Sunday Poster Session
Category: Biliary/Pancreas
P0067 - Comparative Effectiveness of Neuromodulation and Pharmacotherapy in Chronic Pancreatitis Pain: Systemic Review and Insights From Published Literature
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Akanksha Togra, MD (she/her/hers)
Texas Tech University Health Sciences Center, El Paso
El Paso, TX
Presenting Author(s)
Akanksha Togra, MD1, M. Ammar Kalas, MD2, Keith Garrison, MD2, Alejandro Robles, MD3, Paul Estrada, MD4, Nirav Thosani, MD5, Sherif E. Elhanafi, MD2
1Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX; 4Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 5University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Management for chronic pancreatitis (CP) is primarily focused on symptomatic relief of abdominal pain. CP associated pain is multifactorial, involving nociceptive, neuropathic, and centrally sensitized mechanisms. Despite its high burden, evidence-based treatment options remain limited. The aim of this study is to critically evaluate available interventions and compare effectiveness of both neuromodulation and pharmacotherapy for pain management in CP.
Methods: A systematic PubMed literature search identified 22 randomized controlled trials (RCTs) evaluating pain management strategies in CP, of which 4 pharmacological and 5 neuromodulation based interventions were included. Data on pain relief outcomes and responder rates were extracted. Mean difference (MD) with its confidence interval (CI) were used as measures of association.
Results: In neuromodulation group analysis (Figure 1), 2 interventions showed significant positive result compared to placebo. Effect of repetitive transcranial magnetic stimulation (rTMS) (MD 26.10, 95% CI 6.18 to 46.02) and acupuncture (MD 42.00, 95% CI 17.81 to 66.19) showed positive effect. While spinal cord stimulation (MD -0.10, 95% CI -1.56 to 1.36), vagal neuromodulation (MD -1.10, 95% CI -2.66 to 0.46) and internet cognitive behavioural therapy (MD -1.00, 95% CI -2.47 to 0.47) did not have significant impact on pain management.
In pharmacotherapy group analysis (Figure 2) only pregabalin showed a significant positive result compared to placebo (MD 12, 95% CI 10.22 to 13.78). Other pharmacotherapies including endothelium (MD -1.87, 95% CI -2.89 to -0.85), octreotide (MD 0.90, 95% CI -3.65 to 5.45) and antioxidant (MD -0.36, 95% CI -0.71 to 1.43) did not show any significant effect. It is noteworthy that while analgesics are key for managing pain in CP, we found no RCTs specifically evaluating these medications.
Discussion: In this study, repetitive transcranial magnetic stimulation (rTMS) and pregabalin emerged as the most effective modalities for managing chronic pancreatitis-related pain, likely due to their shared neuromodulatory mechanism. To our knowledge, this is the first report to propose a common neuromodulatory basis underlying both pharmacologic and non-pharmacologic interventions in this setting. These findings position neuromodulation as a potential central therapeutic strategy, underscoring the need for further research into its mechanisms and the possible additive or synergistic benefits of integrating it with conventional pain management.
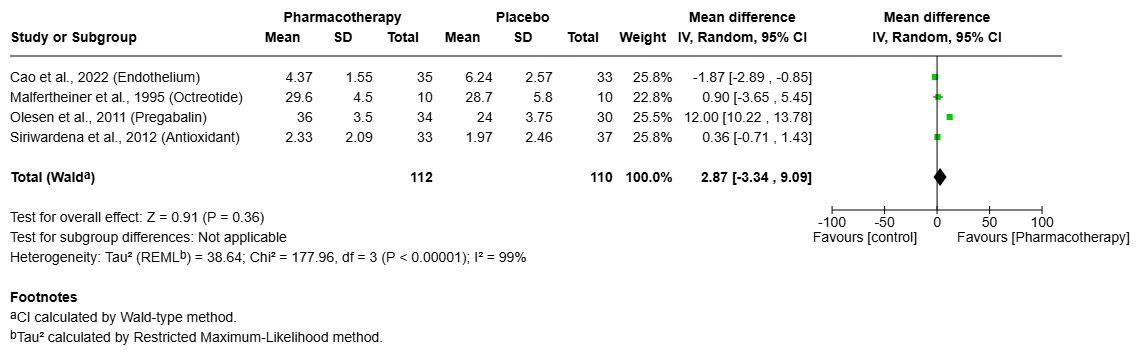
Figure: Neuromodulation in CP Pain Management
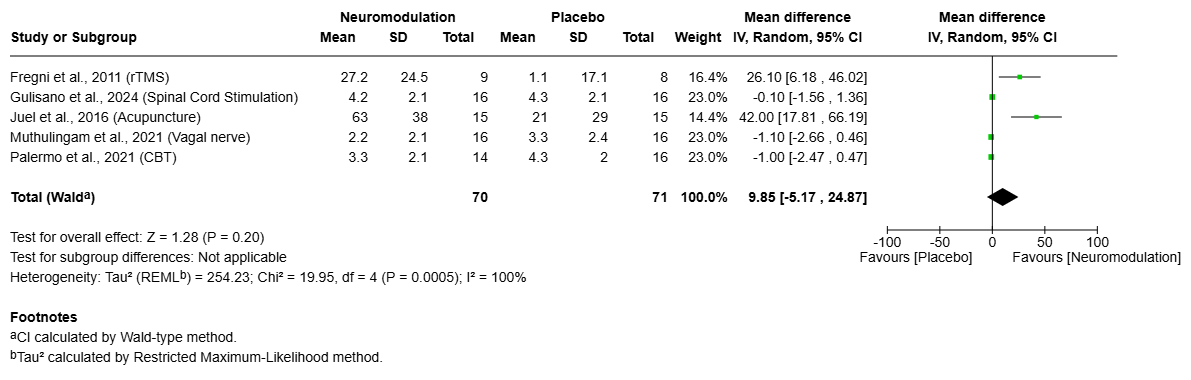
Figure: Pharmacotherapy in CP Pain Management
Disclosures:
Akanksha Togra indicated no relevant financial relationships.
M. Ammar Kalas indicated no relevant financial relationships.
Keith Garrison indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Paul Estrada indicated no relevant financial relationships.
Nirav Thosani: Alpfa medical – Consultant. Roseaid – Creatorship rights.
Sherif Elhanafi indicated no relevant financial relationships.
Akanksha Togra, MD1, M. Ammar Kalas, MD2, Keith Garrison, MD2, Alejandro Robles, MD3, Paul Estrada, MD4, Nirav Thosani, MD5, Sherif E. Elhanafi, MD2. P0067 - Comparative Effectiveness of Neuromodulation and Pharmacotherapy in Chronic Pancreatitis Pain: Systemic Review and Insights From Published Literature, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Department of Gastroenterology, Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center El Paso, El Paso , TX, El Paso, TX; 4Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 5University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Management for chronic pancreatitis (CP) is primarily focused on symptomatic relief of abdominal pain. CP associated pain is multifactorial, involving nociceptive, neuropathic, and centrally sensitized mechanisms. Despite its high burden, evidence-based treatment options remain limited. The aim of this study is to critically evaluate available interventions and compare effectiveness of both neuromodulation and pharmacotherapy for pain management in CP.
Methods: A systematic PubMed literature search identified 22 randomized controlled trials (RCTs) evaluating pain management strategies in CP, of which 4 pharmacological and 5 neuromodulation based interventions were included. Data on pain relief outcomes and responder rates were extracted. Mean difference (MD) with its confidence interval (CI) were used as measures of association.
Results: In neuromodulation group analysis (Figure 1), 2 interventions showed significant positive result compared to placebo. Effect of repetitive transcranial magnetic stimulation (rTMS) (MD 26.10, 95% CI 6.18 to 46.02) and acupuncture (MD 42.00, 95% CI 17.81 to 66.19) showed positive effect. While spinal cord stimulation (MD -0.10, 95% CI -1.56 to 1.36), vagal neuromodulation (MD -1.10, 95% CI -2.66 to 0.46) and internet cognitive behavioural therapy (MD -1.00, 95% CI -2.47 to 0.47) did not have significant impact on pain management.
In pharmacotherapy group analysis (Figure 2) only pregabalin showed a significant positive result compared to placebo (MD 12, 95% CI 10.22 to 13.78). Other pharmacotherapies including endothelium (MD -1.87, 95% CI -2.89 to -0.85), octreotide (MD 0.90, 95% CI -3.65 to 5.45) and antioxidant (MD -0.36, 95% CI -0.71 to 1.43) did not show any significant effect. It is noteworthy that while analgesics are key for managing pain in CP, we found no RCTs specifically evaluating these medications.
Discussion: In this study, repetitive transcranial magnetic stimulation (rTMS) and pregabalin emerged as the most effective modalities for managing chronic pancreatitis-related pain, likely due to their shared neuromodulatory mechanism. To our knowledge, this is the first report to propose a common neuromodulatory basis underlying both pharmacologic and non-pharmacologic interventions in this setting. These findings position neuromodulation as a potential central therapeutic strategy, underscoring the need for further research into its mechanisms and the possible additive or synergistic benefits of integrating it with conventional pain management.
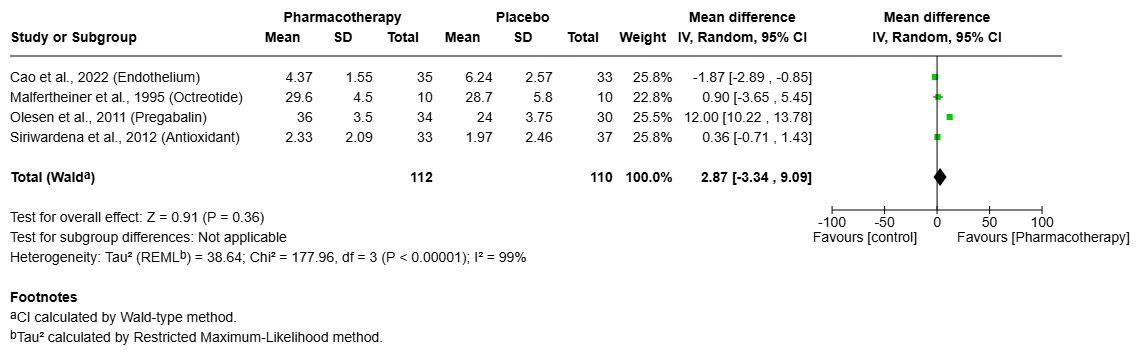
Figure: Neuromodulation in CP Pain Management
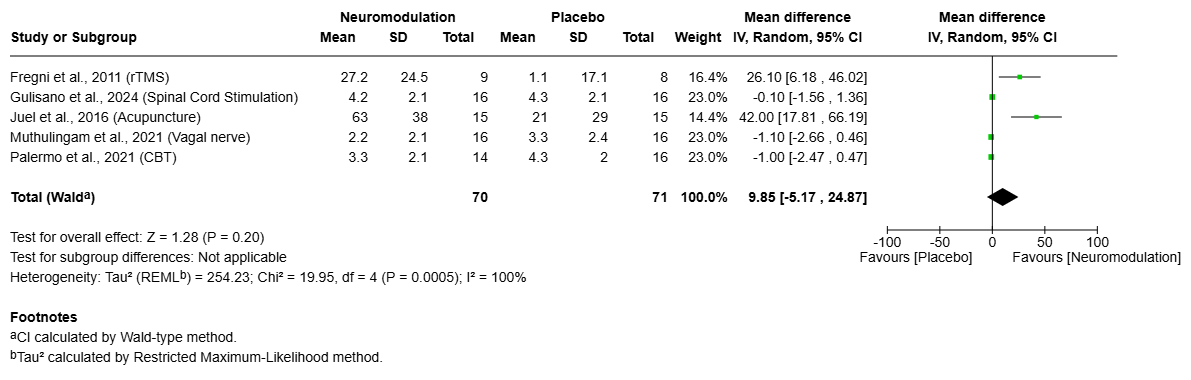
Figure: Pharmacotherapy in CP Pain Management
Disclosures:
Akanksha Togra indicated no relevant financial relationships.
M. Ammar Kalas indicated no relevant financial relationships.
Keith Garrison indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Paul Estrada indicated no relevant financial relationships.
Nirav Thosani: Alpfa medical – Consultant. Roseaid – Creatorship rights.
Sherif Elhanafi indicated no relevant financial relationships.
Akanksha Togra, MD1, M. Ammar Kalas, MD2, Keith Garrison, MD2, Alejandro Robles, MD3, Paul Estrada, MD4, Nirav Thosani, MD5, Sherif E. Elhanafi, MD2. P0067 - Comparative Effectiveness of Neuromodulation and Pharmacotherapy in Chronic Pancreatitis Pain: Systemic Review and Insights From Published Literature, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
