Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 1B: Pancreas
17 - Evaluating the Cost of Surveillance in Pancreatic Cysts of Low-Risk Features in Patients Over 70-Years-Old
Monday, October 27, 2025
2:35 PM - 2:45 PM PDT
Location: North Ballroom 120BC

Shaina Ailawadi, MD
Case Western Reserve University/University Hospitals
University Heights, OH
Presenting Author(s)
Shaina Ailawadi, MD1, Abbinaya Elangovan, MD2, Apoorva K. Chandar, MBBS, MPH3, Mart Andrew Maravillas, MS4, Andrew Catanzaro, MD3, Amitabh Chak, MD, FACG5
1Case Western Reserve University/University Hospitals, University Heights, OH; 2Carilion Clinic, Roanoke, VA; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 5University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: The increasing utilization of high-resolution cross-sectional imaging has led to more incidental diagnoses of pancreatic cysts, particularly in elderly patients. With up to three million incidental pancreatic cystic lesions (PCL) diagnosed each year in the United States, there remains a question about the utility and cost associated with surveillance of PCL of low-risk features (LRF) in elderly patients. In our study, we evaluated the cost of current management guidelines of PCLs of LRF in patients over age 70 from a single tertiary-referral center.
Methods: A retrospective chart review was performed at our tertiary care referral center from 2012-2024 on patients 70-years or older who had a new PCL of LRF diagnosed by CT/MRI. Patients with low-risk PCLs as defined by Fukuoka Criteria were identified via radiographic imaging reports. This cohort was divided into two groups: the no-surveillance group (NSG) (n=184) with no further imaging after identification of PCL, and the surveillance group (SG) (n=256) with patients who had one or more CT/MRI after the diagnosis of PCL. The average cost of radiographic scans from our healthcare system was used to estimate the cost per scan. A descriptive statistics model was used to determine the total cost of surveillance.
Results: Of the 440 patients identified with PCL of LRF, the SG consisted of 256 patients and NSG comprised of 184 patients. The mean age of the cohort was 79.8 ± 12.1 years. The patients were predominantly white (85.0%) and female (67.1%). Throughout the study period, no patients in either cohort developed pancreatic cancer. The survival time in patient years was 7.04 + 3.79 for the surveillance group and 5.26 + 4.03 for the non-surveillance group. The mean number of scans for the surveillance group was 4.72 + 2.75. The average cost of surveillance in this population was $17,628 per person. The total cost of surveillance in our study was $4,512,813 and over the 13-year study period, $347,139 is projected to be spent on surveillance per year (Figure 1).
Discussion: With the widespread use of radiographic imaging in our healthcare system, an increasing number of PCLs with LRF are being diagnosed in elderly patients. With neither the SG nor the NSG group developing pancreatic cancer, the current management of PCL with LRF in patients newly diagnosed over age 70 is not cost-effective. Re-evaluation of surveillance guidelines and consideration of surveillance cessation in this population may reduce unnecessary healthcare expenditures.
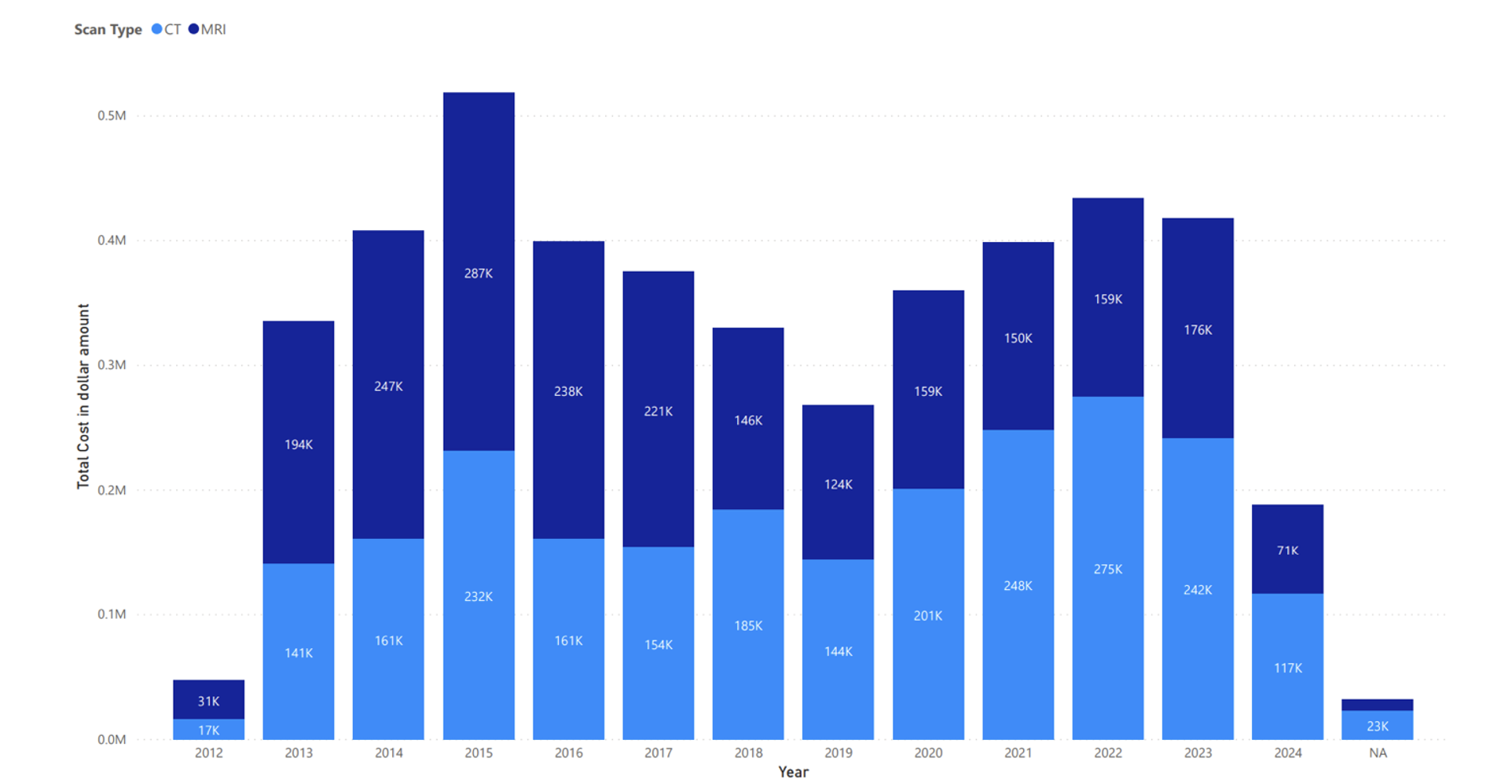
Figure: Figure 1. Total cost of CT and MRI scans for pancreatic cystic lesions of low-risk features surveillance in patients over age 70.
Disclosures:
Shaina Ailawadi indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Mart Andrew Maravillas indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Amitabh Chak: Lucid Dx – Consultant, Grant/Research Support, Intellectual Property/Patents, Royalties, Stock Options, Stock-publicly held company(excluding mutual/index funds). MicroTech – Consultant. Pentax – Consultant. Steris – Consultant.
Shaina Ailawadi, MD1, Abbinaya Elangovan, MD2, Apoorva K. Chandar, MBBS, MPH3, Mart Andrew Maravillas, MS4, Andrew Catanzaro, MD3, Amitabh Chak, MD, FACG5, 17, Evaluating the Cost of Surveillance in Pancreatic Cysts of Low-Risk Features in Patients Over 70-Years-Old, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University/University Hospitals, University Heights, OH; 2Carilion Clinic, Roanoke, VA; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 5University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: The increasing utilization of high-resolution cross-sectional imaging has led to more incidental diagnoses of pancreatic cysts, particularly in elderly patients. With up to three million incidental pancreatic cystic lesions (PCL) diagnosed each year in the United States, there remains a question about the utility and cost associated with surveillance of PCL of low-risk features (LRF) in elderly patients. In our study, we evaluated the cost of current management guidelines of PCLs of LRF in patients over age 70 from a single tertiary-referral center.
Methods: A retrospective chart review was performed at our tertiary care referral center from 2012-2024 on patients 70-years or older who had a new PCL of LRF diagnosed by CT/MRI. Patients with low-risk PCLs as defined by Fukuoka Criteria were identified via radiographic imaging reports. This cohort was divided into two groups: the no-surveillance group (NSG) (n=184) with no further imaging after identification of PCL, and the surveillance group (SG) (n=256) with patients who had one or more CT/MRI after the diagnosis of PCL. The average cost of radiographic scans from our healthcare system was used to estimate the cost per scan. A descriptive statistics model was used to determine the total cost of surveillance.
Results: Of the 440 patients identified with PCL of LRF, the SG consisted of 256 patients and NSG comprised of 184 patients. The mean age of the cohort was 79.8 ± 12.1 years. The patients were predominantly white (85.0%) and female (67.1%). Throughout the study period, no patients in either cohort developed pancreatic cancer. The survival time in patient years was 7.04 + 3.79 for the surveillance group and 5.26 + 4.03 for the non-surveillance group. The mean number of scans for the surveillance group was 4.72 + 2.75. The average cost of surveillance in this population was $17,628 per person. The total cost of surveillance in our study was $4,512,813 and over the 13-year study period, $347,139 is projected to be spent on surveillance per year (Figure 1).
Discussion: With the widespread use of radiographic imaging in our healthcare system, an increasing number of PCLs with LRF are being diagnosed in elderly patients. With neither the SG nor the NSG group developing pancreatic cancer, the current management of PCL with LRF in patients newly diagnosed over age 70 is not cost-effective. Re-evaluation of surveillance guidelines and consideration of surveillance cessation in this population may reduce unnecessary healthcare expenditures.
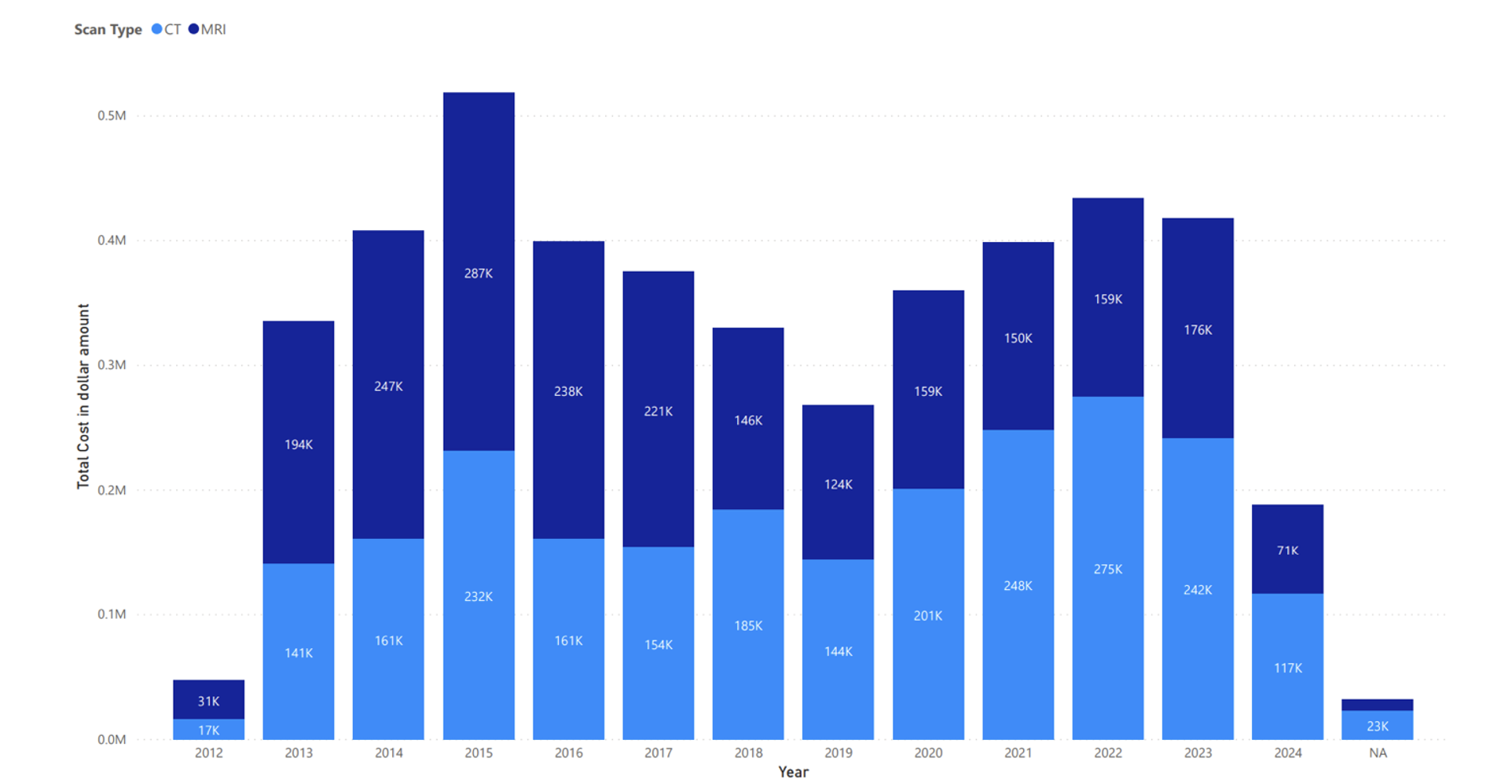
Figure: Figure 1. Total cost of CT and MRI scans for pancreatic cystic lesions of low-risk features surveillance in patients over age 70.
Disclosures:
Shaina Ailawadi indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Mart Andrew Maravillas indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Amitabh Chak: Lucid Dx – Consultant, Grant/Research Support, Intellectual Property/Patents, Royalties, Stock Options, Stock-publicly held company(excluding mutual/index funds). MicroTech – Consultant. Pentax – Consultant. Steris – Consultant.
Shaina Ailawadi, MD1, Abbinaya Elangovan, MD2, Apoorva K. Chandar, MBBS, MPH3, Mart Andrew Maravillas, MS4, Andrew Catanzaro, MD3, Amitabh Chak, MD, FACG5, 17, Evaluating the Cost of Surveillance in Pancreatic Cysts of Low-Risk Features in Patients Over 70-Years-Old, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

