Sunday Poster Session
Category: Biliary/Pancreas
P0087 - Outcomes of Pancreatic Cancer in Patients With Prior Bariatric Surgery: A National Inpatient Sample Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Yasmin O. Ali, MBBS
hennepin Healthcare
Minneapolis, MN
Presenting Author(s)
Zachary Leslie, 1, Yasmin O. Ali, MBBS2, Khalid Ahmed, MD3, Eric Wise, MD, MA4, Ahmed Dirweesh, MD5, Stuart K. Amateau, MD, PhD5
1UMN, Minneapolis, MN; 2hennepin Healthcare, Minneapolis, MN; 3University of Minnesota, Minneapolis, MN; 4University of Minnesota Medical School, Minneapolis, MN; 5University of Minnesota Medical Center, Minneapolis, MN
Introduction: High incidence rates of pancreatic cancer have been observed in individuals with
class 3 obesity. While prior studies suggest that bariatric surgery may reduce the risk of
pancreatic cancer, limited data exist regarding the outcomes of patients who develop
pancreatic cancer within this population.
Methods: We performed a retrospective study using data from the National Inpatient Sample
(NIS) from 2016 to 2022. Patients with class 3 obesity and pancreatic cancer were
identified using ICD-10 codes and stratified based on their history of bariatric surgery.
Demographics, clinical characteristics, and outcomes, including Whipple procedures,
the presence of metastasis, and inpatient mortality, were compared using univariable
and multivariable logistic regression models.
Results: Of 10,083 patients with class 3 obesity diagnosed with pancreatic cancer, 27.1% had
undergone bariatric surgery. Compared to those without prior bariatric surgery, these
patients were more likely to be female (66.1% vs. 56.9%), of White ethnicity (74.2% vs.
69.2%) and have Medicare insurance coverage (52.8% vs. 55.8%), all p-values < 0.001.
Additionally, they were more frequently admitted to high-volume centers and had a
lower Charlson Comorbidity Index (5.89 vs. 6.86). However, multivariable analysis
showed significantly higher odds of metastatic cancer in patients with a history of
bariatric surgery (aOR 1.5, 95% CI:1.27-1.77; p < 0.005). Despite this, bariatric surgery
did not significantly impact the likelihood of undergoing a Whipple procedure (aOR 1.23,
95% CI: 0.98–1.55; p = 0.07) or inpatient mortality (aOR 1.21, 95% CI: 0.92–1.61; p =
0.18). (Table.1)
Discussion: Although bariatric surgery may reduce the overall risk of developing pancreatic cancer,
our findings suggest that patients who do develop pancreatic cancer are more likely to
have metastatic disease. This could be due to altered anatomy potentially leading to
delayed diagnosis. Early referral to tertiary hospitals should be considered when
pancreatic cancer is suspected in this population to facilitate timely diagnostic
evaluation.
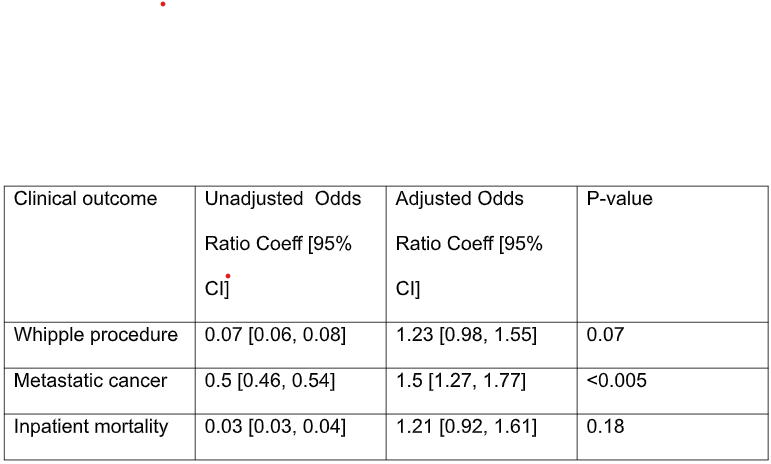
Figure: Table.1 Multivariable binomial logistic regression coefficients assessing the association
between clinical outcomes and prior history of bariatric surgery in patients with
pancreatic cancer. The analysis was adjusted for age, sex, race, medium income,
Charlson Comorbidity Index, and primary payer.
Disclosures:
Zachary Leslie indicated no relevant financial relationships.
Yasmin Ali indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Eric Wise indicated no relevant financial relationships.
Ahmed Dirweesh indicated no relevant financial relationships.
Stuart Amateau: BSC – Consultant. Cook – Consultant. Endo-Therapeutics – Consultant. Merit – Consultant. Olympus – Advisor or Review Panel Member, Consultant. Provation – Advisory Committee/Board Member. Steris – Consultant.
Zachary Leslie, 1, Yasmin O. Ali, MBBS2, Khalid Ahmed, MD3, Eric Wise, MD, MA4, Ahmed Dirweesh, MD5, Stuart K. Amateau, MD, PhD5. P0087 - Outcomes of Pancreatic Cancer in Patients With Prior Bariatric Surgery: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UMN, Minneapolis, MN; 2hennepin Healthcare, Minneapolis, MN; 3University of Minnesota, Minneapolis, MN; 4University of Minnesota Medical School, Minneapolis, MN; 5University of Minnesota Medical Center, Minneapolis, MN
Introduction: High incidence rates of pancreatic cancer have been observed in individuals with
class 3 obesity. While prior studies suggest that bariatric surgery may reduce the risk of
pancreatic cancer, limited data exist regarding the outcomes of patients who develop
pancreatic cancer within this population.
Methods: We performed a retrospective study using data from the National Inpatient Sample
(NIS) from 2016 to 2022. Patients with class 3 obesity and pancreatic cancer were
identified using ICD-10 codes and stratified based on their history of bariatric surgery.
Demographics, clinical characteristics, and outcomes, including Whipple procedures,
the presence of metastasis, and inpatient mortality, were compared using univariable
and multivariable logistic regression models.
Results: Of 10,083 patients with class 3 obesity diagnosed with pancreatic cancer, 27.1% had
undergone bariatric surgery. Compared to those without prior bariatric surgery, these
patients were more likely to be female (66.1% vs. 56.9%), of White ethnicity (74.2% vs.
69.2%) and have Medicare insurance coverage (52.8% vs. 55.8%), all p-values < 0.001.
Additionally, they were more frequently admitted to high-volume centers and had a
lower Charlson Comorbidity Index (5.89 vs. 6.86). However, multivariable analysis
showed significantly higher odds of metastatic cancer in patients with a history of
bariatric surgery (aOR 1.5, 95% CI:1.27-1.77; p < 0.005). Despite this, bariatric surgery
did not significantly impact the likelihood of undergoing a Whipple procedure (aOR 1.23,
95% CI: 0.98–1.55; p = 0.07) or inpatient mortality (aOR 1.21, 95% CI: 0.92–1.61; p =
0.18). (Table.1)
Discussion: Although bariatric surgery may reduce the overall risk of developing pancreatic cancer,
our findings suggest that patients who do develop pancreatic cancer are more likely to
have metastatic disease. This could be due to altered anatomy potentially leading to
delayed diagnosis. Early referral to tertiary hospitals should be considered when
pancreatic cancer is suspected in this population to facilitate timely diagnostic
evaluation.
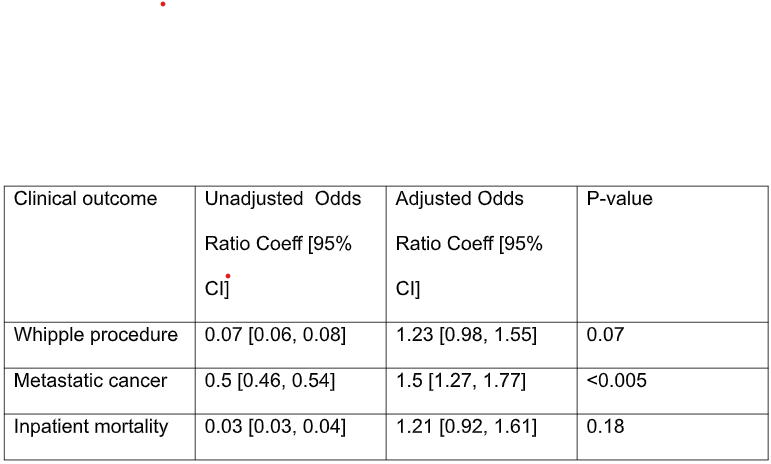
Figure: Table.1 Multivariable binomial logistic regression coefficients assessing the association
between clinical outcomes and prior history of bariatric surgery in patients with
pancreatic cancer. The analysis was adjusted for age, sex, race, medium income,
Charlson Comorbidity Index, and primary payer.
Disclosures:
Zachary Leslie indicated no relevant financial relationships.
Yasmin Ali indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Eric Wise indicated no relevant financial relationships.
Ahmed Dirweesh indicated no relevant financial relationships.
Stuart Amateau: BSC – Consultant. Cook – Consultant. Endo-Therapeutics – Consultant. Merit – Consultant. Olympus – Advisor or Review Panel Member, Consultant. Provation – Advisory Committee/Board Member. Steris – Consultant.
Zachary Leslie, 1, Yasmin O. Ali, MBBS2, Khalid Ahmed, MD3, Eric Wise, MD, MA4, Ahmed Dirweesh, MD5, Stuart K. Amateau, MD, PhD5. P0087 - Outcomes of Pancreatic Cancer in Patients With Prior Bariatric Surgery: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
