Sunday Poster Session
Category: Biliary/Pancreas
P0064 - Burden of Cardiovascular Mortality in Older Adults With Pancreatic Cancer: A 25-Year US Retrospective Study With Sensitivity Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- CC
Corinne Caissie, MD
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Corinne Caissie, MD1, Simran Joshi, MD1, Muhammad Faizan Ali, MD2, Husnain Ahmad, MBBS3, Sherif Eltawansy, MD4, Ali Hassan, MBBS3, Saman Javaid, MBBS5, Noor ul Ain Saleem, 6, Muhammad Khan, MBBS7, Mohammad Islam, MD8, Cheng-Hung Tai, MD1, Sushrut Ingawale, MD, DNB, MBBS9, Pujitha Vallivedu Chennakesavulu, MD, MBBS10, Preethi Jagannath, MBBS11, Matthew Antony. Manoj, MBBS12
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Jinnah Postgraduate Medical Centre, Karachi, Sindh, Pakistan; 3Shalamar Institute of Health Sciences, Lahore, Punjab, Pakistan; 4Jersey Shore University Medical Center, Jersey Shore, NJ; 5CMH Kharian, Sarghoda, Punjab, Pakistan; 6Fatima Memorial Hospital, Lahore, Punjab, Pakistan; 7Bacha Khan Medical College, Mardan, Punjab, Pakistan; 8Yale New Haven Health, Bridgeport, CT; 9Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT; 10Quinnipiac University Frank H Netter School of Medicine/ St Vincent medical center, Bridgeport, CT; 11Mount Auburn Hospital, Cambridge, MA; 12Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Pancreatic cancer (PC) carries a high mortality rate, often compounded by co-morbid conditions such as cardiovascular disease (CVD), which may further worsen patient outcomes. Older adults with PC are particularly vulnerable due to shared risk factors like inflammation, metabolic dysfunction, and treatment-related cardio-toxicity. Despite this, the specific impact of different CVD subtypes on mortality in this population remains poorly defined. This study aims to analyze long-term trends in CVD-related mortality among older adults with PC in the US and identify which CV conditions contribute most significantly to mortality risk.
Methods: Mortality data from CDC WONDER (1999–2023) were analyzed using Joinpoint regression to assess deaths related to PC and CVD in U.S. adults aged 65+. Age-adjusted mortality rates (AAMRs) and average annual percent change (AAPC) with 95% CI were calculated. Furthermore, sensitivity analysis was performed to identify which CVD contributes most to the burden in patients with PC.
Results: A total of 187,120 deaths were attributed to the combined burden of CVD and PC. From 1999 to 2023, the overall AAMR increased from 16.49 to 21.18 (AAPC: 1.11; 95% CI: 0.95–1.25). Men consistently exhibited higher mortality than women (AAMR: 20.08 vs.
14.90) and experienced a steeper increase over time (AAPC: 1.43 vs. 0.77). Non-Hispanic (NH) Black individuals faced the highest mortality burden (AAMR: 23.12), while NH Whites showed the most significant rise (AAPC: 1.34). Among U.S. Census regions,
the Northeast reported the highest mortality (AAMR: 20.82), but the South demonstrated the fastest rise (AAPC: 1.71). State-level variation was notable, with Nebraska reporting the highest AAMR (29.21) and Utah the lowest (11.09). Urban areas had a slightly higher AAMR than rural areas (16.74 vs. 15.87), though rural populations experienced a more rapid rise in mortality (AAPC: 1.21 vs. 0.62). Sensitivity analysis revealed that the comorbidity of PC with hypertensive diseases had the steepest increase in mortality (AAPC: 5.16), followed by pulmonary heart disease (AAPC: 5.09) and arrhythmias (AAPC: 4.67).
Discussion: PC patients with coexisting CVD face a rising mortality burden, with disproportionate increases observed in men, NH Blacks, and rural populations. The steepest mortality surges occurred in cases involving hypertensive disease, pulmonary heart disease, and
arrhythmias—highlighting critical targets for CV risk stratification and intervention in this high-risk cohort.
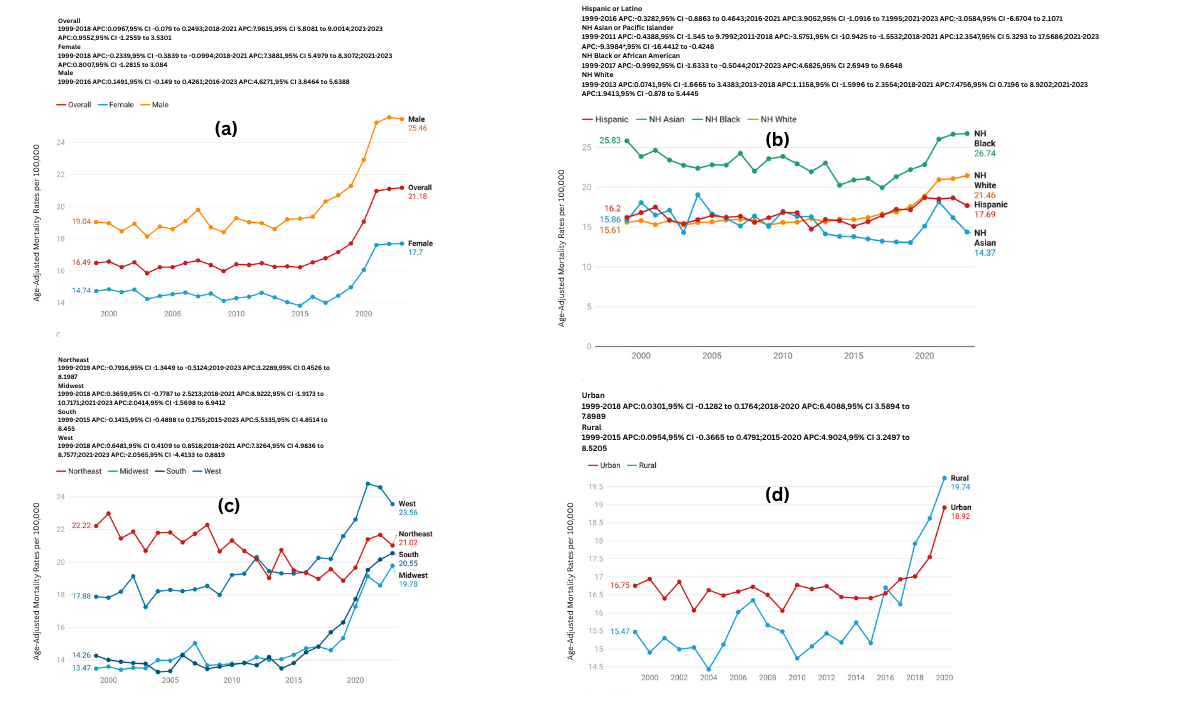
Figure: Trend Graft for a 25-Year U.S. Retrospective Study with Sensitivity Analysis of Burden of Cardiovascular Mortality in Older Adults With Pancreatic Cancer
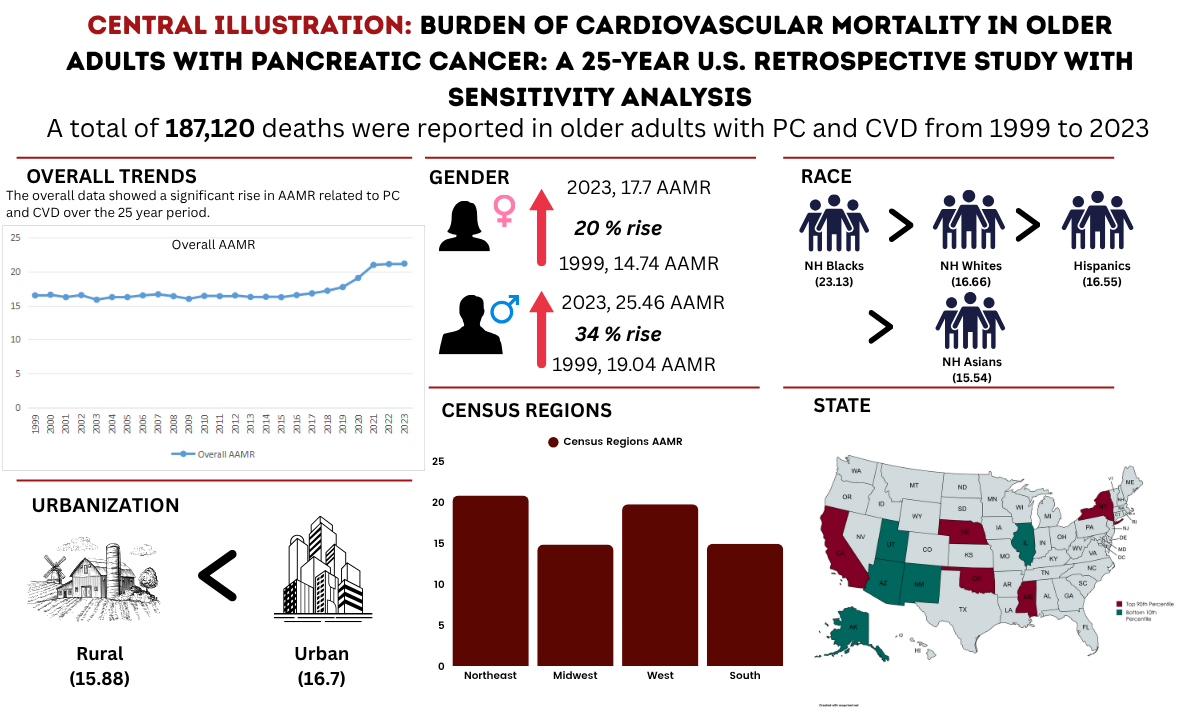
Figure: Central Illustration: Burden of Cardiovascular Mortality in Older Adults With Pancreatic Cancer: A 25-Year U.S. Retrospective Study with Sensitivity Analysis
Disclosures:
Corinne Caissie indicated no relevant financial relationships.
Simran Joshi indicated no relevant financial relationships.
Muhammad Faizan Ali indicated no relevant financial relationships.
Husnain Ahmad indicated no relevant financial relationships.
Sherif Eltawansy indicated no relevant financial relationships.
Ali Hassan indicated no relevant financial relationships.
Saman Javaid indicated no relevant financial relationships.
Noor ul Ain Saleem indicated no relevant financial relationships.
Muhammad Khan indicated no relevant financial relationships.
Mohammad Islam indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Pujitha Vallivedu Chennakesavulu indicated no relevant financial relationships.
Preethi Jagannath indicated no relevant financial relationships.
Matthew Manoj indicated no relevant financial relationships.
Corinne Caissie, MD1, Simran Joshi, MD1, Muhammad Faizan Ali, MD2, Husnain Ahmad, MBBS3, Sherif Eltawansy, MD4, Ali Hassan, MBBS3, Saman Javaid, MBBS5, Noor ul Ain Saleem, 6, Muhammad Khan, MBBS7, Mohammad Islam, MD8, Cheng-Hung Tai, MD1, Sushrut Ingawale, MD, DNB, MBBS9, Pujitha Vallivedu Chennakesavulu, MD, MBBS10, Preethi Jagannath, MBBS11, Matthew Antony. Manoj, MBBS12. P0064 - Burden of Cardiovascular Mortality in Older Adults With Pancreatic Cancer: A 25-Year US Retrospective Study With Sensitivity Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Jinnah Postgraduate Medical Centre, Karachi, Sindh, Pakistan; 3Shalamar Institute of Health Sciences, Lahore, Punjab, Pakistan; 4Jersey Shore University Medical Center, Jersey Shore, NJ; 5CMH Kharian, Sarghoda, Punjab, Pakistan; 6Fatima Memorial Hospital, Lahore, Punjab, Pakistan; 7Bacha Khan Medical College, Mardan, Punjab, Pakistan; 8Yale New Haven Health, Bridgeport, CT; 9Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT; 10Quinnipiac University Frank H Netter School of Medicine/ St Vincent medical center, Bridgeport, CT; 11Mount Auburn Hospital, Cambridge, MA; 12Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Pancreatic cancer (PC) carries a high mortality rate, often compounded by co-morbid conditions such as cardiovascular disease (CVD), which may further worsen patient outcomes. Older adults with PC are particularly vulnerable due to shared risk factors like inflammation, metabolic dysfunction, and treatment-related cardio-toxicity. Despite this, the specific impact of different CVD subtypes on mortality in this population remains poorly defined. This study aims to analyze long-term trends in CVD-related mortality among older adults with PC in the US and identify which CV conditions contribute most significantly to mortality risk.
Methods: Mortality data from CDC WONDER (1999–2023) were analyzed using Joinpoint regression to assess deaths related to PC and CVD in U.S. adults aged 65+. Age-adjusted mortality rates (AAMRs) and average annual percent change (AAPC) with 95% CI were calculated. Furthermore, sensitivity analysis was performed to identify which CVD contributes most to the burden in patients with PC.
Results: A total of 187,120 deaths were attributed to the combined burden of CVD and PC. From 1999 to 2023, the overall AAMR increased from 16.49 to 21.18 (AAPC: 1.11; 95% CI: 0.95–1.25). Men consistently exhibited higher mortality than women (AAMR: 20.08 vs.
14.90) and experienced a steeper increase over time (AAPC: 1.43 vs. 0.77). Non-Hispanic (NH) Black individuals faced the highest mortality burden (AAMR: 23.12), while NH Whites showed the most significant rise (AAPC: 1.34). Among U.S. Census regions,
the Northeast reported the highest mortality (AAMR: 20.82), but the South demonstrated the fastest rise (AAPC: 1.71). State-level variation was notable, with Nebraska reporting the highest AAMR (29.21) and Utah the lowest (11.09). Urban areas had a slightly higher AAMR than rural areas (16.74 vs. 15.87), though rural populations experienced a more rapid rise in mortality (AAPC: 1.21 vs. 0.62). Sensitivity analysis revealed that the comorbidity of PC with hypertensive diseases had the steepest increase in mortality (AAPC: 5.16), followed by pulmonary heart disease (AAPC: 5.09) and arrhythmias (AAPC: 4.67).
Discussion: PC patients with coexisting CVD face a rising mortality burden, with disproportionate increases observed in men, NH Blacks, and rural populations. The steepest mortality surges occurred in cases involving hypertensive disease, pulmonary heart disease, and
arrhythmias—highlighting critical targets for CV risk stratification and intervention in this high-risk cohort.
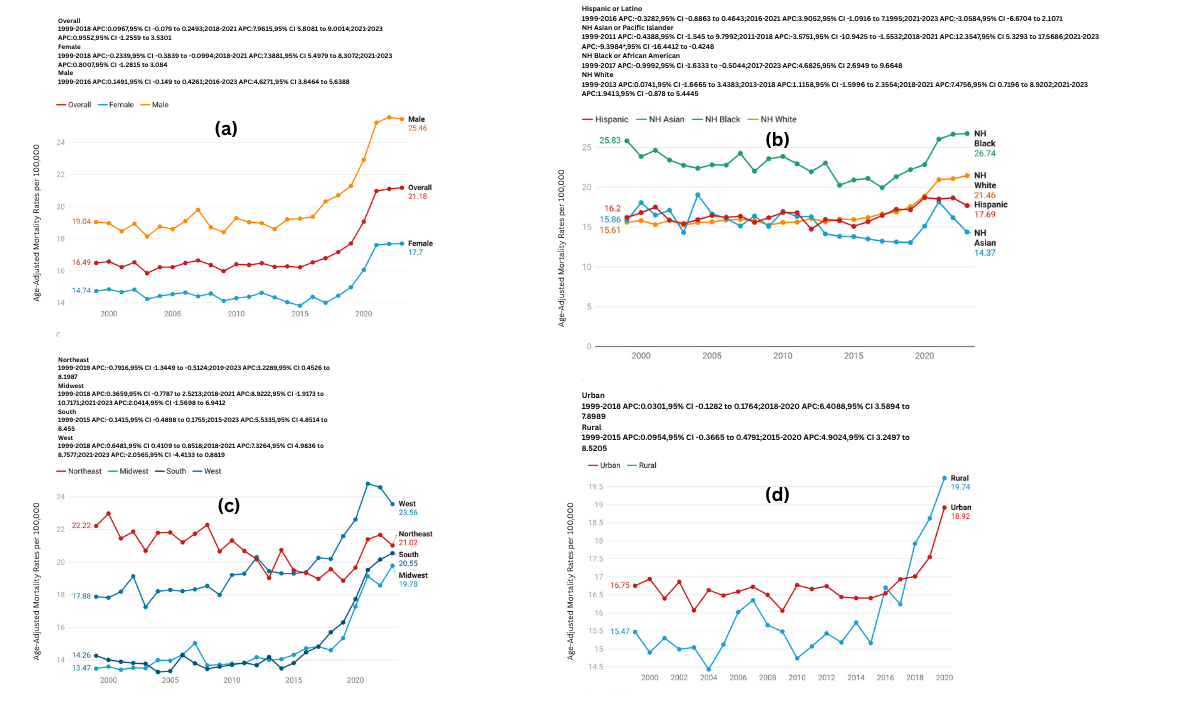
Figure: Trend Graft for a 25-Year U.S. Retrospective Study with Sensitivity Analysis of Burden of Cardiovascular Mortality in Older Adults With Pancreatic Cancer
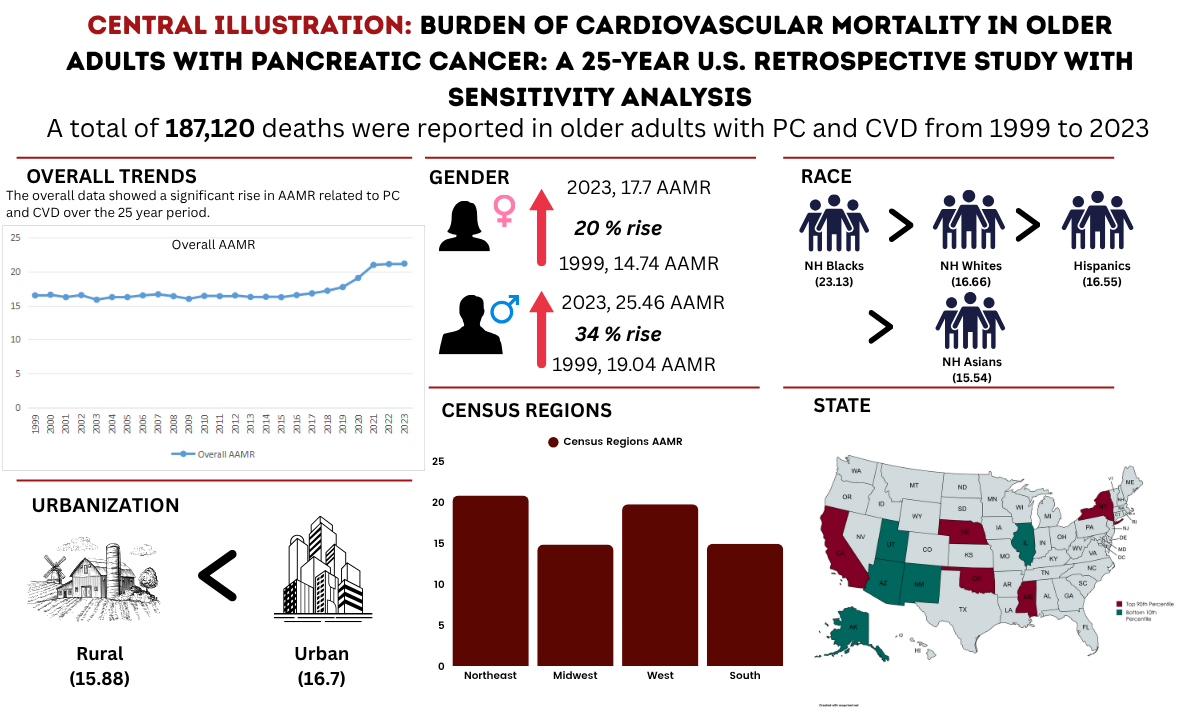
Figure: Central Illustration: Burden of Cardiovascular Mortality in Older Adults With Pancreatic Cancer: A 25-Year U.S. Retrospective Study with Sensitivity Analysis
Disclosures:
Corinne Caissie indicated no relevant financial relationships.
Simran Joshi indicated no relevant financial relationships.
Muhammad Faizan Ali indicated no relevant financial relationships.
Husnain Ahmad indicated no relevant financial relationships.
Sherif Eltawansy indicated no relevant financial relationships.
Ali Hassan indicated no relevant financial relationships.
Saman Javaid indicated no relevant financial relationships.
Noor ul Ain Saleem indicated no relevant financial relationships.
Muhammad Khan indicated no relevant financial relationships.
Mohammad Islam indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Pujitha Vallivedu Chennakesavulu indicated no relevant financial relationships.
Preethi Jagannath indicated no relevant financial relationships.
Matthew Manoj indicated no relevant financial relationships.
Corinne Caissie, MD1, Simran Joshi, MD1, Muhammad Faizan Ali, MD2, Husnain Ahmad, MBBS3, Sherif Eltawansy, MD4, Ali Hassan, MBBS3, Saman Javaid, MBBS5, Noor ul Ain Saleem, 6, Muhammad Khan, MBBS7, Mohammad Islam, MD8, Cheng-Hung Tai, MD1, Sushrut Ingawale, MD, DNB, MBBS9, Pujitha Vallivedu Chennakesavulu, MD, MBBS10, Preethi Jagannath, MBBS11, Matthew Antony. Manoj, MBBS12. P0064 - Burden of Cardiovascular Mortality in Older Adults With Pancreatic Cancer: A 25-Year US Retrospective Study With Sensitivity Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
