Oral Paper Presentation
Annual Scientific Meeting
Session: Presidential Plenary Session 1
2 - Higher Sessile Serrated Lesion Detection Rates Are Associated With Lower Risk for Post-Colonoscopy Colorectal Cancer: Data From the New Hampshire Colonoscopy Registry
Monday, October 27, 2025
8:12 AM - 8:24 AM PDT
Location: North Ballroom 120D

Rachael Hagen, DO (she/her/hers)
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Rachael Hagen, DO1, Douglas Rex, MD2, Todd MacKenzie, PhD3, Christopher Amos, PhD4, Lynn F.. Butterly, MD3, Joseph C. Anderson, MD3
1University of Connecticut Health, Farmington, CT; 2Indiana University School of Medicine, Indianapolis, IN; 3Dartmouth College, Hanover, NH; 4University of New Mexico, Albuquerque, NM
Introduction: The adenoma detection rate (ADR) is inversely associated with post-colonoscopy colorectal cancer (PCCRC) incidence. Calculating ADR-A using data from colonoscopies for all indications, rather than screening exams alone (ADR-S), can provide rates which are easier to calculate and can mitigate gaming by endoscopists. We hypothesized that calculating sessile serrated lesion detection rates (SSLDR-A) using all exams may also be a quality metric for predicting PCCRC risk. Using New Hampshire Colonoscopy Registry (NHCR) data, we examined the association between SSLDR-A and PCCRC risk. We also compared SSLDR-A to all screening examinations (SSLDR-S).
Methods: The cohort included NHCR 115,585 patients with an index colonoscopy. The primary outcome was PCCRC, defined as CRC diagnosed ≥6 months after the index colonoscopy. The exposure variables were endoscopist-specific SSLDR-A (calculated using all exams) and SSLDR-S (using screening exams), stratified into quintiles. Cox regression was used to model the hazard of PCCRC on SSLDR, adjusting for relevant covariates, such as patient age and sex.
Results: The cohort included NHCR 115,585 patients with an index colonoscopy. There were 177 PCCRCs diagnosed. Higher SSLDR-A and SSLDR-S rates were associated with lower PCCRC risks (Table 1). After adjusting for covariates, we observed that higher SSLDR-A rates were associated with lower hazard ratios (HR) as compared to the reference group (SSLDR-A:< 1.5%; HR=1.0 vs. SSLDR-A:1.5 to < 3.0%; HR=0.53, 95% CI 0.35-0.79; SSLDR-A:3.0-< 5.0%; HR=0.59, 95% CI 0.38-0.92; SSLDR:5.0-< 8.0%; HR=0.44, 95% CI 0.28-0.70; and SSLDR:8.0+% HR=0.20, 95% CI 0.08-0.46). The highest quintile of SSLDR-A (8.0%+) (HR=0.20, 95% CI 0.08-0.46) and SSLDR-S (8.0%+) (HR=0.20, 95% CI 0.09-0.44) provided similar protection from PCCRC (Table 1). Comparing SSLDR-A and SSLDR-S, of 126 endoscopists sampled, most (74%) remained in the same quintile.
Discussion: These findings demonstrate that colonoscopies performed by endoscopists with higher SSLDR-A are associated with a lower risk of PCCRC, validating SSLDR-A as a quality metric. We observed that most endoscopists remained in the same quintile rank but about one-quarter moved to a different quintile, a proportion similar to that observed in similar ADR analyses. Furthermore, our data suggest that endoscopists should aim for a SSLDR-A of 8.0% or higher.
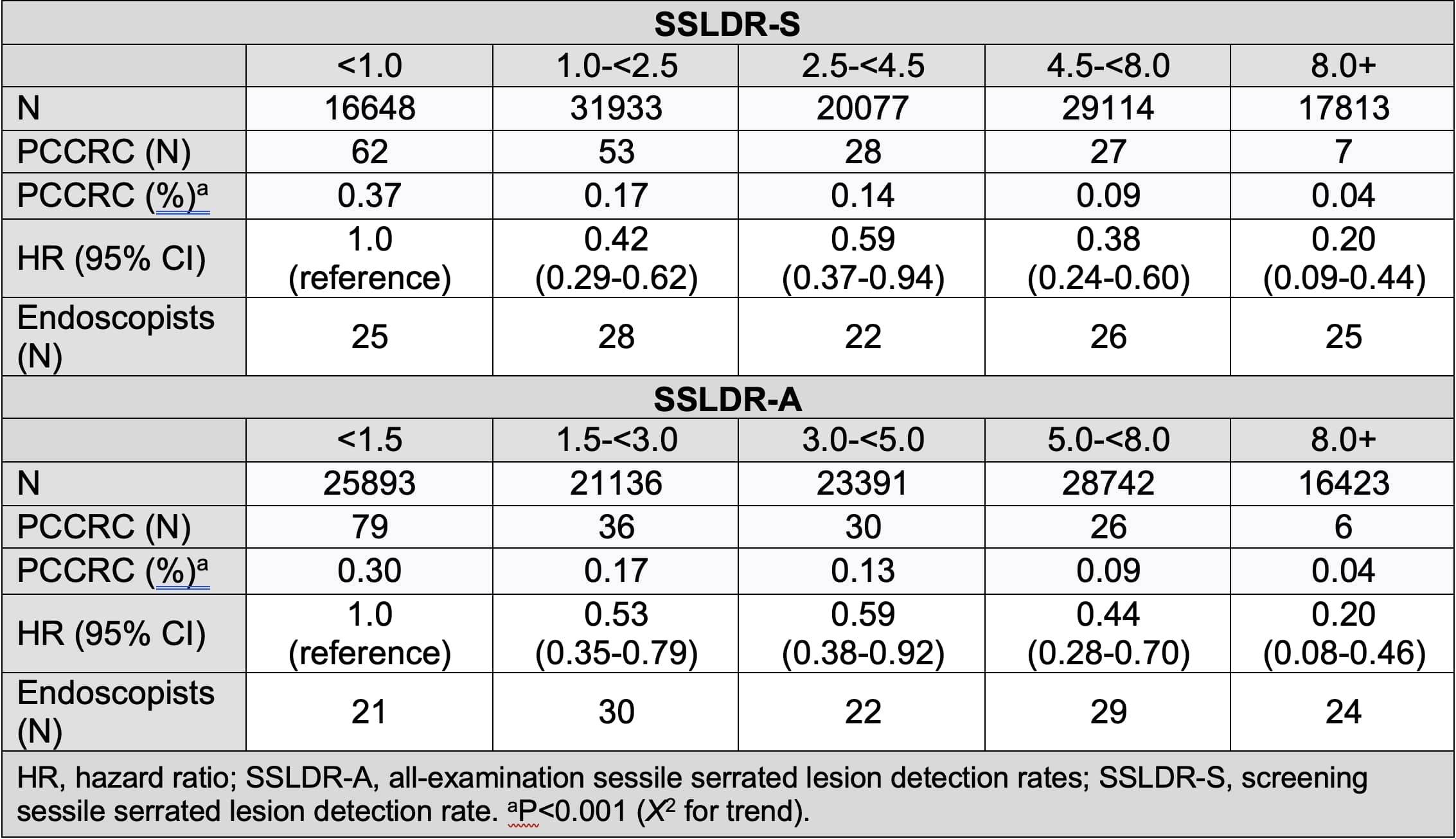
Figure: Table 1. Unadjusted risks and adjusted hazard ratios for post-colonoscopy colorectal cancer for quintiles of endoscopist SSLDR-S and SSLDR-A.
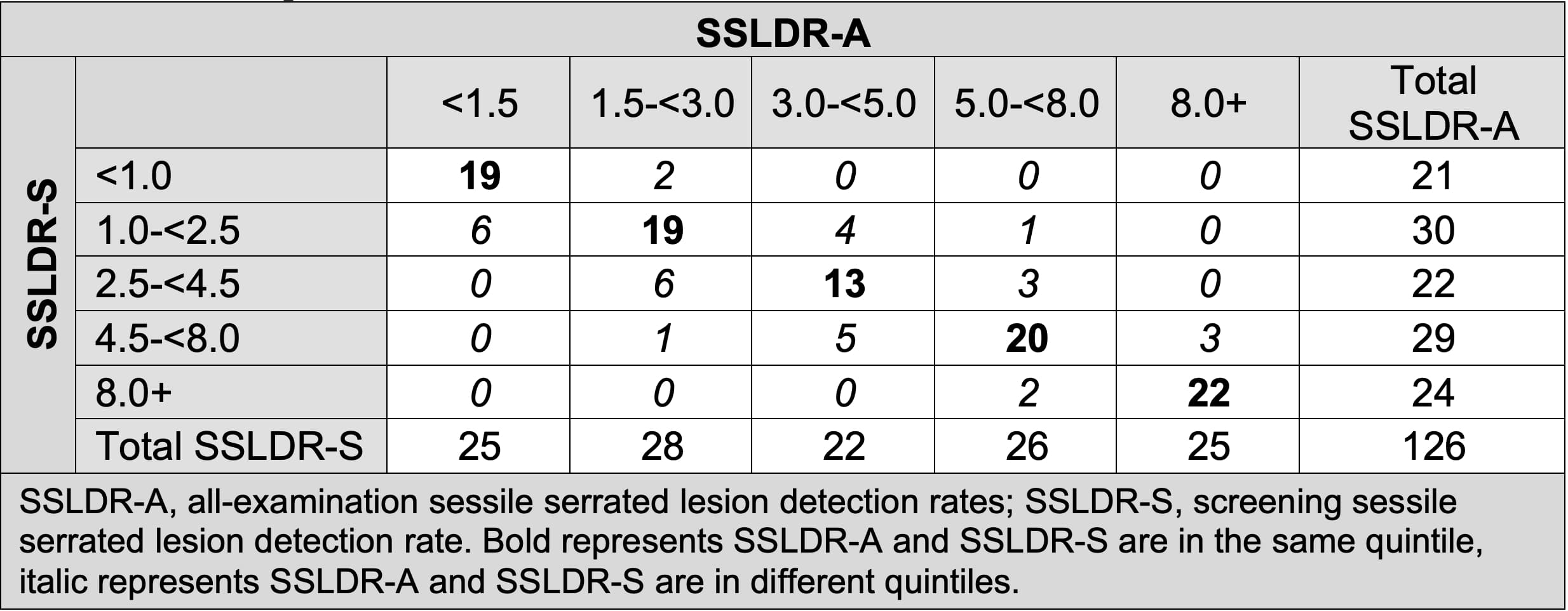
Figure: Table 2. Endoscopists' detection rates as stratified by quintiles when calculating detection rates as SSLDR-A compared to SSLDR-S.
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Douglas Rex indicated no relevant financial relationships.
Todd MacKenzie indicated no relevant financial relationships.
Christopher Amos indicated no relevant financial relationships.
Lynn Butterly indicated no relevant financial relationships.
Joseph Anderson indicated no relevant financial relationships.
Rachael Hagen, DO1, Douglas Rex, MD2, Todd MacKenzie, PhD3, Christopher Amos, PhD4, Lynn F.. Butterly, MD3, Joseph C. Anderson, MD3, 2, Higher Sessile Serrated Lesion Detection Rates Are Associated With Lower Risk for Post-Colonoscopy Colorectal Cancer: Data From the New Hampshire Colonoscopy Registry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2Indiana University School of Medicine, Indianapolis, IN; 3Dartmouth College, Hanover, NH; 4University of New Mexico, Albuquerque, NM
Introduction: The adenoma detection rate (ADR) is inversely associated with post-colonoscopy colorectal cancer (PCCRC) incidence. Calculating ADR-A using data from colonoscopies for all indications, rather than screening exams alone (ADR-S), can provide rates which are easier to calculate and can mitigate gaming by endoscopists. We hypothesized that calculating sessile serrated lesion detection rates (SSLDR-A) using all exams may also be a quality metric for predicting PCCRC risk. Using New Hampshire Colonoscopy Registry (NHCR) data, we examined the association between SSLDR-A and PCCRC risk. We also compared SSLDR-A to all screening examinations (SSLDR-S).
Methods: The cohort included NHCR 115,585 patients with an index colonoscopy. The primary outcome was PCCRC, defined as CRC diagnosed ≥6 months after the index colonoscopy. The exposure variables were endoscopist-specific SSLDR-A (calculated using all exams) and SSLDR-S (using screening exams), stratified into quintiles. Cox regression was used to model the hazard of PCCRC on SSLDR, adjusting for relevant covariates, such as patient age and sex.
Results: The cohort included NHCR 115,585 patients with an index colonoscopy. There were 177 PCCRCs diagnosed. Higher SSLDR-A and SSLDR-S rates were associated with lower PCCRC risks (Table 1). After adjusting for covariates, we observed that higher SSLDR-A rates were associated with lower hazard ratios (HR) as compared to the reference group (SSLDR-A:< 1.5%; HR=1.0 vs. SSLDR-A:1.5 to < 3.0%; HR=0.53, 95% CI 0.35-0.79; SSLDR-A:3.0-< 5.0%; HR=0.59, 95% CI 0.38-0.92; SSLDR:5.0-< 8.0%; HR=0.44, 95% CI 0.28-0.70; and SSLDR:8.0+% HR=0.20, 95% CI 0.08-0.46). The highest quintile of SSLDR-A (8.0%+) (HR=0.20, 95% CI 0.08-0.46) and SSLDR-S (8.0%+) (HR=0.20, 95% CI 0.09-0.44) provided similar protection from PCCRC (Table 1). Comparing SSLDR-A and SSLDR-S, of 126 endoscopists sampled, most (74%) remained in the same quintile.
Discussion: These findings demonstrate that colonoscopies performed by endoscopists with higher SSLDR-A are associated with a lower risk of PCCRC, validating SSLDR-A as a quality metric. We observed that most endoscopists remained in the same quintile rank but about one-quarter moved to a different quintile, a proportion similar to that observed in similar ADR analyses. Furthermore, our data suggest that endoscopists should aim for a SSLDR-A of 8.0% or higher.
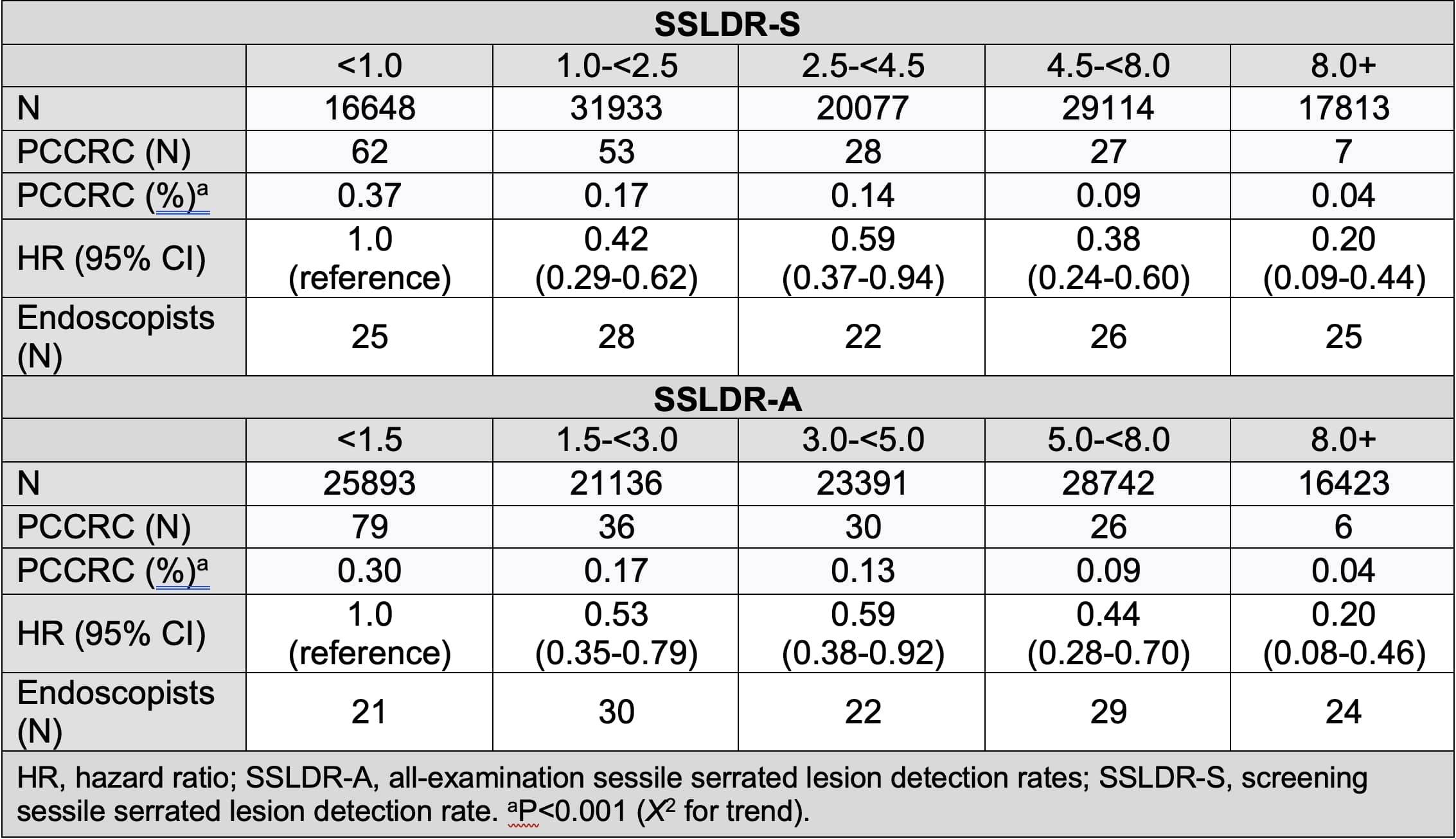
Figure: Table 1. Unadjusted risks and adjusted hazard ratios for post-colonoscopy colorectal cancer for quintiles of endoscopist SSLDR-S and SSLDR-A.
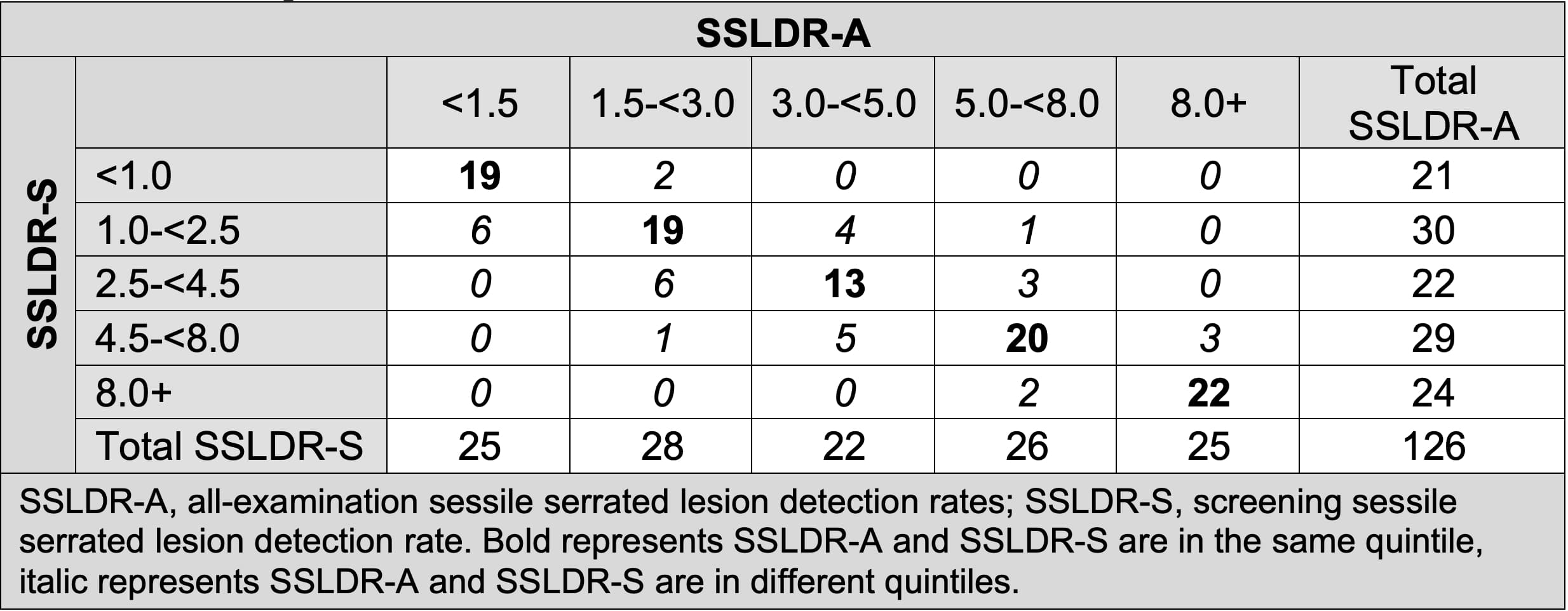
Figure: Table 2. Endoscopists' detection rates as stratified by quintiles when calculating detection rates as SSLDR-A compared to SSLDR-S.
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Douglas Rex indicated no relevant financial relationships.
Todd MacKenzie indicated no relevant financial relationships.
Christopher Amos indicated no relevant financial relationships.
Lynn Butterly indicated no relevant financial relationships.
Joseph Anderson indicated no relevant financial relationships.
Rachael Hagen, DO1, Douglas Rex, MD2, Todd MacKenzie, PhD3, Christopher Amos, PhD4, Lynn F.. Butterly, MD3, Joseph C. Anderson, MD3, 2, Higher Sessile Serrated Lesion Detection Rates Are Associated With Lower Risk for Post-Colonoscopy Colorectal Cancer: Data From the New Hampshire Colonoscopy Registry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.



