Sunday Poster Session
Category: Biliary/Pancreas
P0082 - Does Autoimmune Pancreatitis Pose a Greater Risk of Deep Vein Thrombosis Compared to Acute Pancreatitis? A Ten-Year, Single Center Experience
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohammed Abourahma, MD
Loyola University Medical Center
Willowbrook, IL
Presenting Author(s)
Mohammed Abourahma, MD1, Alexander O'Hara, MD2, Dinkar Ahuja, MD3, Janna Kotsen, BS4, Muneeb Ansari, MD2, Sebastian Chirayil, MD2, Ayokunle T. Abegunde, MD, MBBS, MSc, MRCGP2
1Loyola University Medical Center, Willowbrook, IL; 2Loyola University Medical Center, Maywood, IL; 3Loyola University Medical Center, Chicago, IL; 4Loyola University Chicago Stritch School of Medicine, Maywood, IL
Introduction: Autoimmune pancreatitis (AIP) is a rare pathology that is often mistaken for pancreatic cancer. Three aspects of this pathology can promote thrombus formation: chronic pancreatitis (CP), acute pancreatitis (AP), and systemic autoimmune disease. Despite this, no studies exist describing deep vein thrombosis (DVT) and pulmonary embolism (PE) prevalence in AIP. We hypothesize that DVT and PE rates are higher in this population, given the combined prothrombotic risk from these three mechanisms.
Methods: We conducted a ten-year single-center retrospective study. Patients were confirmed to have AIP using ICDC criteria. AP was confirmed with 2/3 revised Atlanta criteria. All patients had radiographically confirmed DVT or PE within three months of initial AP or AIP diagnosis. Patients with malignancy, surgery unrelated to pancreatitis, pro-coagulant disorders, pregnancy, or estrogen therapy were excluded. Propensity score matching (1:3 nearest-neighbor) was used to control for age, sex, race, and smoking status. Statistical analysis included Fisher’s exact and t-tests.
Results: Fourteen patients with AIP were matched to 42 patients with AP using propensity score matching. No significant differences were observed in baseline demographic characteristics, including age, sex, race, and smoking status. No statistically significant differences were noted in the prevalence of common medical comorbidities between the two groups. Throughout the ten-year study period, no AIP patients were documented to have developed either DVT or PE. In the AP group, three patients (7.1%) developed DVT and one (2.4%) developed PE. These differences were not statistically significant (DVT: p = 0.565; PE: p = 1.000).
Discussion: There was no statistically significant difference in the prevalence of DVT or PE between patients with AIP and those with AP. This finding suggests that AIP is not associated with an increased risk of thrombosis, despite the three known prothrombotic risk factors: systemic autoimmune inflammation, AP, and CP. Further, across the ten-year study period, no AIP patient developed DVT or PE. This study was limited by a small sample size. To our knowledge, it is the first to specifically evaluate thromboembolic events in AIP and may provide valuable initial insight into its thrombotic risk profile.
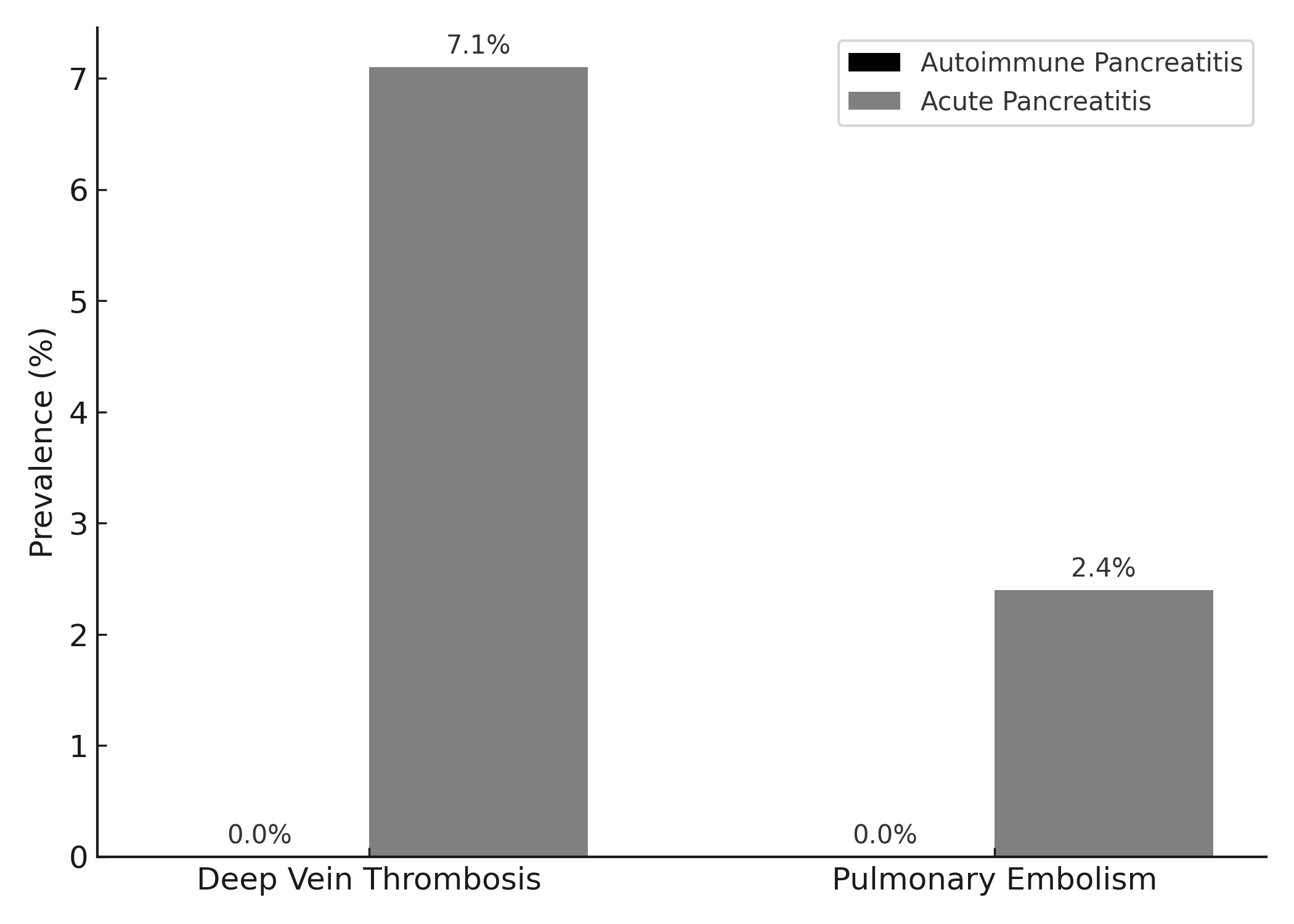
Figure: Comparison of Demographic and Clinical Comorbidities (all P values > 0.05)
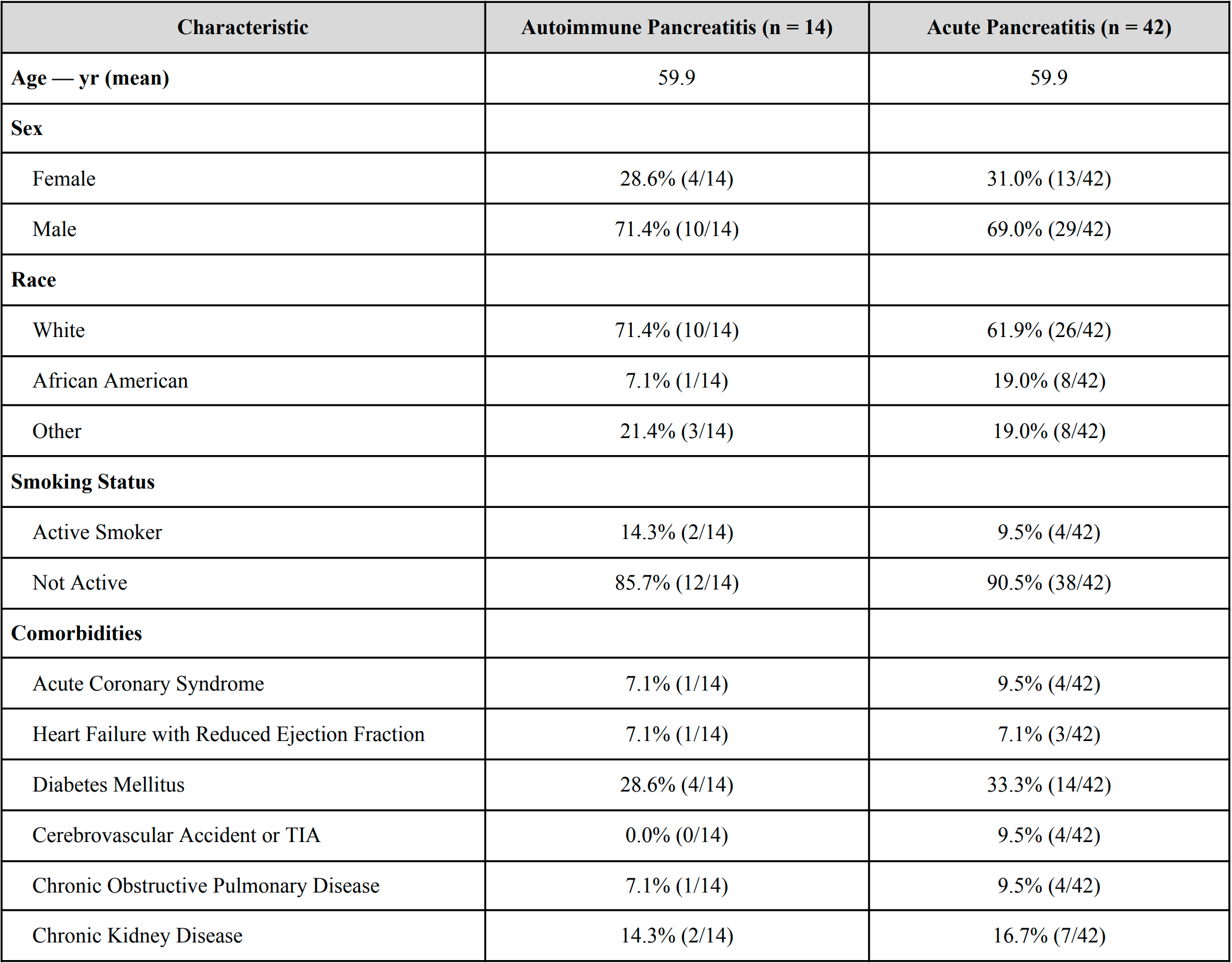
Figure: Prevalence of thrombotic events in autoimmune pancreatitis versus acute pancreatitis
Disclosures:
Mohammed Abourahma indicated no relevant financial relationships.
Alexander O'Hara indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Janna Kotsen indicated no relevant financial relationships.
Muneeb Ansari indicated no relevant financial relationships.
Sebastian Chirayil indicated no relevant financial relationships.
Ayokunle Abegunde indicated no relevant financial relationships.
Mohammed Abourahma, MD1, Alexander O'Hara, MD2, Dinkar Ahuja, MD3, Janna Kotsen, BS4, Muneeb Ansari, MD2, Sebastian Chirayil, MD2, Ayokunle T. Abegunde, MD, MBBS, MSc, MRCGP2. P0082 - Does Autoimmune Pancreatitis Pose a Greater Risk of Deep Vein Thrombosis Compared to Acute Pancreatitis? A Ten-Year, Single Center Experience, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Willowbrook, IL; 2Loyola University Medical Center, Maywood, IL; 3Loyola University Medical Center, Chicago, IL; 4Loyola University Chicago Stritch School of Medicine, Maywood, IL
Introduction: Autoimmune pancreatitis (AIP) is a rare pathology that is often mistaken for pancreatic cancer. Three aspects of this pathology can promote thrombus formation: chronic pancreatitis (CP), acute pancreatitis (AP), and systemic autoimmune disease. Despite this, no studies exist describing deep vein thrombosis (DVT) and pulmonary embolism (PE) prevalence in AIP. We hypothesize that DVT and PE rates are higher in this population, given the combined prothrombotic risk from these three mechanisms.
Methods: We conducted a ten-year single-center retrospective study. Patients were confirmed to have AIP using ICDC criteria. AP was confirmed with 2/3 revised Atlanta criteria. All patients had radiographically confirmed DVT or PE within three months of initial AP or AIP diagnosis. Patients with malignancy, surgery unrelated to pancreatitis, pro-coagulant disorders, pregnancy, or estrogen therapy were excluded. Propensity score matching (1:3 nearest-neighbor) was used to control for age, sex, race, and smoking status. Statistical analysis included Fisher’s exact and t-tests.
Results: Fourteen patients with AIP were matched to 42 patients with AP using propensity score matching. No significant differences were observed in baseline demographic characteristics, including age, sex, race, and smoking status. No statistically significant differences were noted in the prevalence of common medical comorbidities between the two groups. Throughout the ten-year study period, no AIP patients were documented to have developed either DVT or PE. In the AP group, three patients (7.1%) developed DVT and one (2.4%) developed PE. These differences were not statistically significant (DVT: p = 0.565; PE: p = 1.000).
Discussion: There was no statistically significant difference in the prevalence of DVT or PE between patients with AIP and those with AP. This finding suggests that AIP is not associated with an increased risk of thrombosis, despite the three known prothrombotic risk factors: systemic autoimmune inflammation, AP, and CP. Further, across the ten-year study period, no AIP patient developed DVT or PE. This study was limited by a small sample size. To our knowledge, it is the first to specifically evaluate thromboembolic events in AIP and may provide valuable initial insight into its thrombotic risk profile.
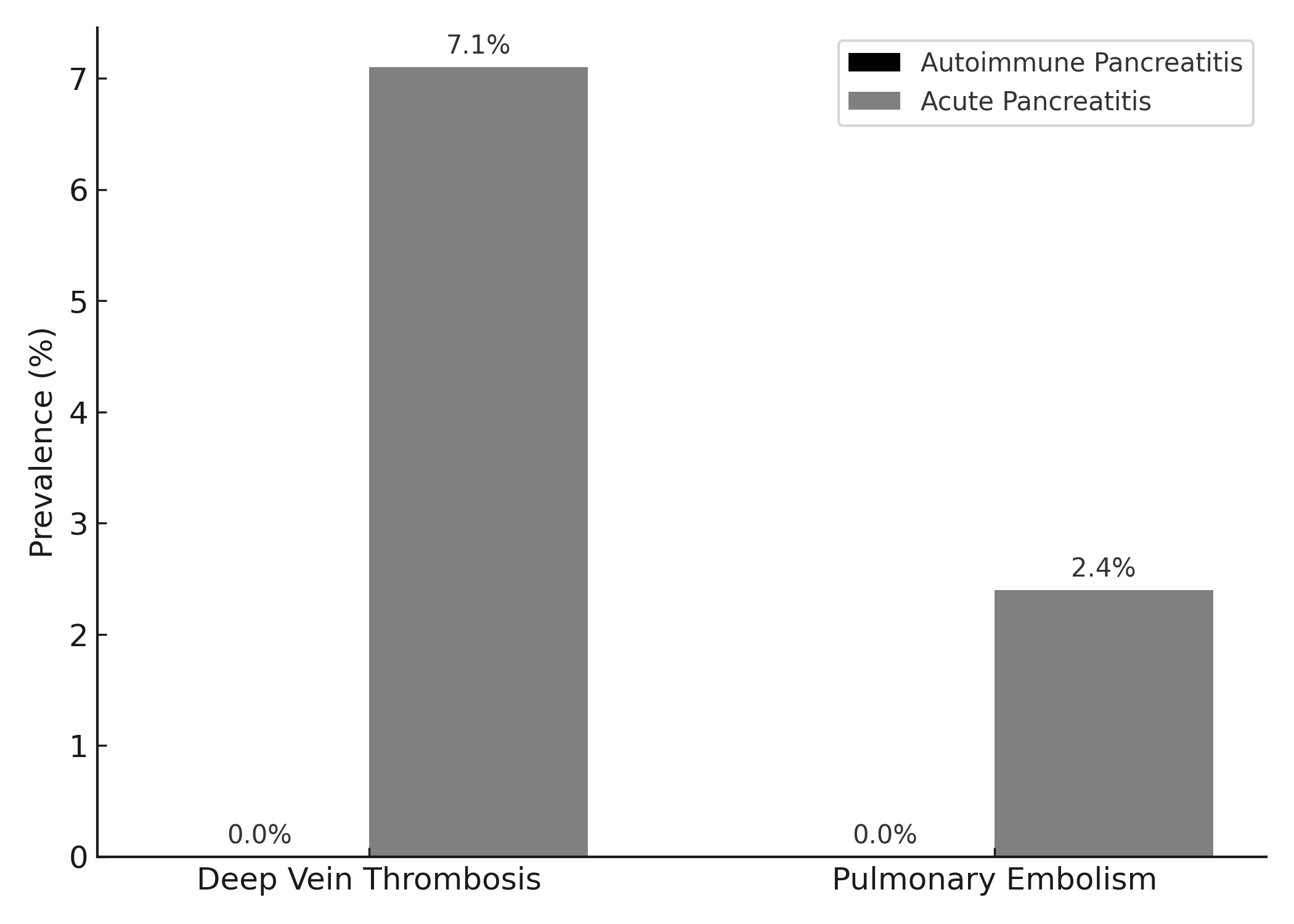
Figure: Comparison of Demographic and Clinical Comorbidities (all P values > 0.05)
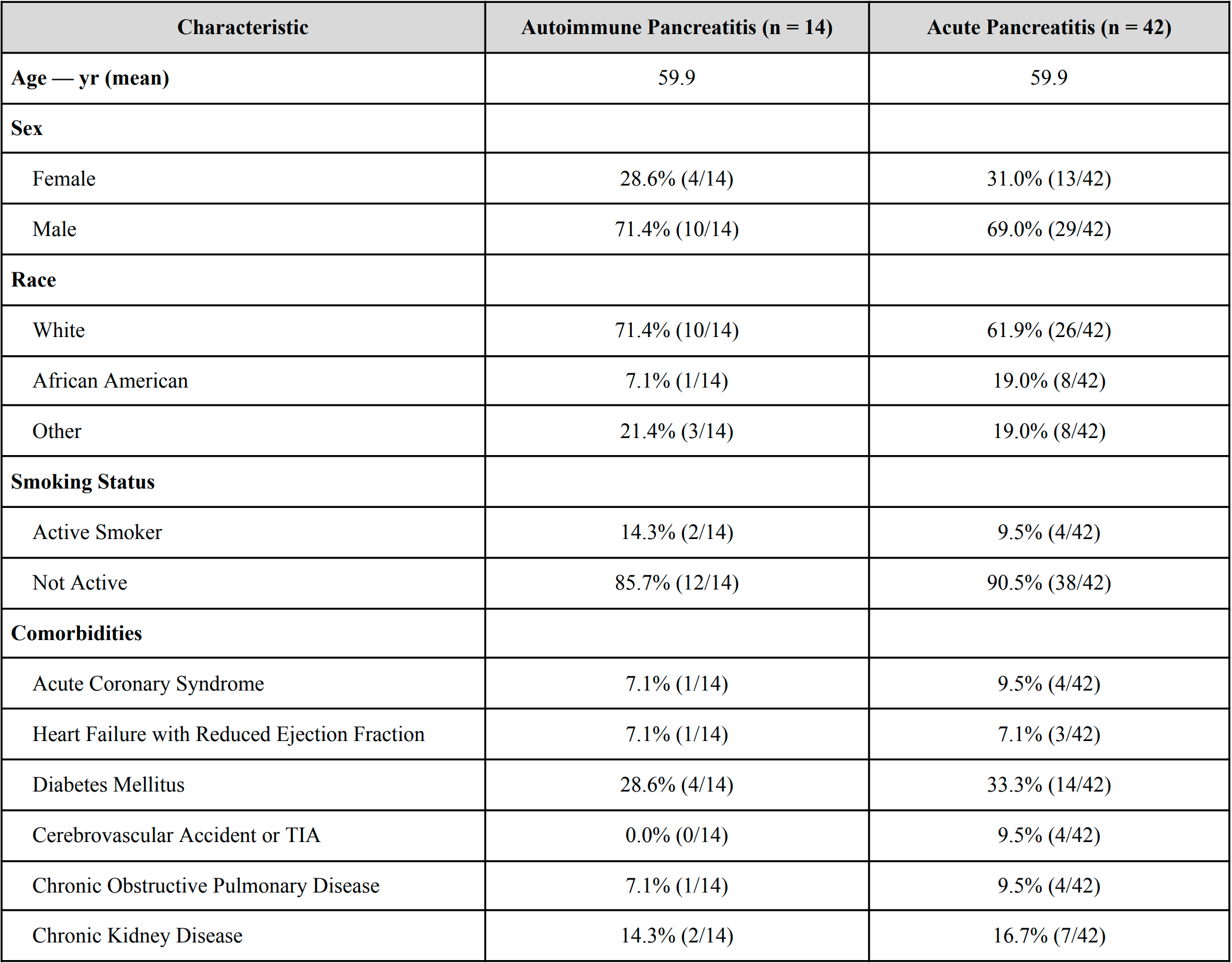
Figure: Prevalence of thrombotic events in autoimmune pancreatitis versus acute pancreatitis
Disclosures:
Mohammed Abourahma indicated no relevant financial relationships.
Alexander O'Hara indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Janna Kotsen indicated no relevant financial relationships.
Muneeb Ansari indicated no relevant financial relationships.
Sebastian Chirayil indicated no relevant financial relationships.
Ayokunle Abegunde indicated no relevant financial relationships.
Mohammed Abourahma, MD1, Alexander O'Hara, MD2, Dinkar Ahuja, MD3, Janna Kotsen, BS4, Muneeb Ansari, MD2, Sebastian Chirayil, MD2, Ayokunle T. Abegunde, MD, MBBS, MSc, MRCGP2. P0082 - Does Autoimmune Pancreatitis Pose a Greater Risk of Deep Vein Thrombosis Compared to Acute Pancreatitis? A Ten-Year, Single Center Experience, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
