Sunday Poster Session
Category: Biliary/Pancreas
P0015 - The Diagnostic Accuracy of Neutrophil-to-Lymphocyte Ratio (NLR) for Assessing Severity of Acute Cholecystitis in the Preoperative Period: A Bayesian Latent Class Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SK
Syeda Kanza Kazmi, MD (she/her/hers)
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Syeda Kanza Kazmi, MD1, Muhammad Zain Raza, MBBS2, Hafiz Muhammad Ehsan Arshad, MBBS2, Musab Maqsood, MBBS2, Ali Ahmad Nadeem, MBBS2, Muhammad Omais, MBBS2
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2King Edward Medical University, Lahore, Punjab, Pakistan
Introduction: Severe acute cholecystitis (AC) carries high risks of morbidity and mortality, yet no universally agreed upon standard method to assess its severity at admission especially in low-resource emergency settings. The neutrophil-to-lymphocyte ratio (NLR), a simple and inexpensive blood marker, reflects the intensity of inflammation and may indicate complications like gangrene or organ dysfunction. Its low cost and quick turnaround make NLR a practical tool for early triage. This meta-analysis aimed to evaluate the diagnostic accuracy of NLR in predicting severe cholecystitis.
Methods: Five databases were searched to identify relevant studies. Given the lack of a uniform reference standard, a Bayesian latent class meta-analysis (B-LCMA) model was employed which estimates sensitivity and specificity without assuming a perfect gold standard and accounts for uncertainty in the true disease status. Optimal threshold for NLR was determined using a hierarchical summary receiver operating characteristic (HSROC) model.
Results: A total of 27 studies met the inclusion criteria. Three reference standards were considered i.e., Tokyo guidelines, histopathology, and presence of organ complications. B-LCMA produced posterior median estimates for sensitivity of 74.7 (95% CrI: 67.1–83.6) and specificity of 76.8 (95% CrI: 71.2–82.6), indicating moderate to high diagnostic performance across diverse thresholds and reference standards. The subgroup analysis based on reference standard revealed similar results in all subgroups (Table 1, Figure 1B). The cut-point parameter (0.392; 95% CrI: -0.291–4.267) and accuracy parameter (2.55; 95% CrI: 1.869–8.837) suggested substantial between-study variability in the NLR thresholds used. The optimal NLR threshold determined via HSROC model was 9.250, yielding a sensitivity of 72.2% (95% CI: 56.3–84.0) and specificity of 70.3% (95% CI: 59.4–79.3).
Discussion: NLR showed moderate diagnostic performance in predicting severe acute cholecystitis; however, significant between-study heterogeneity reduces the certainty of the evidence. While further high-quality studies are needed to confirm its clinical utility, given its moderate effectiveness, NLR may still be valuable as part of a broader diagnostic algorithm, alongside markers like CRP and ultrasonography, for effective preoperative triage.
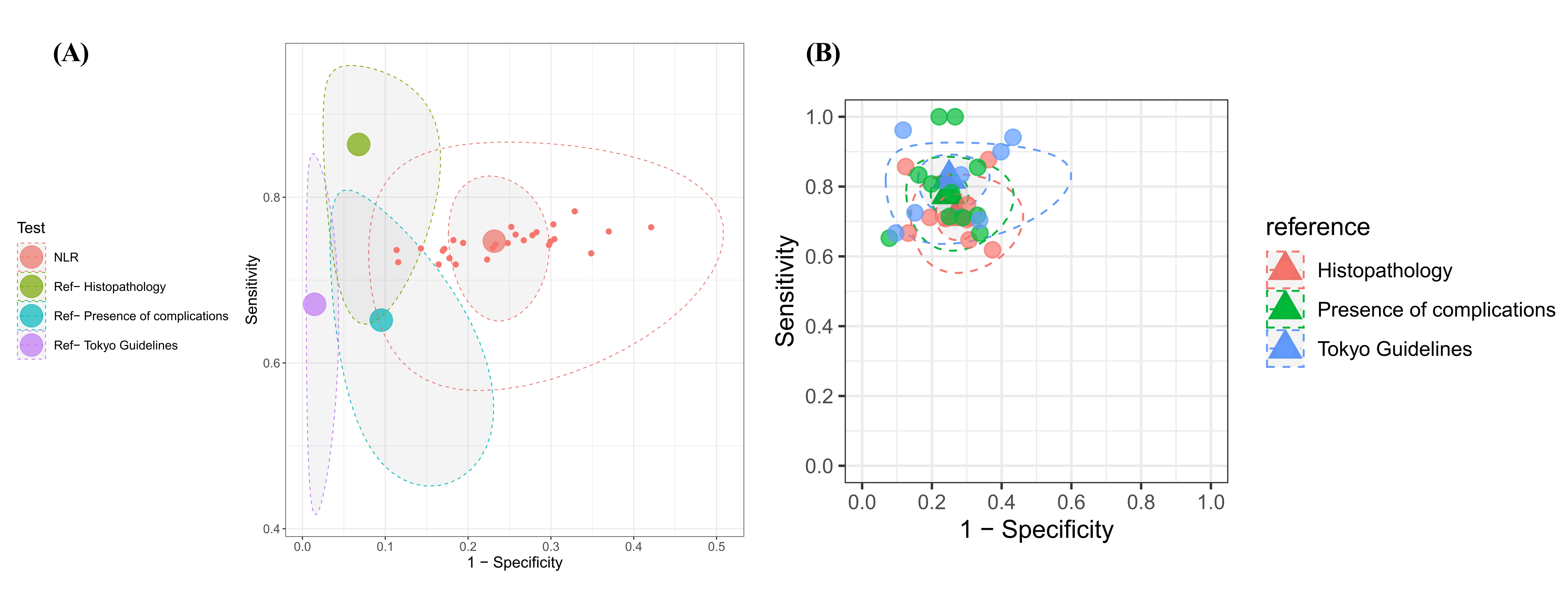
Figure: Table 1: The parameter estimates from B-LCMA model for NLR and reference standards as well as subgroup analysis based on reference standards
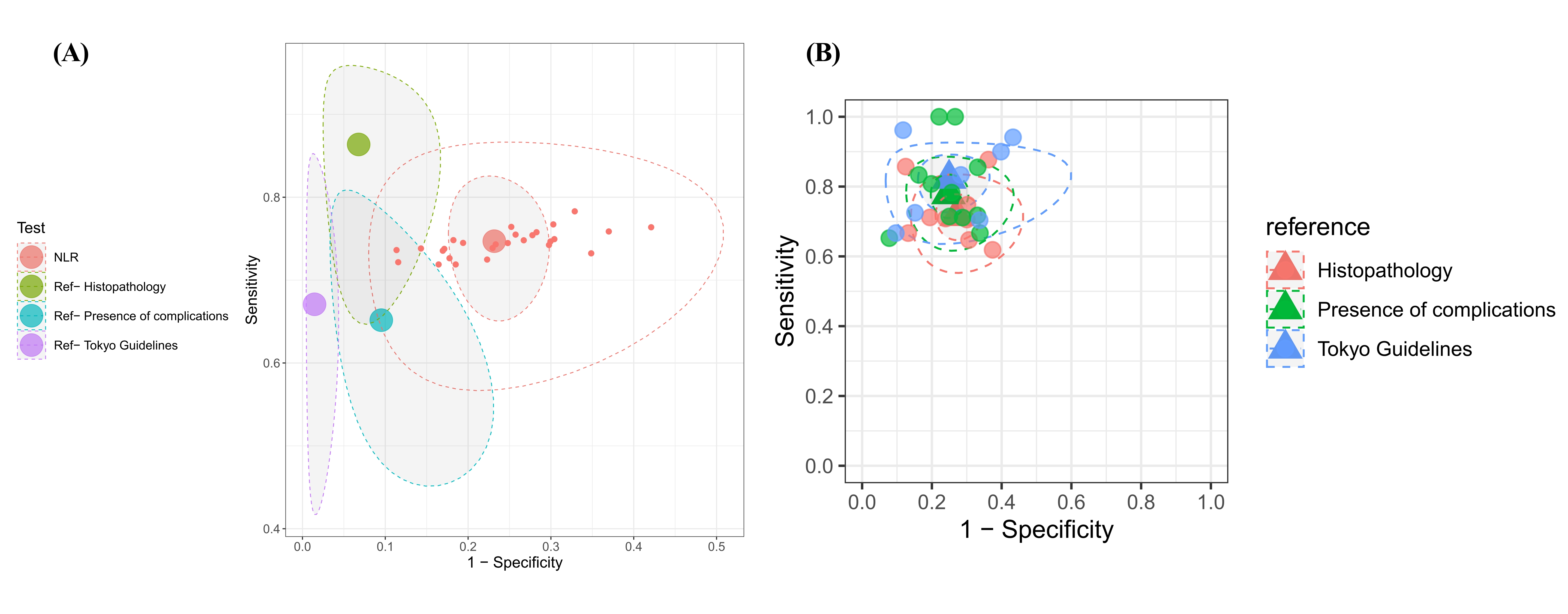
Figure: Figure 1: (A) SROC based on B-LCMA model. (B) SROC for subgroup analysis
Disclosures:
Syeda Kanza Kazmi indicated no relevant financial relationships.
Muhammad Zain Raza indicated no relevant financial relationships.
Hafiz Muhammad Ehsan Arshad indicated no relevant financial relationships.
Musab Maqsood indicated no relevant financial relationships.
Ali Ahmad Nadeem indicated no relevant financial relationships.
Muhammad Omais indicated no relevant financial relationships.
Syeda Kanza Kazmi, MD1, Muhammad Zain Raza, MBBS2, Hafiz Muhammad Ehsan Arshad, MBBS2, Musab Maqsood, MBBS2, Ali Ahmad Nadeem, MBBS2, Muhammad Omais, MBBS2. P0015 - The Diagnostic Accuracy of Neutrophil-to-Lymphocyte Ratio (NLR) for Assessing Severity of Acute Cholecystitis in the Preoperative Period: A Bayesian Latent Class Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2King Edward Medical University, Lahore, Punjab, Pakistan
Introduction: Severe acute cholecystitis (AC) carries high risks of morbidity and mortality, yet no universally agreed upon standard method to assess its severity at admission especially in low-resource emergency settings. The neutrophil-to-lymphocyte ratio (NLR), a simple and inexpensive blood marker, reflects the intensity of inflammation and may indicate complications like gangrene or organ dysfunction. Its low cost and quick turnaround make NLR a practical tool for early triage. This meta-analysis aimed to evaluate the diagnostic accuracy of NLR in predicting severe cholecystitis.
Methods: Five databases were searched to identify relevant studies. Given the lack of a uniform reference standard, a Bayesian latent class meta-analysis (B-LCMA) model was employed which estimates sensitivity and specificity without assuming a perfect gold standard and accounts for uncertainty in the true disease status. Optimal threshold for NLR was determined using a hierarchical summary receiver operating characteristic (HSROC) model.
Results: A total of 27 studies met the inclusion criteria. Three reference standards were considered i.e., Tokyo guidelines, histopathology, and presence of organ complications. B-LCMA produced posterior median estimates for sensitivity of 74.7 (95% CrI: 67.1–83.6) and specificity of 76.8 (95% CrI: 71.2–82.6), indicating moderate to high diagnostic performance across diverse thresholds and reference standards. The subgroup analysis based on reference standard revealed similar results in all subgroups (Table 1, Figure 1B). The cut-point parameter (0.392; 95% CrI: -0.291–4.267) and accuracy parameter (2.55; 95% CrI: 1.869–8.837) suggested substantial between-study variability in the NLR thresholds used. The optimal NLR threshold determined via HSROC model was 9.250, yielding a sensitivity of 72.2% (95% CI: 56.3–84.0) and specificity of 70.3% (95% CI: 59.4–79.3).
Discussion: NLR showed moderate diagnostic performance in predicting severe acute cholecystitis; however, significant between-study heterogeneity reduces the certainty of the evidence. While further high-quality studies are needed to confirm its clinical utility, given its moderate effectiveness, NLR may still be valuable as part of a broader diagnostic algorithm, alongside markers like CRP and ultrasonography, for effective preoperative triage.
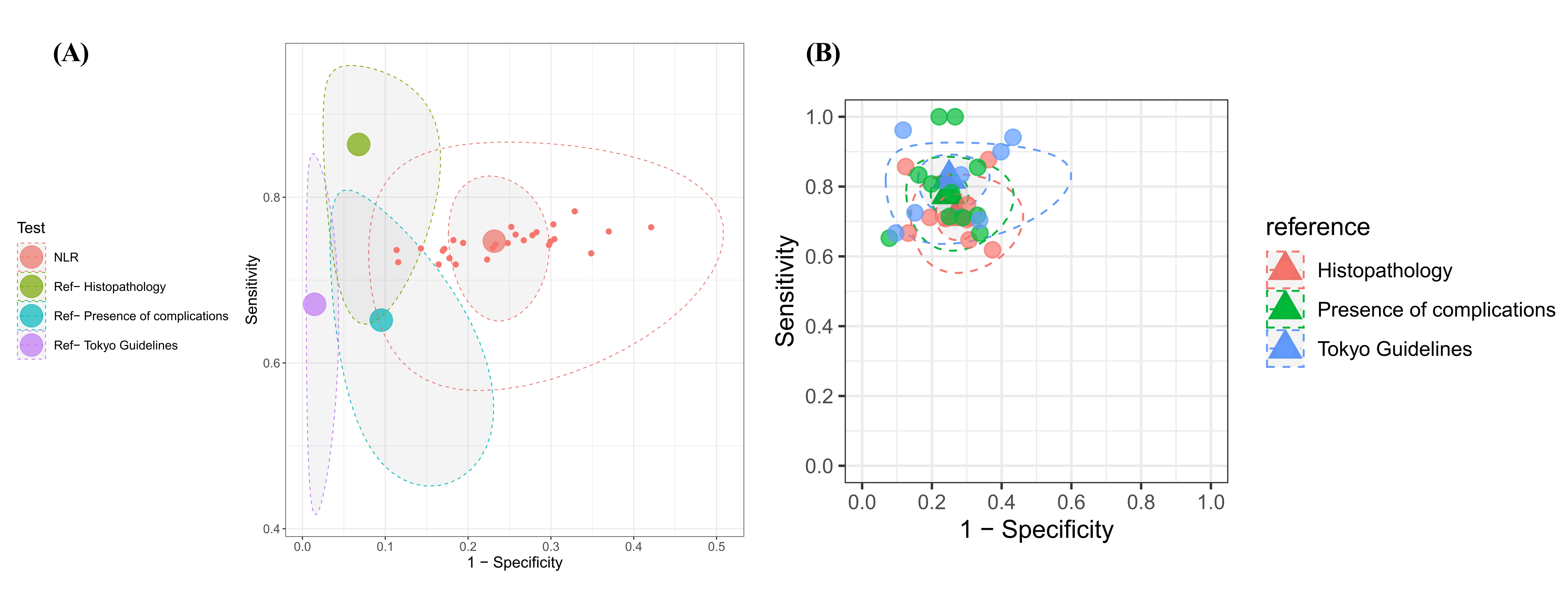
Figure: Table 1: The parameter estimates from B-LCMA model for NLR and reference standards as well as subgroup analysis based on reference standards
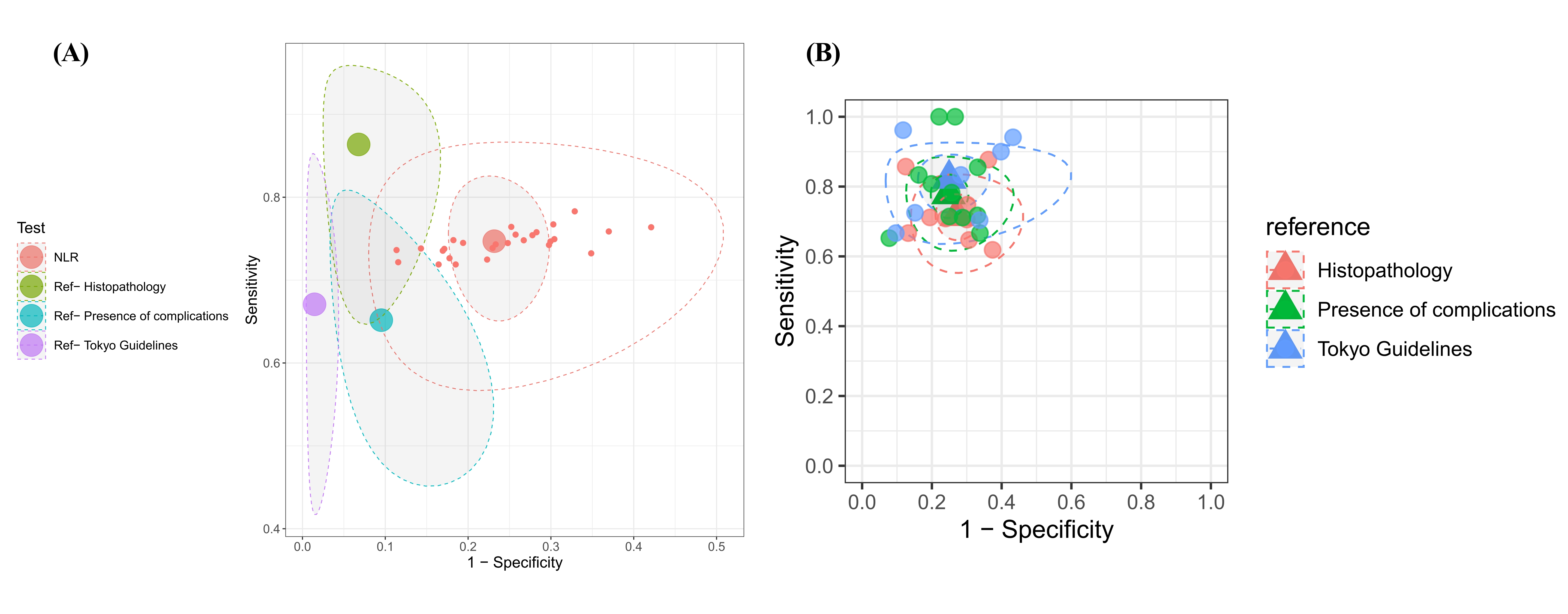
Figure: Figure 1: (A) SROC based on B-LCMA model. (B) SROC for subgroup analysis
Disclosures:
Syeda Kanza Kazmi indicated no relevant financial relationships.
Muhammad Zain Raza indicated no relevant financial relationships.
Hafiz Muhammad Ehsan Arshad indicated no relevant financial relationships.
Musab Maqsood indicated no relevant financial relationships.
Ali Ahmad Nadeem indicated no relevant financial relationships.
Muhammad Omais indicated no relevant financial relationships.
Syeda Kanza Kazmi, MD1, Muhammad Zain Raza, MBBS2, Hafiz Muhammad Ehsan Arshad, MBBS2, Musab Maqsood, MBBS2, Ali Ahmad Nadeem, MBBS2, Muhammad Omais, MBBS2. P0015 - The Diagnostic Accuracy of Neutrophil-to-Lymphocyte Ratio (NLR) for Assessing Severity of Acute Cholecystitis in the Preoperative Period: A Bayesian Latent Class Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

