Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 1A: Infection, Microbiome, Small Intestine
13 - Bile Acid Malabsorption Is Common in Celiac Disease, Especially After Cholecystectomy
Monday, October 27, 2025
2:35 PM - 2:45 PM PDT
Location: North Ballroom 120D

John Damianos, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Award: ACG Auxiliary Award (Trainee)
John Damianos, MD, Katherine S. King, MS, Alex Lee, BS, Michael Camilleri, MD, DSc, Joseph Murray, MD, FACG, Adam C. Bledsoe, MD
Mayo Clinic, Rochester, MN
Introduction: Up to 50% of patients with celiac disease (CD) have ongoing symptoms despite gluten-free diet. Since bile acid (BA) absorption requires intact distal ileal mucosa, our aim was to assess BA malabsorption (BAM) in patients with CD with chronic diarrhea, and with severity or refractoriness of CD, or associated GI disorders: microscopic colitis, small intestinal bacterial overgrowth (SIBO), cholecystectomy, and gastric and colonic transit.
Methods: Patients who had undergone testing for BAM were screened via ICD codes and CD was confirmed by characteristic serologic and histologic findings. BAM testing modalities included serum 7αC4 and single or 48-hour stool measurements of primary BAs (PBA ). Positive results were defined by any of the following: Serum 7αC4 >52.5 ng/mL; or combined single stool >10% PBA plus serum 7αC4 >52.5ng/mL; or either of these 48h stool results: >2337 μmol total BA, or >10% PBAs or combination >1000 μmol/48h plus >4% PBAs. Records were also reviewed for CD severity, associated GI disorders, and results of gastric and colonic transit by scintigraphy.
Results: A total of 363 patients with CD were tested for BAM (76.6% female, 96.1% white, median age at testing 48, range 10-89). Testing modalities included 46.4% 7αC4, 1.4% 7αC4 plus PBAs (in single stool), 0.8% total BAs in 48 hour stool ,20.9% stool PBAs, and 30.4% PBAs plus total BAs in 48 hour stool . BAM was identified in 35.3% of CD patients. Prevalence of BAM was not higher according to Marsh score, presence of refractory CD, microscopic colitis, or SIBO (Table 1). There was numerically faster colonic transit (GC24) between 8 patients with BAM (3.19 ± 0.34) and those 18 without BAM (2.53 ± 0.31) (p=0.11). Cholecystectomy was associated with a significantly higher prevalence of BAM in patients with CD (43% vs. 30% with no cholecystectomy, p = 0.019).
Discussion: BAM is present in 35.5% of patients with CD and is associated with more rapid colonic transit. Cholecystectomy is associated with BAM. These data are comparable with the prevalence of BAM in IBS-D/ functional diarrhea (29.3%) or cholecystectomy alone (45.8%) at the same center. CD disease severity, and comorbidities such as microscopic colitis and SIBO are not associated with BAM in CD. Evaluation for BAM should be considered in CD patients with persistent symptoms (especially diarrhea), particularly in those with a history of cholecystectomy.
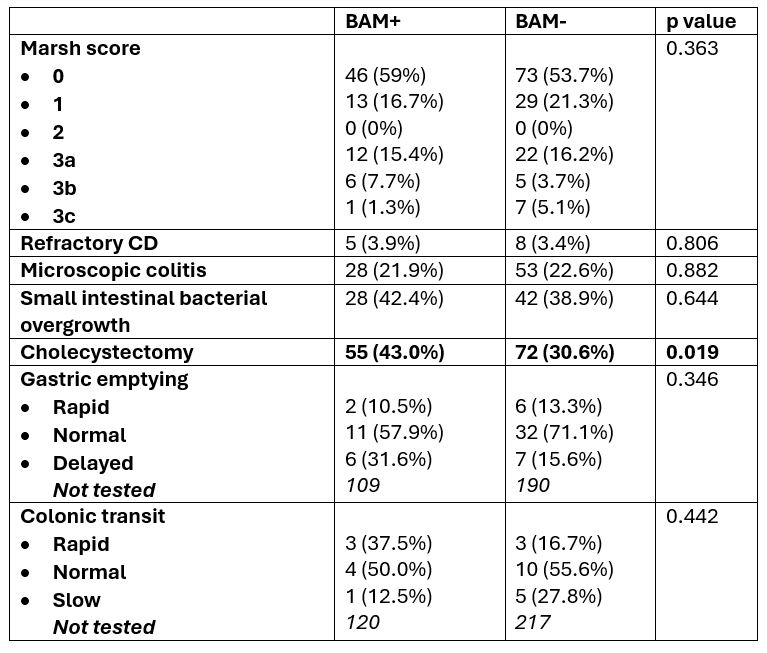
Figure: Table 1: Disease status and comorbidities of CD patients stratified by BAM.
Disclosures:
John Damianos: ExeGi Pharma – Consultant, Grant/Research Support. i-Health – Speakers Bureau.
Katherine King indicated no relevant financial relationships.
Alex Lee indicated no relevant financial relationships.
Michael Camilleri: Alfasigma – Consultant. Amylyx – Consultant. Biocodex – Grant/Research Support. BioKier – Consultant. Brightseed Bio – Consultant, Grant/Research Support. Coloplast – Consultant. Dignify Therapeutics – Stock Options. Intercept – Consultant. Invea – Consultant. Kallyope – Consultant. McDermott Will & Emery – Consultant. Medpace – Consultant. Monteresearch – Consultant. Neurogastrx – Consultant. NGM Biopharmaceuticals – Grant/Research Support. Pfizer – Grant/Research Support. Phenomix – Stock Options. Renexxion – Consultant. SKYE Bioscience – Consultant. Sumitomo – Consultant. Synlogic – Consultant. Vanda – Grant/Research Support.
Joseph Murray indicated no relevant financial relationships.
Adam Bledsoe: Anokion/Kanyos Bio – Grant/Research Support. Barinthus Bio – Grant/Research Support. Chugai Pharma – Grant/Research Support. Sanofi – Grant/Research Support. Takeda – Grant/Research Support.
John Damianos, MD, Katherine S. King, MS, Alex Lee, BS, Michael Camilleri, MD, DSc, Joseph Murray, MD, FACG, Adam C. Bledsoe, MD, 13, Bile Acid Malabsorption Is Common in Celiac Disease, Especially After Cholecystectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
John Damianos, MD, Katherine S. King, MS, Alex Lee, BS, Michael Camilleri, MD, DSc, Joseph Murray, MD, FACG, Adam C. Bledsoe, MD
Mayo Clinic, Rochester, MN
Introduction: Up to 50% of patients with celiac disease (CD) have ongoing symptoms despite gluten-free diet. Since bile acid (BA) absorption requires intact distal ileal mucosa, our aim was to assess BA malabsorption (BAM) in patients with CD with chronic diarrhea, and with severity or refractoriness of CD, or associated GI disorders: microscopic colitis, small intestinal bacterial overgrowth (SIBO), cholecystectomy, and gastric and colonic transit.
Methods: Patients who had undergone testing for BAM were screened via ICD codes and CD was confirmed by characteristic serologic and histologic findings. BAM testing modalities included serum 7αC4 and single or 48-hour stool measurements of primary BAs (PBA ). Positive results were defined by any of the following: Serum 7αC4 >52.5 ng/mL; or combined single stool >10% PBA plus serum 7αC4 >52.5ng/mL; or either of these 48h stool results: >2337 μmol total BA, or >10% PBAs or combination >1000 μmol/48h plus >4% PBAs. Records were also reviewed for CD severity, associated GI disorders, and results of gastric and colonic transit by scintigraphy.
Results: A total of 363 patients with CD were tested for BAM (76.6% female, 96.1% white, median age at testing 48, range 10-89). Testing modalities included 46.4% 7αC4, 1.4% 7αC4 plus PBAs (in single stool), 0.8% total BAs in 48 hour stool ,20.9% stool PBAs, and 30.4% PBAs plus total BAs in 48 hour stool . BAM was identified in 35.3% of CD patients. Prevalence of BAM was not higher according to Marsh score, presence of refractory CD, microscopic colitis, or SIBO (Table 1). There was numerically faster colonic transit (GC24) between 8 patients with BAM (3.19 ± 0.34) and those 18 without BAM (2.53 ± 0.31) (p=0.11). Cholecystectomy was associated with a significantly higher prevalence of BAM in patients with CD (43% vs. 30% with no cholecystectomy, p = 0.019).
Discussion: BAM is present in 35.5% of patients with CD and is associated with more rapid colonic transit. Cholecystectomy is associated with BAM. These data are comparable with the prevalence of BAM in IBS-D/ functional diarrhea (29.3%) or cholecystectomy alone (45.8%) at the same center. CD disease severity, and comorbidities such as microscopic colitis and SIBO are not associated with BAM in CD. Evaluation for BAM should be considered in CD patients with persistent symptoms (especially diarrhea), particularly in those with a history of cholecystectomy.
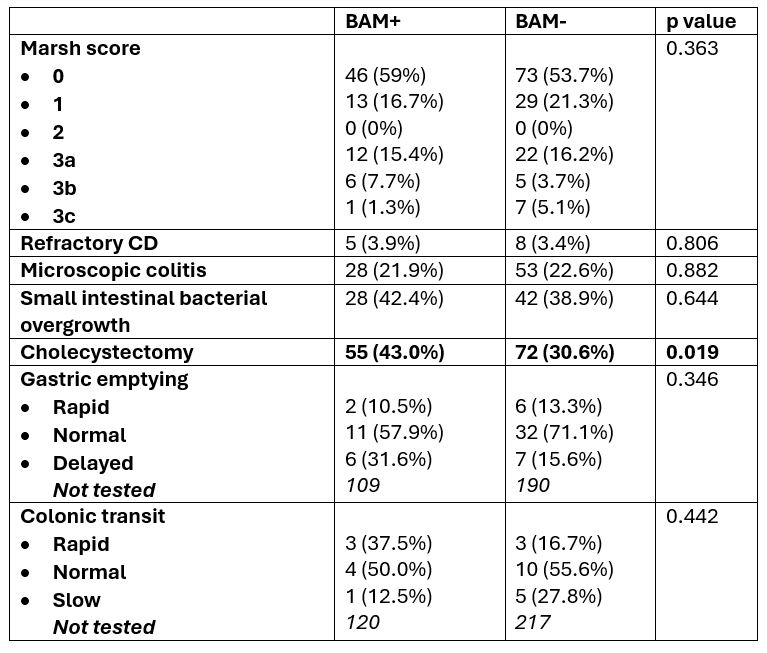
Figure: Table 1: Disease status and comorbidities of CD patients stratified by BAM.
Disclosures:
John Damianos: ExeGi Pharma – Consultant, Grant/Research Support. i-Health – Speakers Bureau.
Katherine King indicated no relevant financial relationships.
Alex Lee indicated no relevant financial relationships.
Michael Camilleri: Alfasigma – Consultant. Amylyx – Consultant. Biocodex – Grant/Research Support. BioKier – Consultant. Brightseed Bio – Consultant, Grant/Research Support. Coloplast – Consultant. Dignify Therapeutics – Stock Options. Intercept – Consultant. Invea – Consultant. Kallyope – Consultant. McDermott Will & Emery – Consultant. Medpace – Consultant. Monteresearch – Consultant. Neurogastrx – Consultant. NGM Biopharmaceuticals – Grant/Research Support. Pfizer – Grant/Research Support. Phenomix – Stock Options. Renexxion – Consultant. SKYE Bioscience – Consultant. Sumitomo – Consultant. Synlogic – Consultant. Vanda – Grant/Research Support.
Joseph Murray indicated no relevant financial relationships.
Adam Bledsoe: Anokion/Kanyos Bio – Grant/Research Support. Barinthus Bio – Grant/Research Support. Chugai Pharma – Grant/Research Support. Sanofi – Grant/Research Support. Takeda – Grant/Research Support.
John Damianos, MD, Katherine S. King, MS, Alex Lee, BS, Michael Camilleri, MD, DSc, Joseph Murray, MD, FACG, Adam C. Bledsoe, MD, 13, Bile Acid Malabsorption Is Common in Celiac Disease, Especially After Cholecystectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.



