Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 1A: Infection, Microbiome, Small Intestine
12 - Reducing Inappropriate Proton Pump Inhibitor Prescribing in Non-Critically Ill Hospitalized Patients: A Single Center Quality Improvement Project
Monday, October 27, 2025
2:25 PM - 2:35 PM PDT
Location: North Ballroom 120D

Matthew Ryan, MD
University of Miami
Miami, FL
Presenting Author(s)
Award: ACG Lawlor Resident Award
Matthew Ryan, MD1, Christopher Ma, MD2, Ami Panara Shukla, MD2, Marlene Onaindia, PharmD2, Sebastian Suarez, MD, MPH2
1University of Miami, Miami, FL; 2University of Miami Health System, Miami, FL
Introduction: Proton pump inhibitors (PPIs) are indicated for various gastrointestinal illnesses. However, they are sometimes inappropriately prescribed in non-critical hospitalized patients without a guideline-directed indication. PPI use is associated with Clostridium difficile (C. diff) infection, among other side effects. PPIs also pose a significant global economic burden, with market estimates of $3.52 billion by 2028. Current stewardship guidelines outside the intensive care unit are institution-specific, highlighting the need for standardized criteria to optimize prescribing practices. We conducted a quality improvement study to reduce inappropriate PPI prescribing on admission for patients admitted to internal medicine teams at a tertiary care center by 20% within 6 months using two de-implementation strategies.
Methods: Clinical data on inpatient PPI orders and ICD-10 codes billed for each admission to hospital medicine were extracted from the electronic medical record (EMR) via an information technology data pull and reviewed by a physician. Patients with ICD-10 codes for conditions where PPIs were indicated were excluded. Pre-intervention data (5/1/23-4/30/24) established baseline rates of inappropriate PPI orders. PPIs were removed from the EMR admission order set as the first intervention (5/1/24-7/30/24) and a standardized history and physical (H&P) note template was introduced to all medicine teams as the second intervention (7/31/24-12/31/24).
Results: The rate of inappropriate PPI orders on admission decreased from 42.4% to 34.1% (19.6% reduction, p< 0.001) between the pre-intervention (n=6549) and the post-intervention group (n=1683) (Figure 1A). When stratified by teams, PPI orders decreased by 40.8% (p< 0.001) in non-academic teams between the pre- and post-intervention groups (Figure 1B). C diff (defined by ICD-10 codes) decreased by 42.4% (p=0.037) in the same groups (Figure 2). There was no difference in PPI prescriptions at discharge between groups (p=0.228) (Figure 1A).
Discussion: Removing PPIs from the admission order sets and standardizing our H&P templates significantly reduced inappropriate PPI prescribing by 19.6%, primarily driven by changes in non-academic teams. Although C. diff infections decreased by 42.4%, we cannot conclude that this was solely due to our interventions. Limitations include reliance on ICD-10 codes and inaccurate home medication lists. Additional de-implementation strategies could decrease PPI orders during hospitalization and at discharge.
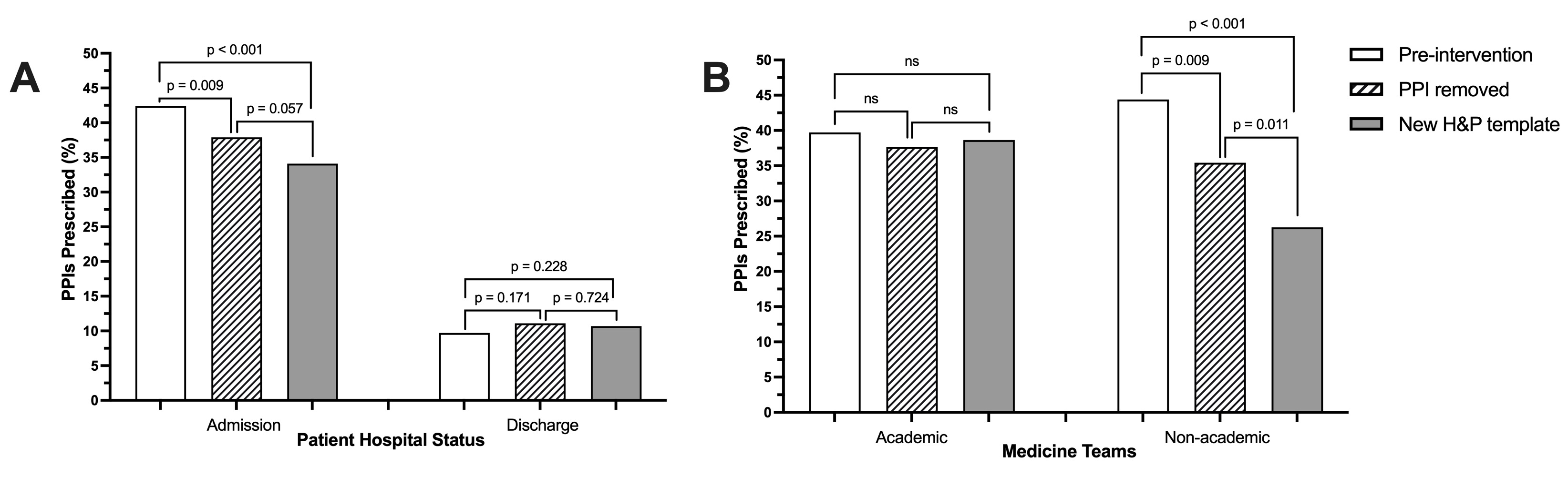
Figure: Figure 1. Rates of PPI orders on admission in (A) all non-critically ill admitted patients and in (B) patients stratified by academic vs non-academic teams.
Note: ns: non-significant
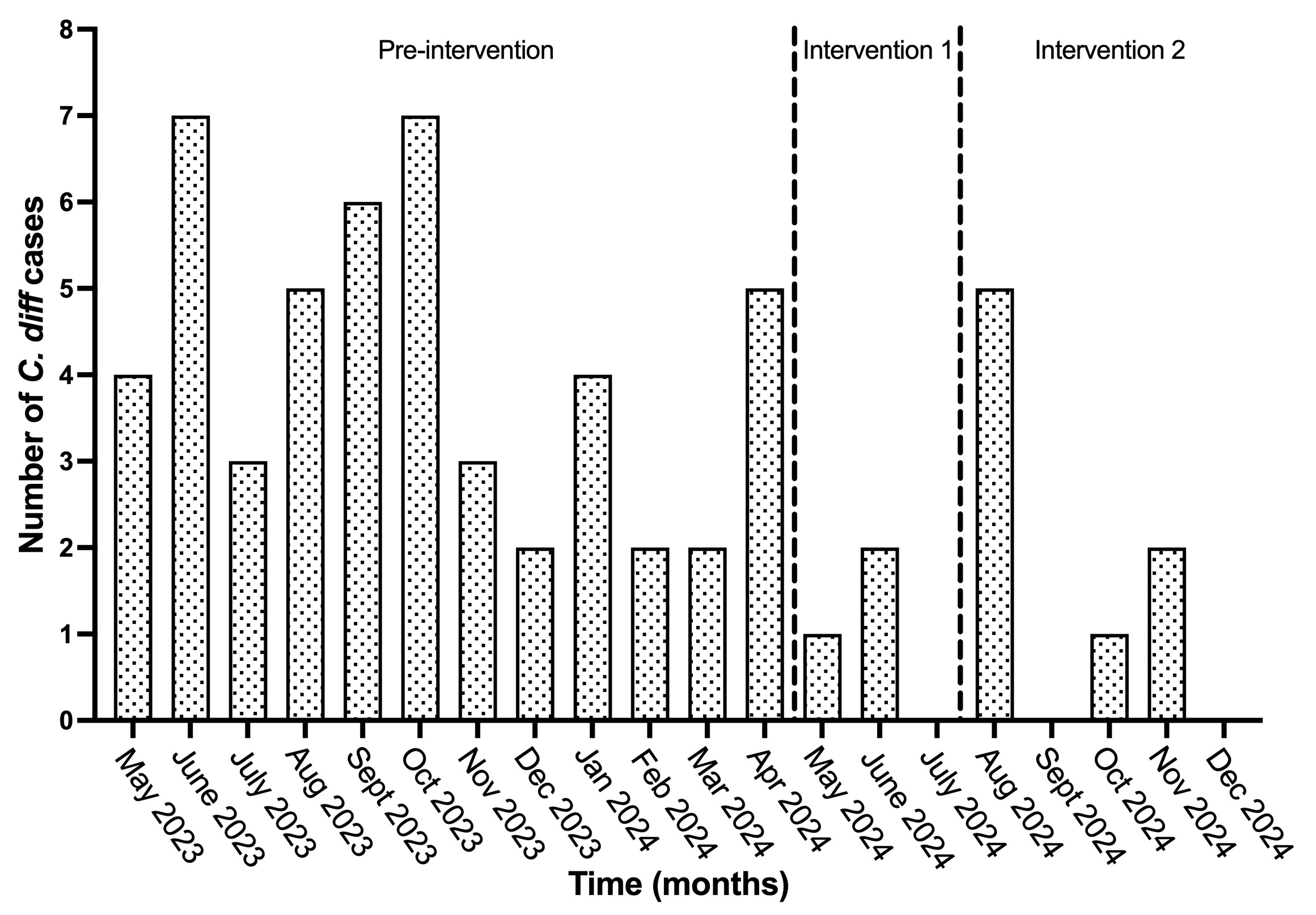
Figure: Figure 2. Number of C. diff infections throughout the study periods
Disclosures:
Matthew Ryan indicated no relevant financial relationships.
Christopher Ma indicated no relevant financial relationships.
Ami Panara Shukla indicated no relevant financial relationships.
Marlene Onaindia indicated no relevant financial relationships.
Sebastian Suarez indicated no relevant financial relationships.
Matthew Ryan, MD1, Christopher Ma, MD2, Ami Panara Shukla, MD2, Marlene Onaindia, PharmD2, Sebastian Suarez, MD, MPH2, 12, Reducing Inappropriate Proton Pump Inhibitor Prescribing in Non-Critically Ill Hospitalized Patients: A Single Center Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Matthew Ryan, MD1, Christopher Ma, MD2, Ami Panara Shukla, MD2, Marlene Onaindia, PharmD2, Sebastian Suarez, MD, MPH2
1University of Miami, Miami, FL; 2University of Miami Health System, Miami, FL
Introduction: Proton pump inhibitors (PPIs) are indicated for various gastrointestinal illnesses. However, they are sometimes inappropriately prescribed in non-critical hospitalized patients without a guideline-directed indication. PPI use is associated with Clostridium difficile (C. diff) infection, among other side effects. PPIs also pose a significant global economic burden, with market estimates of $3.52 billion by 2028. Current stewardship guidelines outside the intensive care unit are institution-specific, highlighting the need for standardized criteria to optimize prescribing practices. We conducted a quality improvement study to reduce inappropriate PPI prescribing on admission for patients admitted to internal medicine teams at a tertiary care center by 20% within 6 months using two de-implementation strategies.
Methods: Clinical data on inpatient PPI orders and ICD-10 codes billed for each admission to hospital medicine were extracted from the electronic medical record (EMR) via an information technology data pull and reviewed by a physician. Patients with ICD-10 codes for conditions where PPIs were indicated were excluded. Pre-intervention data (5/1/23-4/30/24) established baseline rates of inappropriate PPI orders. PPIs were removed from the EMR admission order set as the first intervention (5/1/24-7/30/24) and a standardized history and physical (H&P) note template was introduced to all medicine teams as the second intervention (7/31/24-12/31/24).
Results: The rate of inappropriate PPI orders on admission decreased from 42.4% to 34.1% (19.6% reduction, p< 0.001) between the pre-intervention (n=6549) and the post-intervention group (n=1683) (Figure 1A). When stratified by teams, PPI orders decreased by 40.8% (p< 0.001) in non-academic teams between the pre- and post-intervention groups (Figure 1B). C diff (defined by ICD-10 codes) decreased by 42.4% (p=0.037) in the same groups (Figure 2). There was no difference in PPI prescriptions at discharge between groups (p=0.228) (Figure 1A).
Discussion: Removing PPIs from the admission order sets and standardizing our H&P templates significantly reduced inappropriate PPI prescribing by 19.6%, primarily driven by changes in non-academic teams. Although C. diff infections decreased by 42.4%, we cannot conclude that this was solely due to our interventions. Limitations include reliance on ICD-10 codes and inaccurate home medication lists. Additional de-implementation strategies could decrease PPI orders during hospitalization and at discharge.
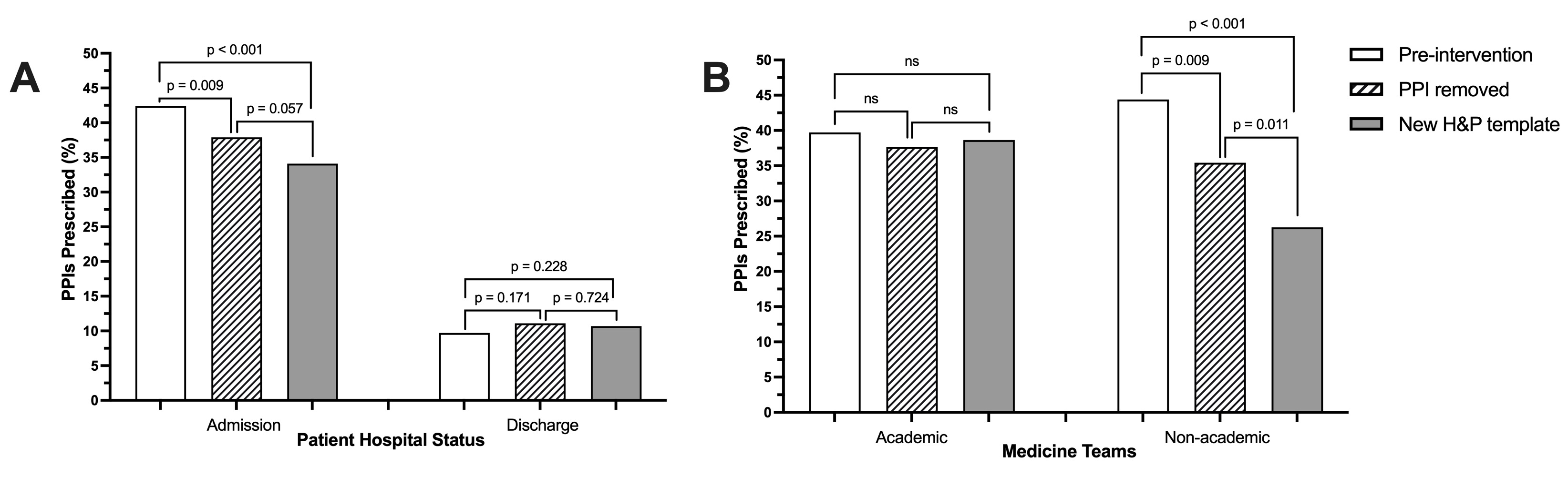
Figure: Figure 1. Rates of PPI orders on admission in (A) all non-critically ill admitted patients and in (B) patients stratified by academic vs non-academic teams.
Note: ns: non-significant
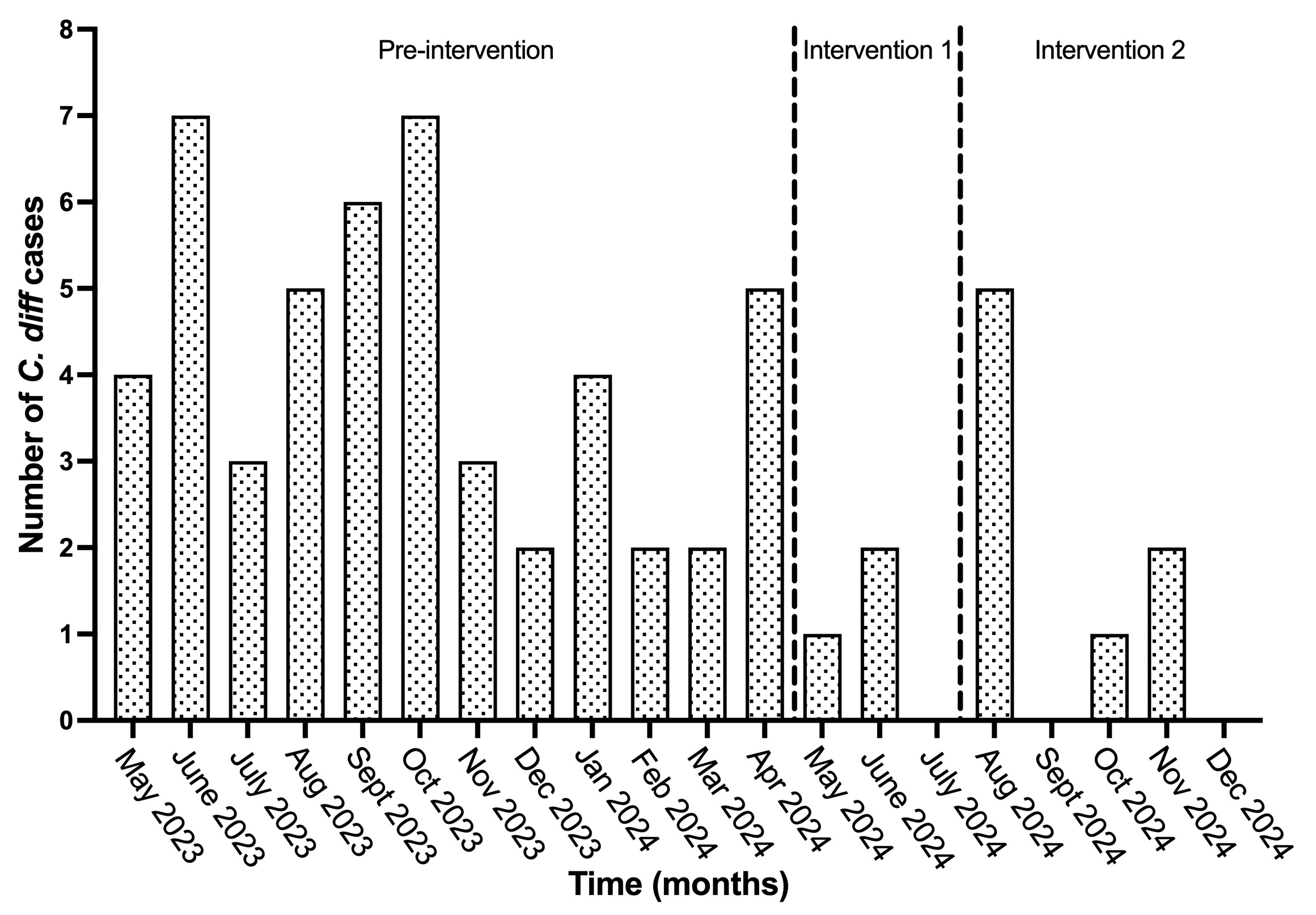
Figure: Figure 2. Number of C. diff infections throughout the study periods
Disclosures:
Matthew Ryan indicated no relevant financial relationships.
Christopher Ma indicated no relevant financial relationships.
Ami Panara Shukla indicated no relevant financial relationships.
Marlene Onaindia indicated no relevant financial relationships.
Sebastian Suarez indicated no relevant financial relationships.
Matthew Ryan, MD1, Christopher Ma, MD2, Ami Panara Shukla, MD2, Marlene Onaindia, PharmD2, Sebastian Suarez, MD, MPH2, 12, Reducing Inappropriate Proton Pump Inhibitor Prescribing in Non-Critically Ill Hospitalized Patients: A Single Center Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.



