Sunday Poster Session
Category: Biliary/Pancreas
P0016 - Early CRP Trends and Phenotypes Predict Mortality in Acute Pancreatitis: A Trajectory-Based Analysis With Implications for Resource Optimization
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SV
Samir Vanani, MBBS
Surat Institute of Digestive Sciences Hospital
Surat, Gujarat, India
Presenting Author(s)
Award: ACG Presidential Poster Award
Samir Vanani, MBBS1, Mipasha Patel, MD2, Dhvani Adhvaryu, PharmD1, Nishtha Nandwani, MBBS1, Aarya Desai, BSc1, Dhiraaj Desai, BE1, Rajiv Mehta, MD, DNB1
1Surat Institute of Digestive Sciences Hospital, Surat, Gujarat, India; 2Jefferson Abington Hospital, Willow Grove, PA
Introduction: C-reactive protein (CRP) is commonly used in acute pancreatitis (AP) to assess severity, but the value of early serial CRP trends for mortality prediction is unclear. We evaluated whether changes over the first 4-5 days can improve risk stratification and guide clinical decision-making.
Methods: We ambispectively analyzed 372 AP patients (median age: 39 [IQR 30-54]; 80% male) with serial CRP values recorded from days 2 to 5 of symptom onset (CRP2-CRP5). Missing values were imputed using constrained interpolation or iterative regression. Post-imputation analyses showed consistent trends and predictive performance compared to complete-case data. K-means clustering identified CRP trajectory phenotypes. Logistic regression, ROC analysis, and decision curve analysis (DCA) assessed mortality prediction and net clinical benefit. Subgroup analysis was performed by CRP2 level and BISAP score.
Results: Overall mortality was 6.2% (n=23). Mean CRP declined from 250 mg/L (day 2) to 134 mg/L (day 5). Trajectory clustering revealed two phenotypes, resolving CRP (mortality 2.2%) and persistently elevated CRP (mortality 12.4%; OR=6.29). A model using CRP2-CRP4 yielded strong discrimination for mortality (AUC=0.809; 95% CI: 0.689–0.911). Overall, a CRP4/CRP2 ratio ≥0.90 predicted mortality with AUC of 0.64. In patients with CRP2 >300 mg/L (n=134), predictive performance improved (AUC = 0.820, NPV = 93.9%), highlighting its utility in high-baseline inflammation states. Predictive trends remained consistent across etiologies and robust across sensitivity analyses. Decision curve analysis showed that adding CRP5 to the model of CRP2-4 provided minimal incremental benefit (AUC gain of +0.002)), with a maximum net benefit of 0.0064 at a threshold probability of 0.27, suggesting most prognostic information is captured by Day 4. Early CRP trends can inform ICU triage, escalation of care, and early discharge planning, supporting more efficient resource allocation.
Discussion: CRP trajectories through Day 4 define meaningful phenotypes in AP. The CRP4/CRP2 ratio provides modest overall discrimination but is highly predictive in patients with elevated baseline CRP. The limited added value of day 5 CRP supports more efficient care pathways, especially in settings with constrained resources. Early CRP trends offer a practical, scalable tool for personalized and resource-conscious AP care.
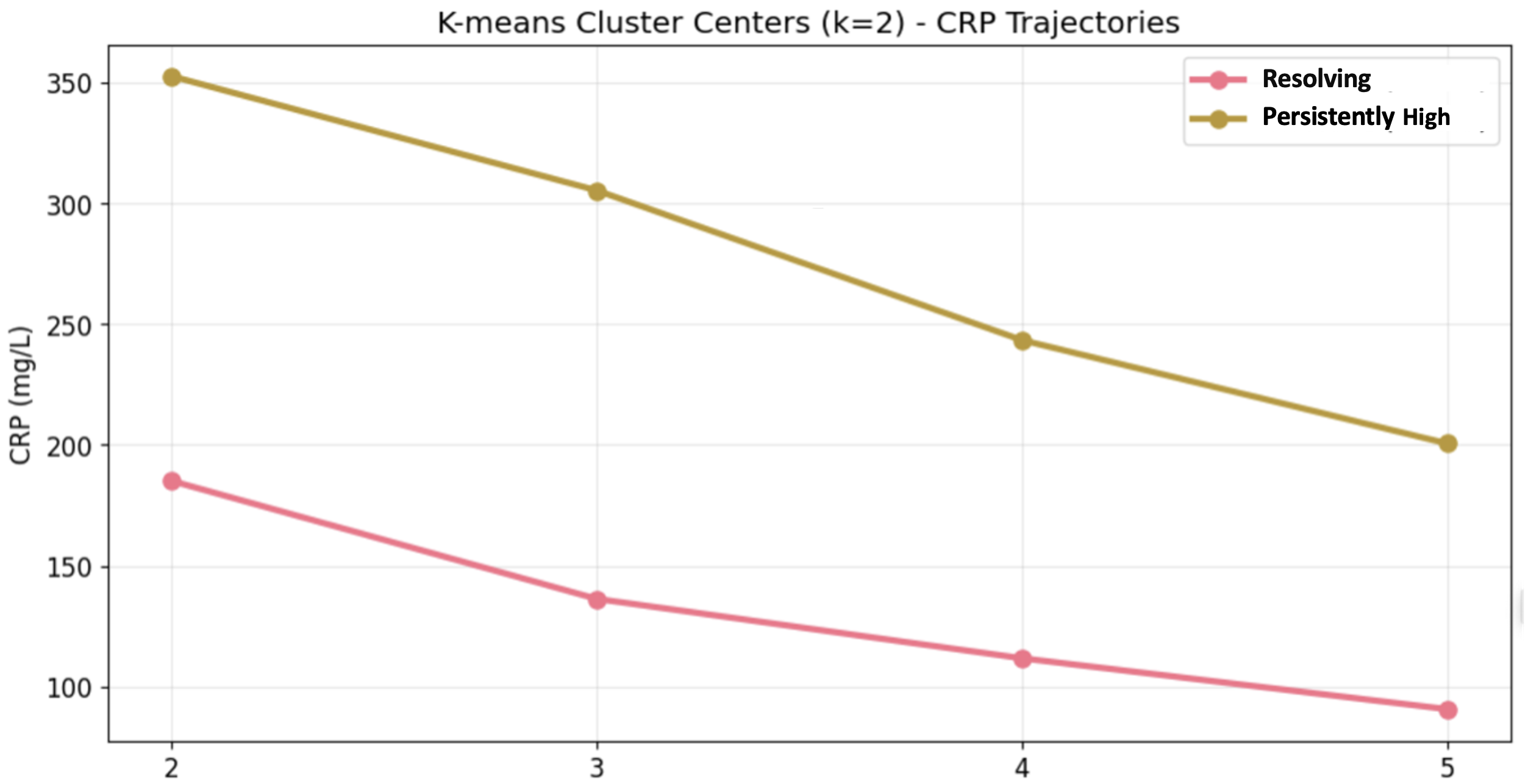
Figure: CRP trajectory clustering in acute pancreatitis identified two phenotypes: resolving and persistently elevated CRP.
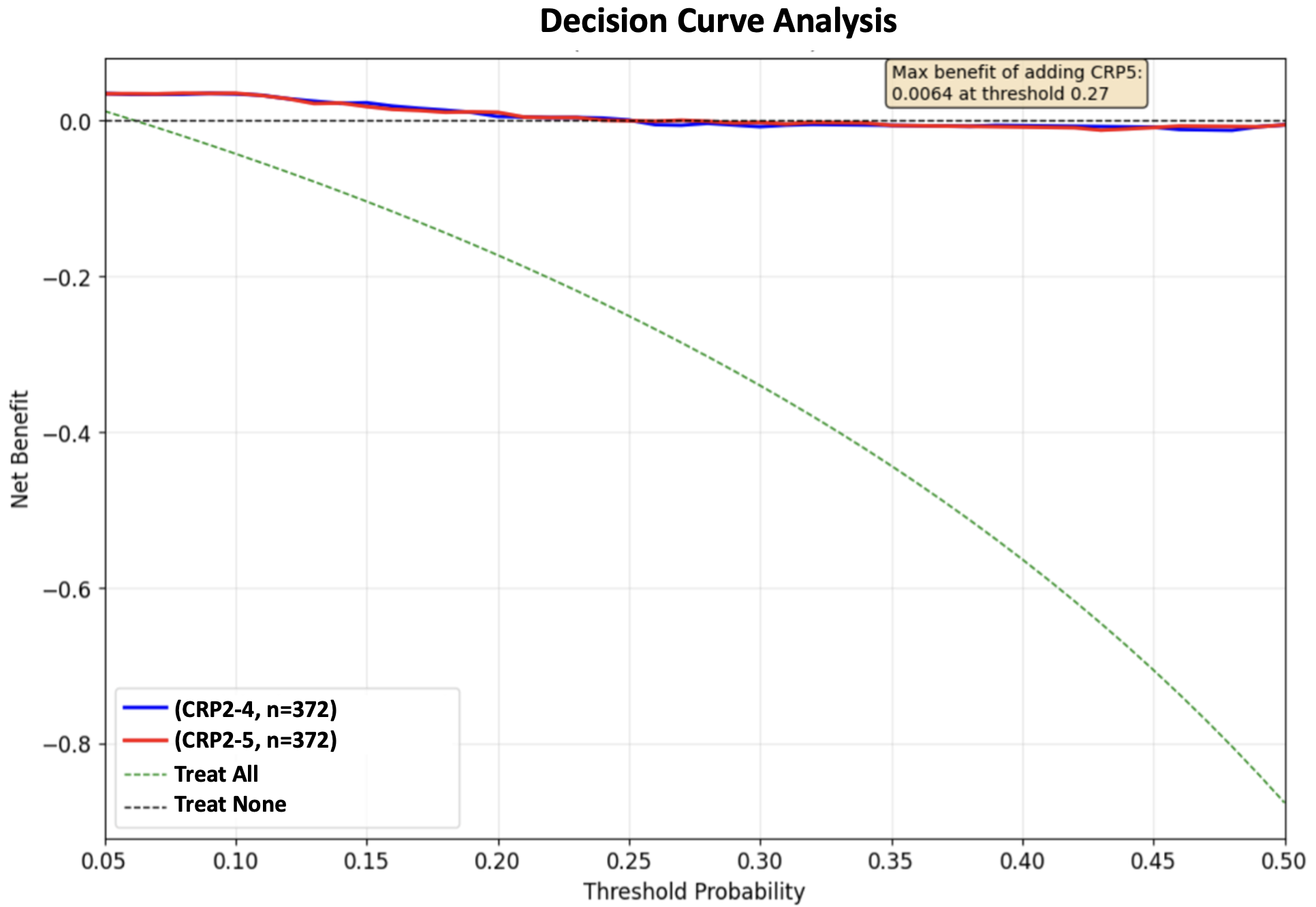
Figure: Decision curve analysis compared CRP2–4 vs CRP2–5 models to evaluate net clinical benefit from adding CRP Day 5.
Disclosures:
Samir Vanani indicated no relevant financial relationships.
Mipasha Patel indicated no relevant financial relationships.
Dhvani Adhvaryu indicated no relevant financial relationships.
Nishtha Nandwani indicated no relevant financial relationships.
Aarya Desai indicated no relevant financial relationships.
Dhiraaj Desai indicated no relevant financial relationships.
Rajiv Mehta indicated no relevant financial relationships.
Samir Vanani, MBBS1, Mipasha Patel, MD2, Dhvani Adhvaryu, PharmD1, Nishtha Nandwani, MBBS1, Aarya Desai, BSc1, Dhiraaj Desai, BE1, Rajiv Mehta, MD, DNB1. P0016 - Early CRP Trends and Phenotypes Predict Mortality in Acute Pancreatitis: A Trajectory-Based Analysis With Implications for Resource Optimization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Samir Vanani, MBBS1, Mipasha Patel, MD2, Dhvani Adhvaryu, PharmD1, Nishtha Nandwani, MBBS1, Aarya Desai, BSc1, Dhiraaj Desai, BE1, Rajiv Mehta, MD, DNB1
1Surat Institute of Digestive Sciences Hospital, Surat, Gujarat, India; 2Jefferson Abington Hospital, Willow Grove, PA
Introduction: C-reactive protein (CRP) is commonly used in acute pancreatitis (AP) to assess severity, but the value of early serial CRP trends for mortality prediction is unclear. We evaluated whether changes over the first 4-5 days can improve risk stratification and guide clinical decision-making.
Methods: We ambispectively analyzed 372 AP patients (median age: 39 [IQR 30-54]; 80% male) with serial CRP values recorded from days 2 to 5 of symptom onset (CRP2-CRP5). Missing values were imputed using constrained interpolation or iterative regression. Post-imputation analyses showed consistent trends and predictive performance compared to complete-case data. K-means clustering identified CRP trajectory phenotypes. Logistic regression, ROC analysis, and decision curve analysis (DCA) assessed mortality prediction and net clinical benefit. Subgroup analysis was performed by CRP2 level and BISAP score.
Results: Overall mortality was 6.2% (n=23). Mean CRP declined from 250 mg/L (day 2) to 134 mg/L (day 5). Trajectory clustering revealed two phenotypes, resolving CRP (mortality 2.2%) and persistently elevated CRP (mortality 12.4%; OR=6.29). A model using CRP2-CRP4 yielded strong discrimination for mortality (AUC=0.809; 95% CI: 0.689–0.911). Overall, a CRP4/CRP2 ratio ≥0.90 predicted mortality with AUC of 0.64. In patients with CRP2 >300 mg/L (n=134), predictive performance improved (AUC = 0.820, NPV = 93.9%), highlighting its utility in high-baseline inflammation states. Predictive trends remained consistent across etiologies and robust across sensitivity analyses. Decision curve analysis showed that adding CRP5 to the model of CRP2-4 provided minimal incremental benefit (AUC gain of +0.002)), with a maximum net benefit of 0.0064 at a threshold probability of 0.27, suggesting most prognostic information is captured by Day 4. Early CRP trends can inform ICU triage, escalation of care, and early discharge planning, supporting more efficient resource allocation.
Discussion: CRP trajectories through Day 4 define meaningful phenotypes in AP. The CRP4/CRP2 ratio provides modest overall discrimination but is highly predictive in patients with elevated baseline CRP. The limited added value of day 5 CRP supports more efficient care pathways, especially in settings with constrained resources. Early CRP trends offer a practical, scalable tool for personalized and resource-conscious AP care.
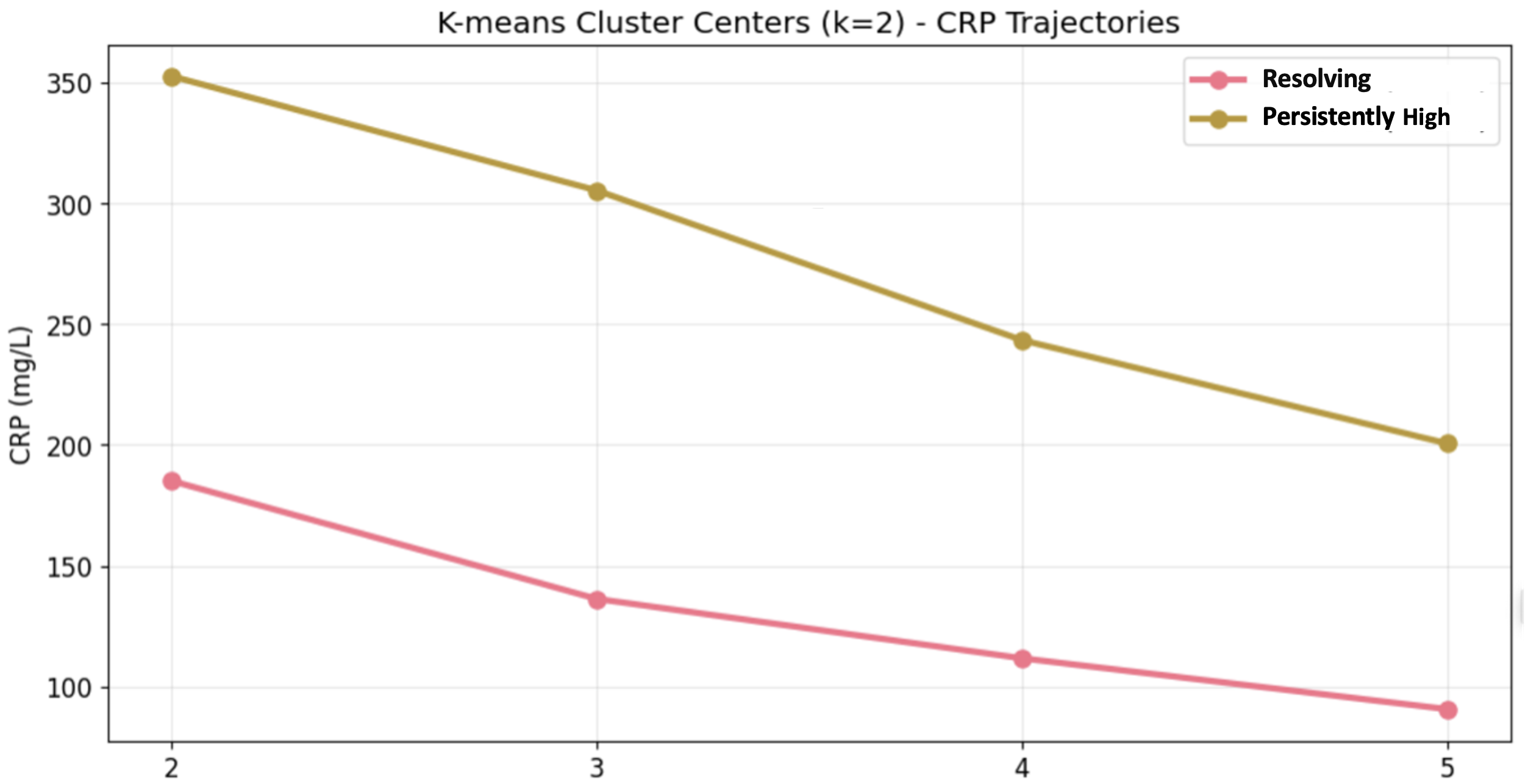
Figure: CRP trajectory clustering in acute pancreatitis identified two phenotypes: resolving and persistently elevated CRP.
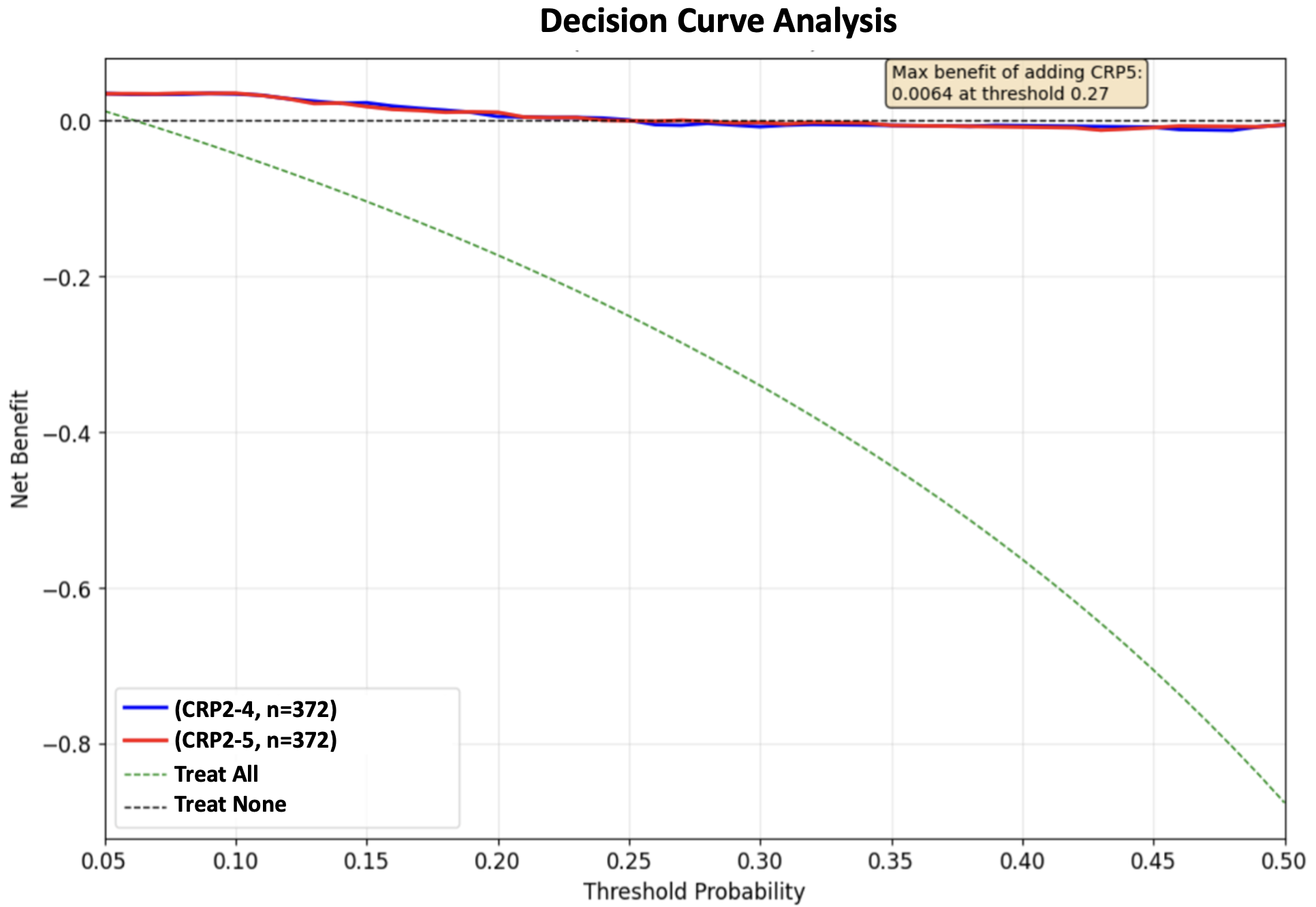
Figure: Decision curve analysis compared CRP2–4 vs CRP2–5 models to evaluate net clinical benefit from adding CRP Day 5.
Disclosures:
Samir Vanani indicated no relevant financial relationships.
Mipasha Patel indicated no relevant financial relationships.
Dhvani Adhvaryu indicated no relevant financial relationships.
Nishtha Nandwani indicated no relevant financial relationships.
Aarya Desai indicated no relevant financial relationships.
Dhiraaj Desai indicated no relevant financial relationships.
Rajiv Mehta indicated no relevant financial relationships.
Samir Vanani, MBBS1, Mipasha Patel, MD2, Dhvani Adhvaryu, PharmD1, Nishtha Nandwani, MBBS1, Aarya Desai, BSc1, Dhiraaj Desai, BE1, Rajiv Mehta, MD, DNB1. P0016 - Early CRP Trends and Phenotypes Predict Mortality in Acute Pancreatitis: A Trajectory-Based Analysis With Implications for Resource Optimization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


