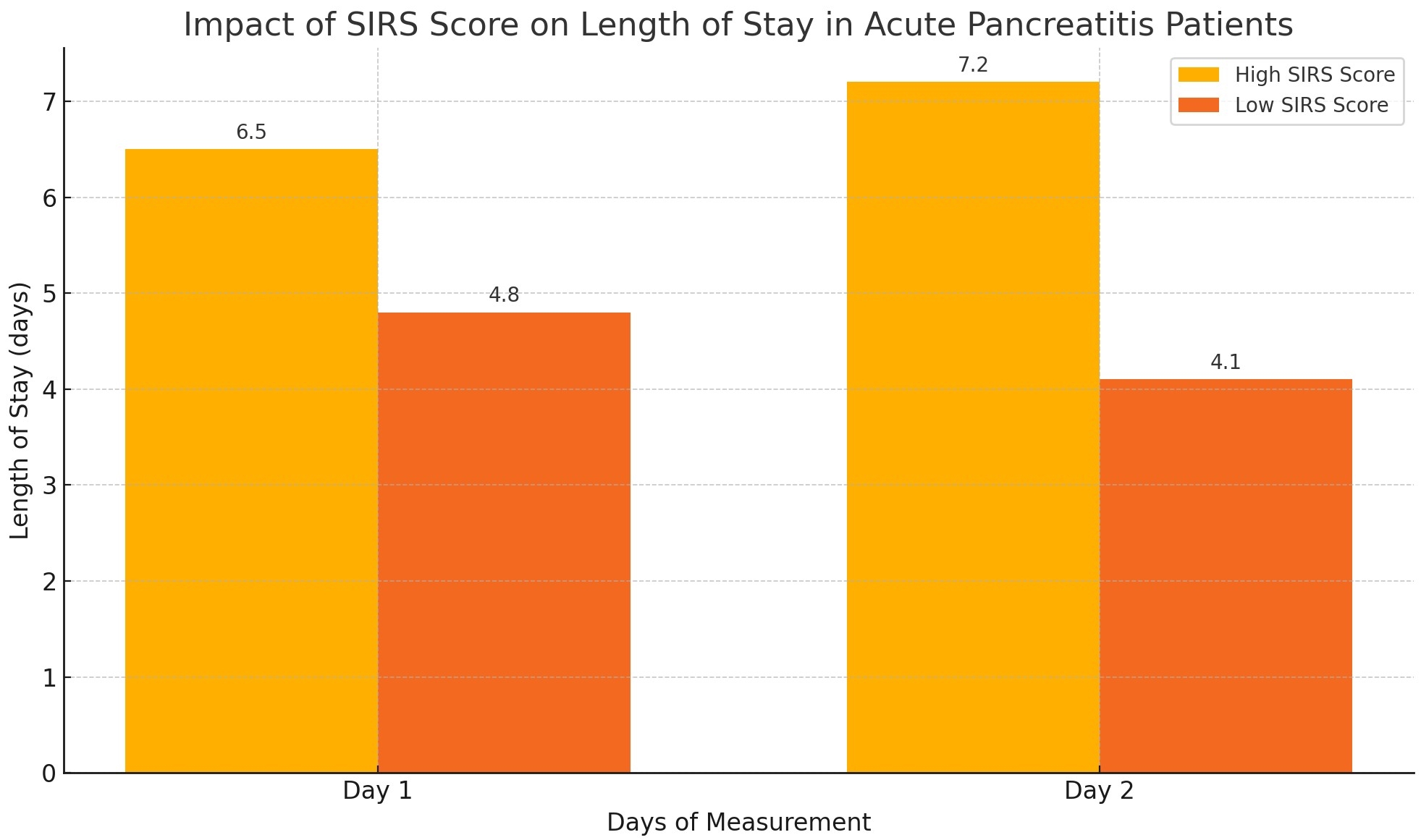
Figure: Relation between SIRS and Acute Pancreatitis
Disclosures:
Dilman Natt indicated no relevant financial relationships.
Rajmohan Rammohan indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Achal Patel indicated no relevant financial relationships.
Wing Hang Lau indicated no relevant financial relationships.
Venkata Panchagnula indicated no relevant financial relationships.
Amina Zafar indicated no relevant financial relationships.
Amilcar Guaschino indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Sindhuja Giridharan indicated no relevant financial relationships.
Cesar Orlando Ortiz Bernard indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Dilman Natt, MD, Rajmohan Rammohan, MD, Sai Reshma Magam, MD, Achal Patel, MD, Wing Hang Lau, DO, Venkata Panchagnula, MD, Amina Zafar, MD, Amilcar Guaschino, MD, Sri Harsha Boppana, MD, Sindhuja Giridharan, MD, Cesar Orlando Ortiz Bernard, MD, Leeza E. Pannikodu, MD, Paul Mustacchia, MD. P0088 - Rethinking Severity: SIRS Score Outperforms Ranson Criteria in Predicting Pancreatitis Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Acute pancreatitis varies in severity and requires early risk assessment. Traditional Ranson criteria are limited by delayed accuracy. This study evaluates the Systemic Inflammatory Response Syndrome (SIRS) score as an early predictor of outcomes, using HCUP data (2019–2024) to assess its link to LOS and readmission.
Methods: In our study, we performed a retrospective analysis of the HCUP National Database from 2019 to 2024 to identify patients with acute pancreatitis using specific ICD codes. We collected data on comorbidities, insurance status, educational levels, and hospital admissions. SIRS criteria were assessed on days 1, 2, and 3 of hospital admission. We applied binary logistic regression to identify independent risk factors for readmission. Further, we used area under the receiver operating characteristic curve (AUROC) and relationship mapping techniques to evaluate the risk and predictive accuracy of various variables in the logistic regression model.
Results: Data from the Healthcare Cost and Utilization Project (HCUP) National Database were used to analyze hospital admissions from 2019 to 2024, encompassing a total of 2,858,576 adults. Among these, 58,546 patients were diagnosed with pancreatitis, with 21,015 (approximately 44%) being female. The analysis revealed that patients with higher Systemic Inflammatory Response Syndrome (SIRS) scores on day 1 experienced increased Length of Stay (LOS) (p=0.012). Similarly, higher SIRS scores on day 2 were associated with increased LOS (p=0.0234), while lower SIRS scores corresponded to reduced LOS (p=0.031). These findings suggest that SIRS criteria could serve as an alternative to the Ranson score for predicting LOS in patients with acute pancreatitis.
Discussion: The findings from our study using the HCUP National Database indicate that the Systemic Inflammatory Response Syndrome (SIRS) score effectively predicts hospital outcomes, such as length of stay, in acute pancreatitis patients. Our data shows that higher SIRS scores correlate with increased length of stay, supporting the score’s utility as an early, dynamic assessment tool in clinical settings. The results emphasize the need for further research into integrating SIRS scores into standard practice, potentially enhancing management strategies and improving outcomes by enabling more targeted and timely interventions for acute pancreatitis.
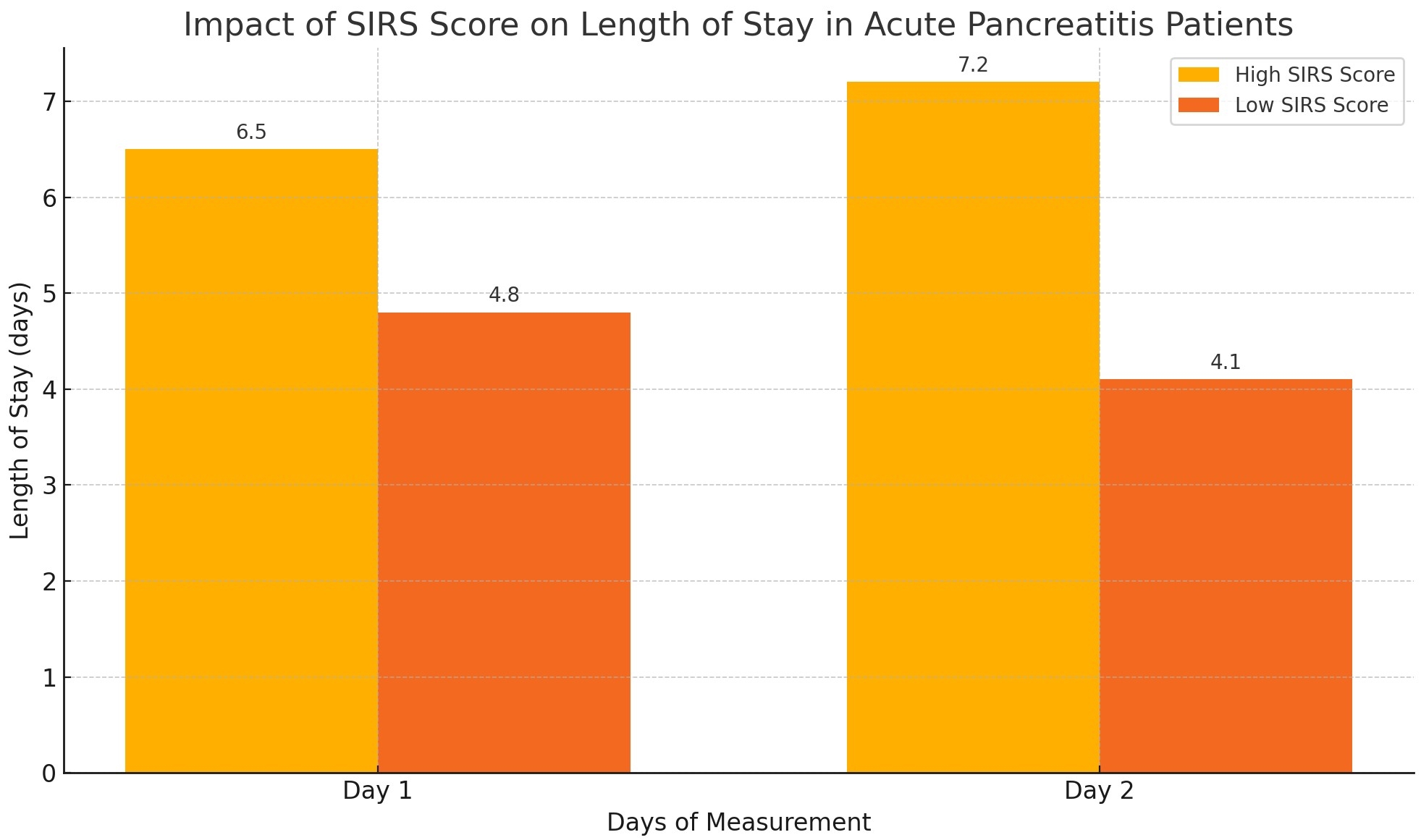
Figure: Relation between SIRS and Acute Pancreatitis
Disclosures:
Dilman Natt indicated no relevant financial relationships.
Rajmohan Rammohan indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Achal Patel indicated no relevant financial relationships.
Wing Hang Lau indicated no relevant financial relationships.
Venkata Panchagnula indicated no relevant financial relationships.
Amina Zafar indicated no relevant financial relationships.
Amilcar Guaschino indicated no relevant financial relationships.
Sri Harsha Boppana indicated no relevant financial relationships.
Sindhuja Giridharan indicated no relevant financial relationships.
Cesar Orlando Ortiz Bernard indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Dilman Natt, MD, Rajmohan Rammohan, MD, Sai Reshma Magam, MD, Achal Patel, MD, Wing Hang Lau, DO, Venkata Panchagnula, MD, Amina Zafar, MD, Amilcar Guaschino, MD, Sri Harsha Boppana, MD, Sindhuja Giridharan, MD, Cesar Orlando Ortiz Bernard, MD, Leeza E. Pannikodu, MD, Paul Mustacchia, MD. P0088 - Rethinking Severity: SIRS Score Outperforms Ranson Criteria in Predicting Pancreatitis Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
