Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 1B: Pancreas
15 - Novel Mesenteric-Based Imaging Classification Predicts Oral Feeding Intolerance in Acute Pancreatitis
Monday, October 27, 2025
2:15 PM - 2:25 PM PDT
Location: North Ballroom 120BC
Gaurav Suryawanshi, MD (he/him/his)
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Gaurav Suryawanshi, MD1, Petr Vanek, MD, PhD2, Nauroze Faizi, MD1, Guru Trikudanathan, MD1
1University of Minnesota, Minneapolis, MN; 2University of Minnesota, Minneapolis, USA; Palacky University Olomouc, Olomouc, Czech Republic, Minneapolis, MN
Introduction: Oral feeding intolerance (OFI) delays recovery and discharge in acute pancreatitis (AP). Timely resumption of an oral diet is recommended to preserve gut barrier integrity, limit the need for artificial nutrition, and shorten the length of stay. However, early predictors remain underexplored, and the ability to predict OFI during the admission remains elusive. We hypothesized that mesenteric inflammatory changes seen on the admission CT could predict OFI.
Methods: Adult AP patients admitted between 2019–2023 were identified from a prospective database. Exclusions were absence of a contrast-enhanced CT 3–7 days from pain onset or initial care outside our system. Patients were placed in two groups based on whether they had OFI, defined as requiring enteral nutrition or total parenteral nutrition (TPN). Two abdominal radiologists, blinded to outcomes, graded the level of mesenteric inflammation: Type 0 – none; Type 1 – changes involving the mesenteric root with vascular engorgement and focal fat stranding; Type 2 – diffuse mesenteric fat stranding without mass effect; Type 3 – diffuse mesenteric fat stranding with mass effect. Baseline demographic, clinical, and radiologic variables were compared between the groups. Univariable and multivariable analysis was completed to identify independent predictors of OFI. A p< 0.05 was considered significant.
Results: Of 285 included patients (median age 44 [33-57] y; 62% male), 32 (11.2%) developed OFI. The incidence of OFI correlated with increasing mesenteric grade (Cochran-Armitage trend, p< 0.001). On multivariable analysis, severe mesenteric changes (Type 2/3) independently predicted OFI (aOR 6.21; 95% CI 1.88–20.50; p=0.0027), even after adjustment for disease severity, comorbidities, and other traditional covariates.
Discussion: Severity of mesenteric inflammation on the index CT is a strong, independent predictor of OFI in AP. Integrating a simple four-tier mesenteric grading into routine imaging reports could flag high-risk patients on admission, prompting timely nutritional support and potentially improving patient outcomes by shortening hospital stay.
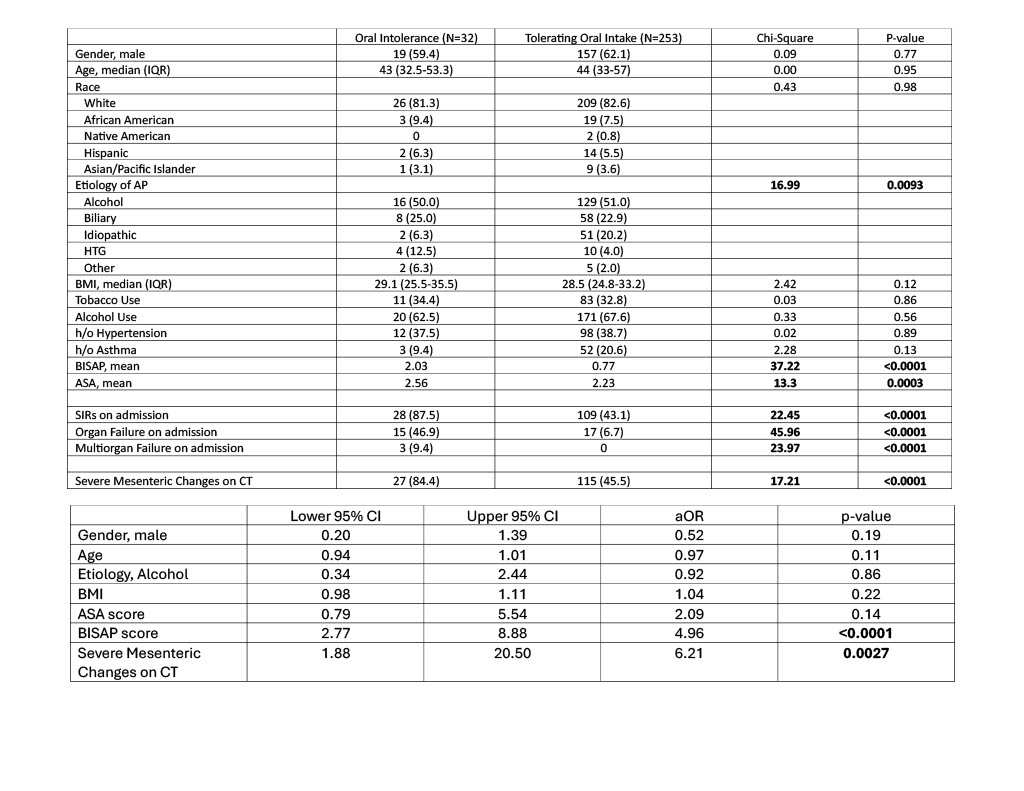
Figure: Figure 1. Representative contrast-enhanced CT images showing graded mesenteric inflammation in acute pancreatitis: (A) Type 0 – no visible changes in the mesentery; (B) Type 1 – focal changes involving the mesenteric root with vascular engorgement and fat stranding; (C) Type 2 – diffuse mesenteric fat stranding without mass effect; (D) Type 3 – diffuse mesenteric fat stranding with mass effect on adjacent structures.
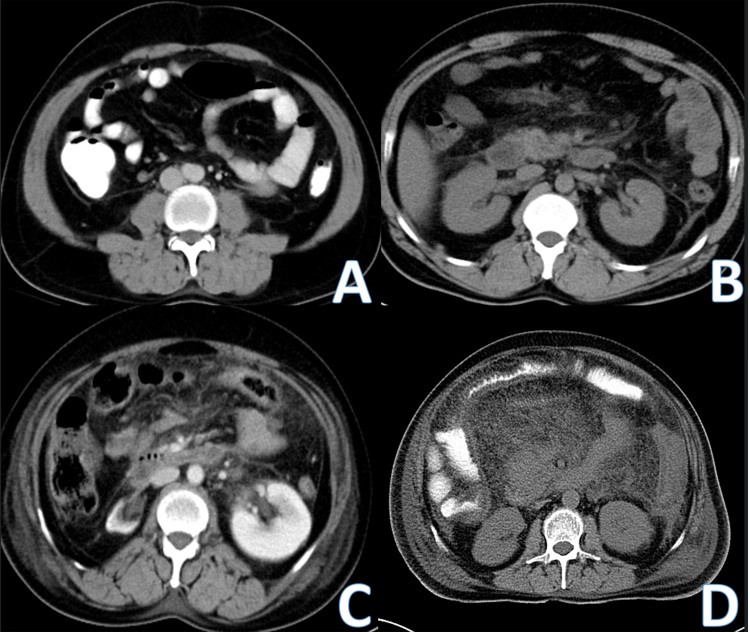
Figure: Table 1: Univariable analysis of predictors of ODI. Table 2: Multivariable analysis of predictors of ODI. aOR = adjusted odds ratio; CI = confidence interval; IQR = interquartile range; AP = acute pancreatitis; BMI = body mass index; H/o = history of; ASA = American Society of Anesthesiologists physical status classification; BISAP = Bedside Index for Severity in Acute Pancreatitis; SIRS = systemic inflammatory response syndrome; CT = computed tomography.
Disclosures:
Gaurav Suryawanshi indicated no relevant financial relationships.
Petr Vanek indicated no relevant financial relationships.
Nauroze Faizi indicated no relevant financial relationships.
Guru Trikudanathan: AbbVie – Grant/Research Support. Boston Scientific – Consultant.
Gaurav Suryawanshi, MD1, Petr Vanek, MD, PhD2, Nauroze Faizi, MD1, Guru Trikudanathan, MD1, 15, Novel Mesenteric-Based Imaging Classification Predicts Oral Feeding Intolerance in Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota, Minneapolis, USA; Palacky University Olomouc, Olomouc, Czech Republic, Minneapolis, MN
Introduction: Oral feeding intolerance (OFI) delays recovery and discharge in acute pancreatitis (AP). Timely resumption of an oral diet is recommended to preserve gut barrier integrity, limit the need for artificial nutrition, and shorten the length of stay. However, early predictors remain underexplored, and the ability to predict OFI during the admission remains elusive. We hypothesized that mesenteric inflammatory changes seen on the admission CT could predict OFI.
Methods: Adult AP patients admitted between 2019–2023 were identified from a prospective database. Exclusions were absence of a contrast-enhanced CT 3–7 days from pain onset or initial care outside our system. Patients were placed in two groups based on whether they had OFI, defined as requiring enteral nutrition or total parenteral nutrition (TPN). Two abdominal radiologists, blinded to outcomes, graded the level of mesenteric inflammation: Type 0 – none; Type 1 – changes involving the mesenteric root with vascular engorgement and focal fat stranding; Type 2 – diffuse mesenteric fat stranding without mass effect; Type 3 – diffuse mesenteric fat stranding with mass effect. Baseline demographic, clinical, and radiologic variables were compared between the groups. Univariable and multivariable analysis was completed to identify independent predictors of OFI. A p< 0.05 was considered significant.
Results: Of 285 included patients (median age 44 [33-57] y; 62% male), 32 (11.2%) developed OFI. The incidence of OFI correlated with increasing mesenteric grade (Cochran-Armitage trend, p< 0.001). On multivariable analysis, severe mesenteric changes (Type 2/3) independently predicted OFI (aOR 6.21; 95% CI 1.88–20.50; p=0.0027), even after adjustment for disease severity, comorbidities, and other traditional covariates.
Discussion: Severity of mesenteric inflammation on the index CT is a strong, independent predictor of OFI in AP. Integrating a simple four-tier mesenteric grading into routine imaging reports could flag high-risk patients on admission, prompting timely nutritional support and potentially improving patient outcomes by shortening hospital stay.
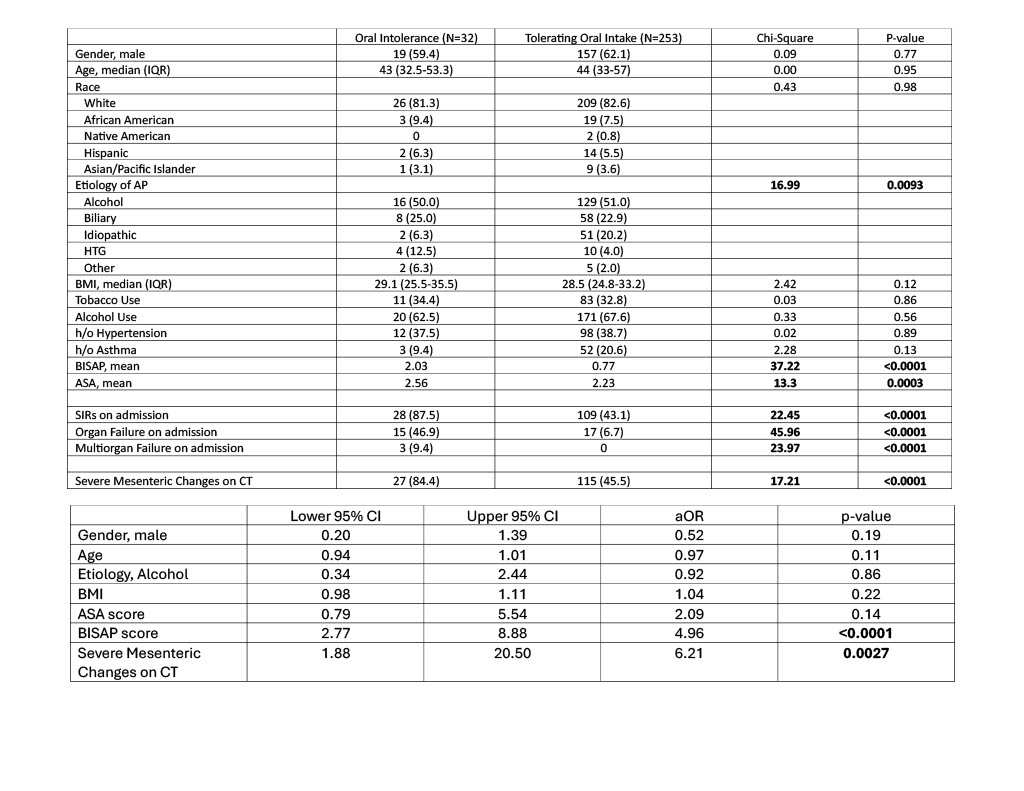
Figure: Figure 1. Representative contrast-enhanced CT images showing graded mesenteric inflammation in acute pancreatitis: (A) Type 0 – no visible changes in the mesentery; (B) Type 1 – focal changes involving the mesenteric root with vascular engorgement and fat stranding; (C) Type 2 – diffuse mesenteric fat stranding without mass effect; (D) Type 3 – diffuse mesenteric fat stranding with mass effect on adjacent structures.
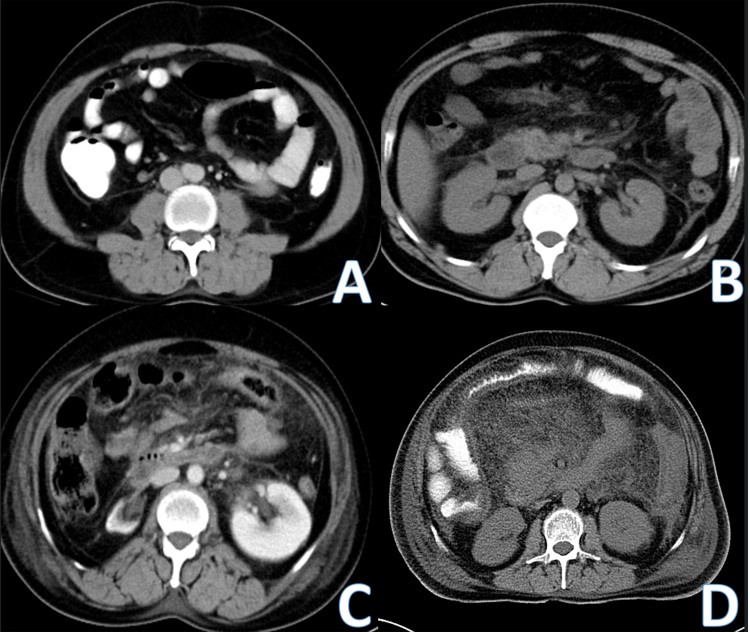
Figure: Table 1: Univariable analysis of predictors of ODI. Table 2: Multivariable analysis of predictors of ODI. aOR = adjusted odds ratio; CI = confidence interval; IQR = interquartile range; AP = acute pancreatitis; BMI = body mass index; H/o = history of; ASA = American Society of Anesthesiologists physical status classification; BISAP = Bedside Index for Severity in Acute Pancreatitis; SIRS = systemic inflammatory response syndrome; CT = computed tomography.
Disclosures:
Gaurav Suryawanshi indicated no relevant financial relationships.
Petr Vanek indicated no relevant financial relationships.
Nauroze Faizi indicated no relevant financial relationships.
Guru Trikudanathan: AbbVie – Grant/Research Support. Boston Scientific – Consultant.
Gaurav Suryawanshi, MD1, Petr Vanek, MD, PhD2, Nauroze Faizi, MD1, Guru Trikudanathan, MD1, 15, Novel Mesenteric-Based Imaging Classification Predicts Oral Feeding Intolerance in Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

