Sunday Poster Session
Category: Biliary/Pancreas
P0034 - Delayed Palliative Care Consultation Among Veterans With Pancreatic Cancer: An Analysis of Patterns and Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Akhil Adla, DO
University of Tennessee Health Science Center
Memphis, TN
Presenting Author(s)
Akhil Adla, DO1, Hayes Walker, MD2, Samantha Whitwell, MD2, Louis Yn, MD3, Claudio Tombazzi, MD4
1University of Tennessee Health Science Center, Memphis, TN; 2UTHSC, Memphis, TN; 3University of Tennessee Health Science Center - Methodist University Hospital, Memphis, TN; 4VA Memphis Health Care, Memphis, TN
Introduction: Pancreatic cancer is characterized by a rapid disease progression, and poor overall prognosis, necessitating a comprehensive approach to care. The American Society of Clinical Oncology (ASCO) strongly recommends early palliative care consultation for all advanced pancreatic cancer patients, at the time of diagnosis or within the 8-12 weeks of diagnosis [1]. Timely palliative care involvement has been shown to improve symptom management, mood, and improved survival[2][3][4]. Despite these benefits, palliative care referrals are often delayed, limiting the potential impact on patient outcomes.
Methods: A retrospective chart review was conducted of veterans diagnosed with pancreatic cancer from 2014 to 2024, utilizing the Computerized Patient Record System (CPRS) within the Veterans Health Administration (VHA). Observed variables included age, sex, race, stage at diagnosis, modifiable risk factors, treatment modalities, timing and frequency of palliative care referral, and overall survival. Comparative analyses were performed to assess associations among these factors.
Results: Overall, 54.7% of patients received palliative care consultation. 21.7% of patients never received palliative care. 23.6% of patients had missing or unknown palliative care status. Data for overall survival (OS) was missing for 12 patients (10.2%). Patients had a mean time from diagnosis to palliative care consultation of 148 days, median of 42 days, with a range of 0 to 841 days (25th%=14 days, 75th%=189 days). Patients in this study lived more than half their survival time without palliative care support. Patients who received palliative care had a mean OS of 532 days and a median OS of 245 days. Patients who never received palliative care had a mean OS of 486 days and a median OS of 198 days (p=0.72). Patient geographic distribution was 67.9% urban and 32.1% rural. In this data set, palliative care consultation rates for rural and urban patients were 63% and 53%, respectively (p=0.31).
Discussion: This study reveals a dramatic percentage of patients who did not have palliative care consultations in a timely fashion as recommended by ASCO. As this study was retrospective, we cannot glean whether the end-of-life experience was improved with the involvement of palliative care, despite there not being significant differences in OS. Utilizing the data, an internal quality improvement project was proposed at the VA to create a protocol to ensure early palliative care consultation in this vulnerable patient population.
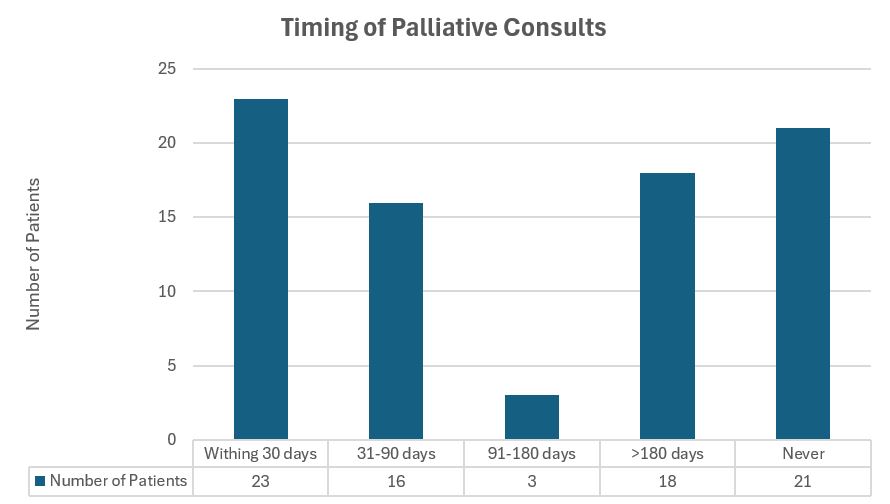
Figure: Figure A: 20.2% of pancreatic patients received a palliative consult within 30 days of diagnosis. 18.4% of patients did not receive a palliative consult and the status of 28.9% of patients is unknown.
Disclosures:
Akhil Adla indicated no relevant financial relationships.
Hayes Walker indicated no relevant financial relationships.
Samantha Whitwell indicated no relevant financial relationships.
Louis Yn indicated no relevant financial relationships.
Claudio Tombazzi indicated no relevant financial relationships.
Akhil Adla, DO1, Hayes Walker, MD2, Samantha Whitwell, MD2, Louis Yn, MD3, Claudio Tombazzi, MD4. P0034 - Delayed Palliative Care Consultation Among Veterans With Pancreatic Cancer: An Analysis of Patterns and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Tennessee Health Science Center, Memphis, TN; 2UTHSC, Memphis, TN; 3University of Tennessee Health Science Center - Methodist University Hospital, Memphis, TN; 4VA Memphis Health Care, Memphis, TN
Introduction: Pancreatic cancer is characterized by a rapid disease progression, and poor overall prognosis, necessitating a comprehensive approach to care. The American Society of Clinical Oncology (ASCO) strongly recommends early palliative care consultation for all advanced pancreatic cancer patients, at the time of diagnosis or within the 8-12 weeks of diagnosis [1]. Timely palliative care involvement has been shown to improve symptom management, mood, and improved survival[2][3][4]. Despite these benefits, palliative care referrals are often delayed, limiting the potential impact on patient outcomes.
Methods: A retrospective chart review was conducted of veterans diagnosed with pancreatic cancer from 2014 to 2024, utilizing the Computerized Patient Record System (CPRS) within the Veterans Health Administration (VHA). Observed variables included age, sex, race, stage at diagnosis, modifiable risk factors, treatment modalities, timing and frequency of palliative care referral, and overall survival. Comparative analyses were performed to assess associations among these factors.
Results: Overall, 54.7% of patients received palliative care consultation. 21.7% of patients never received palliative care. 23.6% of patients had missing or unknown palliative care status. Data for overall survival (OS) was missing for 12 patients (10.2%). Patients had a mean time from diagnosis to palliative care consultation of 148 days, median of 42 days, with a range of 0 to 841 days (25th%=14 days, 75th%=189 days). Patients in this study lived more than half their survival time without palliative care support. Patients who received palliative care had a mean OS of 532 days and a median OS of 245 days. Patients who never received palliative care had a mean OS of 486 days and a median OS of 198 days (p=0.72). Patient geographic distribution was 67.9% urban and 32.1% rural. In this data set, palliative care consultation rates for rural and urban patients were 63% and 53%, respectively (p=0.31).
Discussion: This study reveals a dramatic percentage of patients who did not have palliative care consultations in a timely fashion as recommended by ASCO. As this study was retrospective, we cannot glean whether the end-of-life experience was improved with the involvement of palliative care, despite there not being significant differences in OS. Utilizing the data, an internal quality improvement project was proposed at the VA to create a protocol to ensure early palliative care consultation in this vulnerable patient population.
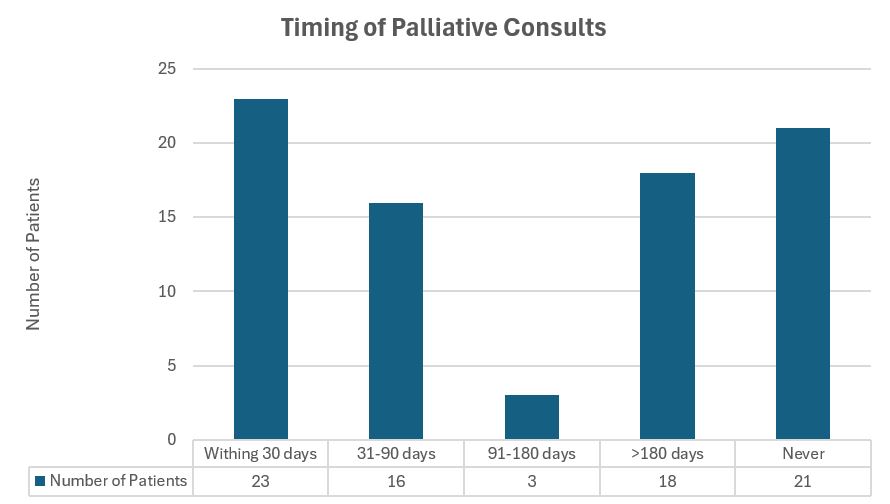
Figure: Figure A: 20.2% of pancreatic patients received a palliative consult within 30 days of diagnosis. 18.4% of patients did not receive a palliative consult and the status of 28.9% of patients is unknown.
Disclosures:
Akhil Adla indicated no relevant financial relationships.
Hayes Walker indicated no relevant financial relationships.
Samantha Whitwell indicated no relevant financial relationships.
Louis Yn indicated no relevant financial relationships.
Claudio Tombazzi indicated no relevant financial relationships.
Akhil Adla, DO1, Hayes Walker, MD2, Samantha Whitwell, MD2, Louis Yn, MD3, Claudio Tombazzi, MD4. P0034 - Delayed Palliative Care Consultation Among Veterans With Pancreatic Cancer: An Analysis of Patterns and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

