Sunday Poster Session
Category: Biliary/Pancreas
P0081 - Systemic Therapy for a Local Problem? Anticoagulation in Pancreatitis-Induced Splanchnic Vein Thrombosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohammed Abourahma, MD
Loyola University Medical Center
Willowbrook, IL
Presenting Author(s)
Mohammed Abourahma, MD1, Alexander O'Hara, MD2, Muneeb Ansari, MD2, Sebastian Chirayil, MD2, Dinkar Ahuja, MD3, Martin Kalski, BS4, Ayokunle T. Abegunde, MD, MBBS, MSc, MRCGP2, Dejan Micic, MD2
1Loyola University Medical Center, Willowbrook, IL; 2Loyola University Medical Center, Maywood, IL; 3Loyola University Medical Center, Chicago, IL; 4Loyola University Chicago Stritch School of Medicine, Chicago, IL
Introduction: Splanchnic vein thrombosis (SVT) is a complication of acute pancreatitis (AP). The role of anticoagulation (AC) in this setting remains controversial, with no formal guidelines. Data from current studies conflict on whether AC improves thrombus resolution or affects bleeding risk. This study explores where AC may offer the greatest clinical benefit.
Methods: In this retrospective cohort study, we included patients between 01/2014 to 12/2024 who presented with AP and radiographically confirmed splanchnic vein thrombosis (SVT) within three months. Exclusion criteria were malignancy, cirrhosis, age < 18, and hypercoagulable disorders. The primary outcome was complete thrombus resolution on imaging within 6 months. Patients were further stratified by thrombus chronicity, with chronic thrombus (CT) defined by the presence of venous collaterals, and acute thrombus (AT) defined by their absence. Categorical variables were reported as frequencies and proportions. Proportions were compared using chi-square or Fisher’s exact test with a significance level of a = 0.05.
Results: Of 40 patients, 26 (65%) received AC and 14 (35%) did not. Median AC duration was 3.5 months (IQR: 3.0–6.0). Thrombus resolution was higher in the AC group (39.1% [9/23]) vs. no AC (23.1% [3/13], p=0.4678). Baseline comorbidities and labs were similar, though the AC group had a higher proportion of women (61.5% vs. 14.3%, p=0.007).
Among isolated thrombi, resolution with AC vs. no AC was: mesenteric (4/5 [80%] vs. 0/1 [0%], p=0.33), and splenic (1/5 [20%] vs. 0/4 [0%], p=1.00). Secondary outcomes (AC vs. no AC) included bleeding (19.2% vs. 14.3%, p=1.00), 30-day readmission (50.0% vs. 42.9%, p=0.92), and mortality (7.7% vs. 0%, p=0.53). Thrombus resolution was higher with AC in patients with AT compared to AC in CT (60.0% [6/10] vs. 23.1% [3/13], p=0.102). Clinically significant bleeding was also more frequent in CT patients who received AC compared to those with CT and no AC (38.5% vs. 12.5%, p=0.338).
Discussion: Overall, thrombus resolution was higher with AC, with similar bleeding rates (p > 0.05). The benefit of AC was more pronounced in patients with AT, while bleeding risk with AC was higher in those with CT compared to the general cohort (38.5% vs. 19.2%, p=0.25). AC was associated with higher resolution rates in isolated thrombi but showed less benefit in patients with local complications of AP and multiple thrombi. Although underpowered, this study suggests that AC may offer the greatest benefit in select subgroups.
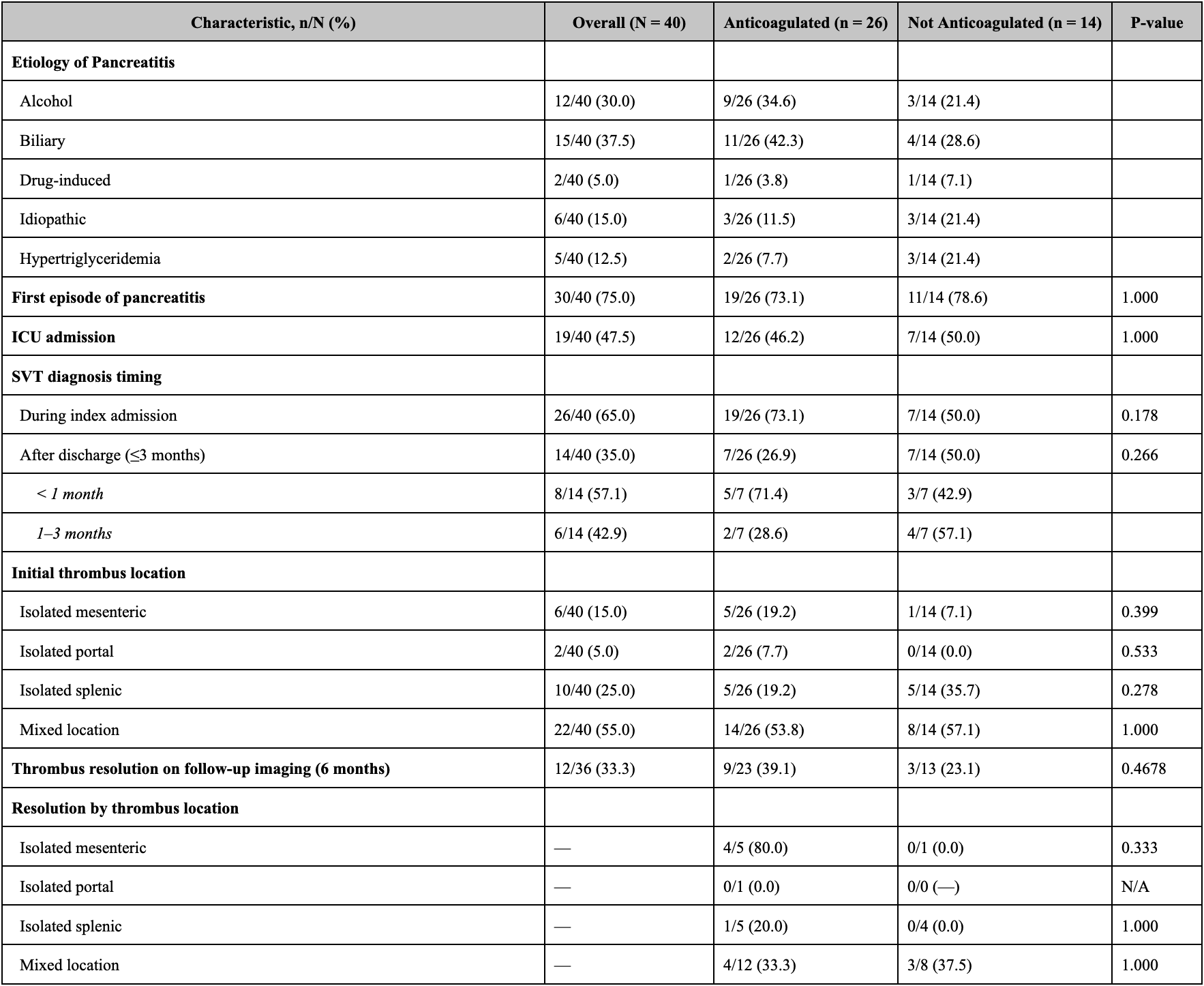
Figure: Thrombus resolution and bleeding risk stratified by thrombus chronicity and local pancreatic complications. Relative risks (RR) were calculated with a 0.05 continuity correction for zero counts.
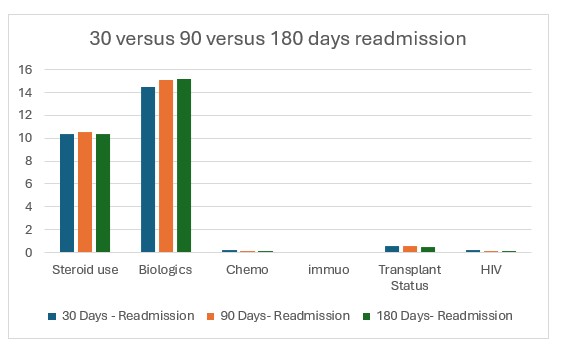
Figure: Clinical Characteristics, Thrombus Resolution and Location Distribution
Disclosures:
Mohammed Abourahma indicated no relevant financial relationships.
Alexander O'Hara indicated no relevant financial relationships.
Muneeb Ansari indicated no relevant financial relationships.
Sebastian Chirayil indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Martin Kalski indicated no relevant financial relationships.
Ayokunle Abegunde indicated no relevant financial relationships.
Dejan Micic indicated no relevant financial relationships.
Mohammed Abourahma, MD1, Alexander O'Hara, MD2, Muneeb Ansari, MD2, Sebastian Chirayil, MD2, Dinkar Ahuja, MD3, Martin Kalski, BS4, Ayokunle T. Abegunde, MD, MBBS, MSc, MRCGP2, Dejan Micic, MD2. P0081 - Systemic Therapy for a Local Problem? Anticoagulation in Pancreatitis-Induced Splanchnic Vein Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Willowbrook, IL; 2Loyola University Medical Center, Maywood, IL; 3Loyola University Medical Center, Chicago, IL; 4Loyola University Chicago Stritch School of Medicine, Chicago, IL
Introduction: Splanchnic vein thrombosis (SVT) is a complication of acute pancreatitis (AP). The role of anticoagulation (AC) in this setting remains controversial, with no formal guidelines. Data from current studies conflict on whether AC improves thrombus resolution or affects bleeding risk. This study explores where AC may offer the greatest clinical benefit.
Methods: In this retrospective cohort study, we included patients between 01/2014 to 12/2024 who presented with AP and radiographically confirmed splanchnic vein thrombosis (SVT) within three months. Exclusion criteria were malignancy, cirrhosis, age < 18, and hypercoagulable disorders. The primary outcome was complete thrombus resolution on imaging within 6 months. Patients were further stratified by thrombus chronicity, with chronic thrombus (CT) defined by the presence of venous collaterals, and acute thrombus (AT) defined by their absence. Categorical variables were reported as frequencies and proportions. Proportions were compared using chi-square or Fisher’s exact test with a significance level of a = 0.05.
Results: Of 40 patients, 26 (65%) received AC and 14 (35%) did not. Median AC duration was 3.5 months (IQR: 3.0–6.0). Thrombus resolution was higher in the AC group (39.1% [9/23]) vs. no AC (23.1% [3/13], p=0.4678). Baseline comorbidities and labs were similar, though the AC group had a higher proportion of women (61.5% vs. 14.3%, p=0.007).
Among isolated thrombi, resolution with AC vs. no AC was: mesenteric (4/5 [80%] vs. 0/1 [0%], p=0.33), and splenic (1/5 [20%] vs. 0/4 [0%], p=1.00). Secondary outcomes (AC vs. no AC) included bleeding (19.2% vs. 14.3%, p=1.00), 30-day readmission (50.0% vs. 42.9%, p=0.92), and mortality (7.7% vs. 0%, p=0.53). Thrombus resolution was higher with AC in patients with AT compared to AC in CT (60.0% [6/10] vs. 23.1% [3/13], p=0.102). Clinically significant bleeding was also more frequent in CT patients who received AC compared to those with CT and no AC (38.5% vs. 12.5%, p=0.338).
Discussion: Overall, thrombus resolution was higher with AC, with similar bleeding rates (p > 0.05). The benefit of AC was more pronounced in patients with AT, while bleeding risk with AC was higher in those with CT compared to the general cohort (38.5% vs. 19.2%, p=0.25). AC was associated with higher resolution rates in isolated thrombi but showed less benefit in patients with local complications of AP and multiple thrombi. Although underpowered, this study suggests that AC may offer the greatest benefit in select subgroups.
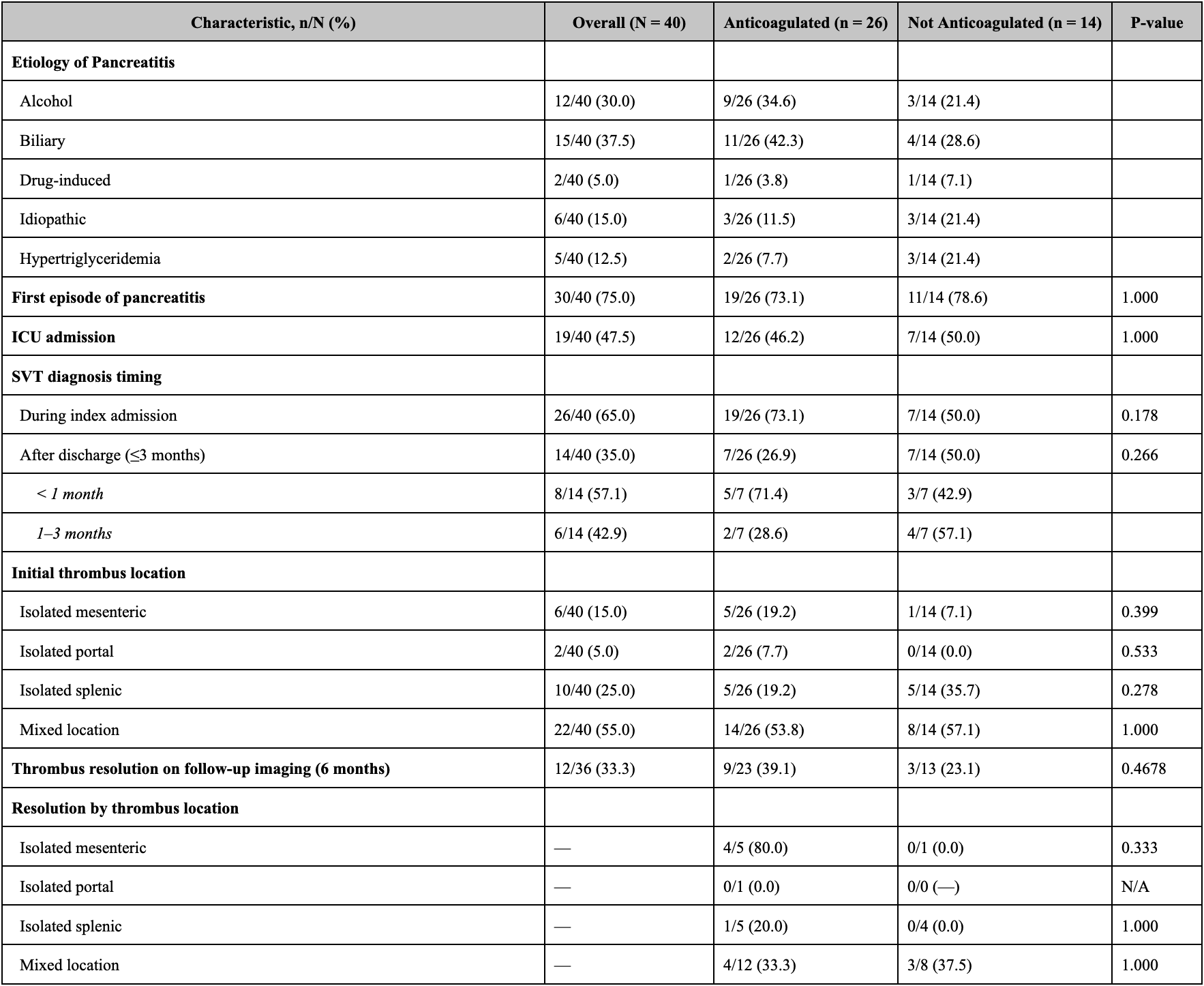
Figure: Thrombus resolution and bleeding risk stratified by thrombus chronicity and local pancreatic complications. Relative risks (RR) were calculated with a 0.05 continuity correction for zero counts.
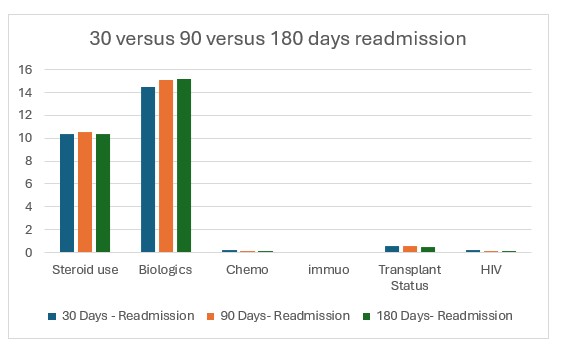
Figure: Clinical Characteristics, Thrombus Resolution and Location Distribution
Disclosures:
Mohammed Abourahma indicated no relevant financial relationships.
Alexander O'Hara indicated no relevant financial relationships.
Muneeb Ansari indicated no relevant financial relationships.
Sebastian Chirayil indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Martin Kalski indicated no relevant financial relationships.
Ayokunle Abegunde indicated no relevant financial relationships.
Dejan Micic indicated no relevant financial relationships.
Mohammed Abourahma, MD1, Alexander O'Hara, MD2, Muneeb Ansari, MD2, Sebastian Chirayil, MD2, Dinkar Ahuja, MD3, Martin Kalski, BS4, Ayokunle T. Abegunde, MD, MBBS, MSc, MRCGP2, Dejan Micic, MD2. P0081 - Systemic Therapy for a Local Problem? Anticoagulation in Pancreatitis-Induced Splanchnic Vein Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
