Sunday Poster Session
Category: Biliary/Pancreas
P0080 - Early Signs of Pancreas Adenocarcinoma Are Often Missed on Cross-Sectional Imaging: Results From a Multicenter Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Benjamin M. Moy, MD
McGaw Medical Center of Northwestern University
Chicago, IL
Presenting Author(s)
Benjamin M. Moy, MD1, Rajesh N. Keswani, MD, MS2
1McGaw Medical Center of Northwestern University, Chicago, IL; 2Feinberg School of Medicine, Northwestern University, Chicago, IL
Introduction: Pancreatic ductal adenocarcinoma (PDAC) is the third leading cause of cancer death. CT or MRI are often the initial diagnostic modalities for detecting PDAC. However, early imaging findings suggesting PDAC may be unappreciated, leading to diagnostic delays. We aimed to determine the prevalence and type of abnormal findings on pre-diagnostic scans in patients later diagnosed with PDAC.
Methods: We identified patients diagnosed with PDAC between September 2023 and February 2025 at one of ten hospitals who had a “pre-diagnostic” scan, defined as any abdominal CT or MRI performed 3-36 months prior to a scan diagnostic for PDAC. These patients were compared to a cohort undergoing cross-sectional imaging for pancreas cancer screening who did not develop PDAC after 5-years longitudinal follow-up (“non-PDAC patients”). Imaging features (e.g., duct dilation or pancreatic atrophy) were collected from procedure reports. The primary outcome was the prevalence of abnormal pancreas imaging findings associated with PDAC on pre-diagnostic scans.
Results: Of 460 PDAC patients during the study period, 103 (22.4%) had a pre-diagnostic scan and comprised the study cohort (mean diagnosis age 72.2 yo, 57.3% female). At time of diagnosis, mean pancreas mass size was 3.2 cm and 35% had metastatic disease. Mean (±SD) time interval between pre-diagnostic and diagnostic scans was 16.0 ± 10.1 months with 62% having a pre-diagnostic scan 3-18 months prior to PDAC diagnosis. Most (78.6%) pre-diagnostic scans were CT scans. Imaging findings associated with PDAC were noted on 31.1% of pre-diagnostic scans (Table). PDAC patients with pre-diagnostic scans were compared to a cohort of non-PDAC patients. Pancreatic cysts were noted in a similar proportion of pre-diagnostic scans (17.5%) and non-PDAC patient scans (24.3%, p=0.3). However, pancreatic duct dilation (9.7% vs 1.9%, p=0.03) and pancreatic atrophy (6.8% vs 1.9%, p=0.17) were observed more frequently in pre-diagnostic scans compared to scans in non-PDAC patients.
Discussion: While > 20% of patients with PDAC had a pre-diagnostic scan, most of these scans had no pancreas abnormalities noted. Despite this “negative” preceding scan, patients presented with large tumors and over one-third had metastatic disease. When present, pancreatic duct dilation and atrophy may suggest early signs of PDAC. However, the paucity of recognized abnormal findings on pre-diagnostic imaging highlights the suboptimal yield of cross-sectional imaging to identify early PDAC.
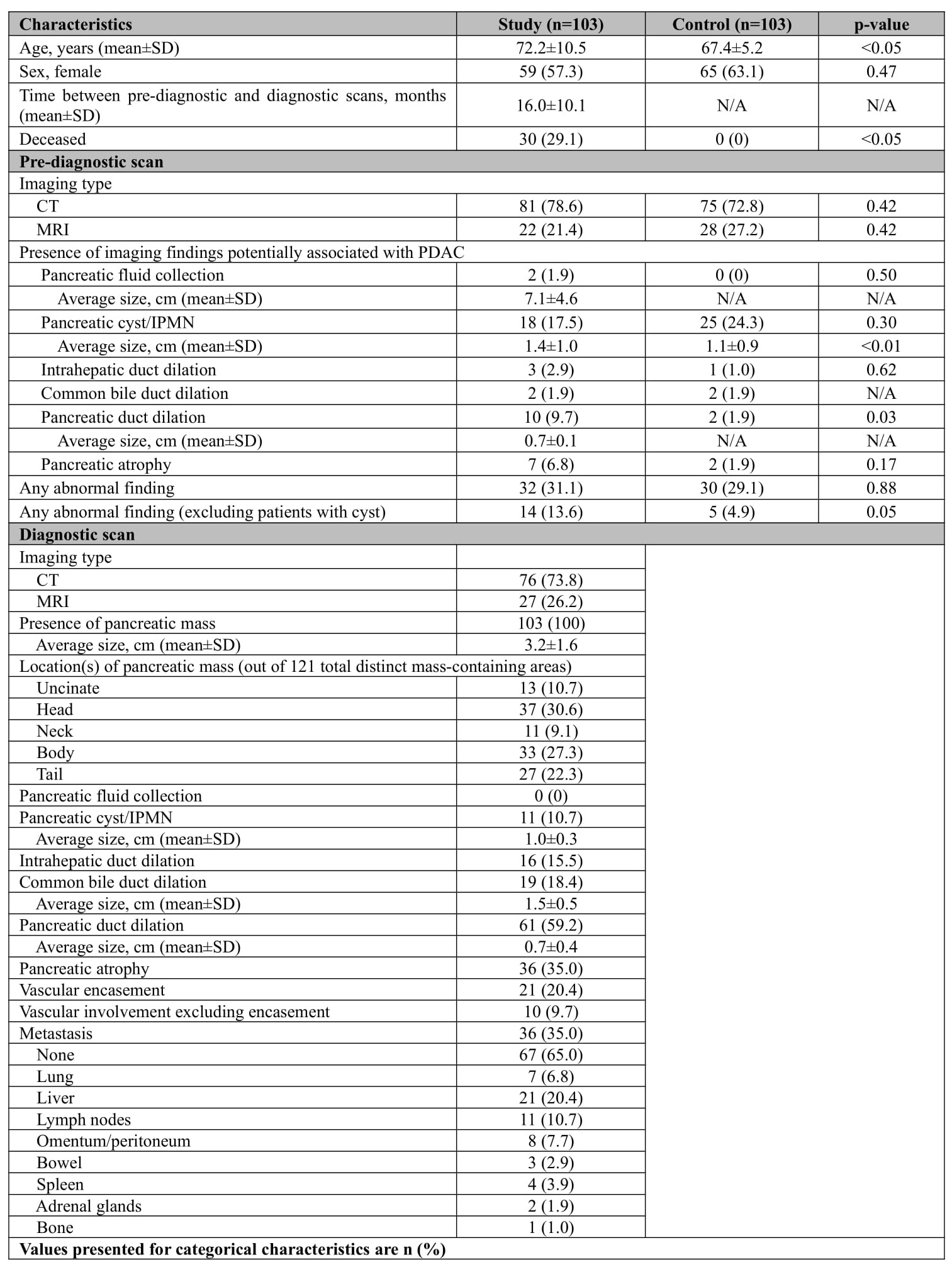
Figure: Table 1. Patient Characteristics and Imaging Findings
Disclosures:
Benjamin Moy indicated no relevant financial relationships.
Rajesh Keswani: Boston Scientific – Consultant. Cook Medical – Consultant. Medtronic, Inc. – Consultant, Grant/Research Support. Neptune Medical – Consultant. Olympus Corporation – Consultant.
Benjamin M. Moy, MD1, Rajesh N. Keswani, MD, MS2. P0080 - Early Signs of Pancreas Adenocarcinoma Are Often Missed on Cross-Sectional Imaging: Results From a Multicenter Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McGaw Medical Center of Northwestern University, Chicago, IL; 2Feinberg School of Medicine, Northwestern University, Chicago, IL
Introduction: Pancreatic ductal adenocarcinoma (PDAC) is the third leading cause of cancer death. CT or MRI are often the initial diagnostic modalities for detecting PDAC. However, early imaging findings suggesting PDAC may be unappreciated, leading to diagnostic delays. We aimed to determine the prevalence and type of abnormal findings on pre-diagnostic scans in patients later diagnosed with PDAC.
Methods: We identified patients diagnosed with PDAC between September 2023 and February 2025 at one of ten hospitals who had a “pre-diagnostic” scan, defined as any abdominal CT or MRI performed 3-36 months prior to a scan diagnostic for PDAC. These patients were compared to a cohort undergoing cross-sectional imaging for pancreas cancer screening who did not develop PDAC after 5-years longitudinal follow-up (“non-PDAC patients”). Imaging features (e.g., duct dilation or pancreatic atrophy) were collected from procedure reports. The primary outcome was the prevalence of abnormal pancreas imaging findings associated with PDAC on pre-diagnostic scans.
Results: Of 460 PDAC patients during the study period, 103 (22.4%) had a pre-diagnostic scan and comprised the study cohort (mean diagnosis age 72.2 yo, 57.3% female). At time of diagnosis, mean pancreas mass size was 3.2 cm and 35% had metastatic disease. Mean (±SD) time interval between pre-diagnostic and diagnostic scans was 16.0 ± 10.1 months with 62% having a pre-diagnostic scan 3-18 months prior to PDAC diagnosis. Most (78.6%) pre-diagnostic scans were CT scans. Imaging findings associated with PDAC were noted on 31.1% of pre-diagnostic scans (Table). PDAC patients with pre-diagnostic scans were compared to a cohort of non-PDAC patients. Pancreatic cysts were noted in a similar proportion of pre-diagnostic scans (17.5%) and non-PDAC patient scans (24.3%, p=0.3). However, pancreatic duct dilation (9.7% vs 1.9%, p=0.03) and pancreatic atrophy (6.8% vs 1.9%, p=0.17) were observed more frequently in pre-diagnostic scans compared to scans in non-PDAC patients.
Discussion: While > 20% of patients with PDAC had a pre-diagnostic scan, most of these scans had no pancreas abnormalities noted. Despite this “negative” preceding scan, patients presented with large tumors and over one-third had metastatic disease. When present, pancreatic duct dilation and atrophy may suggest early signs of PDAC. However, the paucity of recognized abnormal findings on pre-diagnostic imaging highlights the suboptimal yield of cross-sectional imaging to identify early PDAC.
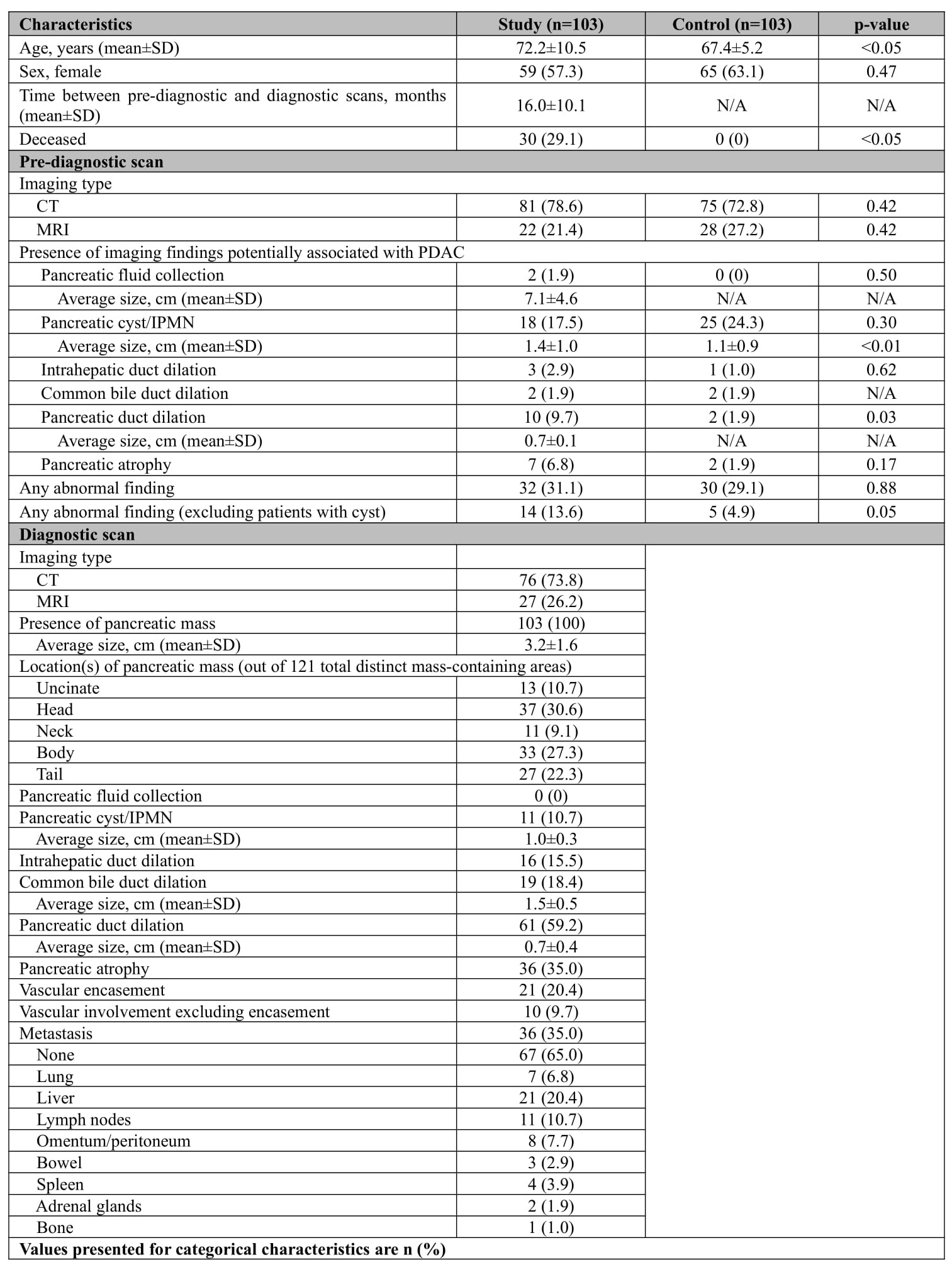
Figure: Table 1. Patient Characteristics and Imaging Findings
Disclosures:
Benjamin Moy indicated no relevant financial relationships.
Rajesh Keswani: Boston Scientific – Consultant. Cook Medical – Consultant. Medtronic, Inc. – Consultant, Grant/Research Support. Neptune Medical – Consultant. Olympus Corporation – Consultant.
Benjamin M. Moy, MD1, Rajesh N. Keswani, MD, MS2. P0080 - Early Signs of Pancreas Adenocarcinoma Are Often Missed on Cross-Sectional Imaging: Results From a Multicenter Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

