Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3A: Liver / Functional
44 - Trends and Disparities in Mortality From Obesity-Associated Gastrointestinal Cancers in the United States, 1999–2020: A CDC WONDER Analysis
Tuesday, October 28, 2025
3:25 PM - 3:35 PM PDT
Location: North Ballroom 120D

Usama Sakhawat, MD
United Health Services, Wilson Medical Center
BINGHAMTON, NY
Presenting Author(s)
Award: ACG Outstanding Research Award in the Diet, Nutrition, and Obesity Category (Trainee)
Usama Sakhawat, MD1, Usman Mazhar, MBBS2, Ahmed Shehadah, MD3, Hafsah Ali, MBBS4, Daniyal Abbasi, MBBS5, Ali Hamza, MBBS6, Fnu Veena, MD7, Muhammad Hamza Rafique, MD8, Usama Bilal, MBBS9, Maham Waqar, MBBS10, Allah Dad, MD11, Sheena Shamoon, MD12, Muhammad Arham, 13, Faseeh Haider, MD14, Faizan Ahmad, MD15, Fatima Binte Athar, MBBS16, Moheudin Khan, MD1, Toseef Javaid, MD1
1United Health Services, Wilson Medical Center, Johnson City, NY; 2Rawalpindi Medical University, Pakistan, Rawalpindi, Punjab, Pakistan; 3United Health Services, Wilson Medical Center, Binghamton, NY; 4Allama Iqbal Medical College, Manama, Al Muharraq, Bahrain; 5Islamabad Medical and Dental College, Islamabad, Islamabad, Pakistan; 6Army Medical College, Rawalpindi, Punjab, Pakistan; 7BronxCare Health System, Bronx, NY; 8Woodhull Medical Center, Brooklyn, NY; 9Rawalpindi Medical University, Rawalpindi, Rawalpindi, Punjab, Pakistan; 10Rawalpindi Medical University, Rawalpindi, Punjab, Pakistan; 11Shiekh Zayed Medical College Rahim Yar Khan, Pakistan, Kot Addu, Punjab, Pakistan; 12University at Buffalo, Buffalo, NY; 13Sheikh Zayed Medical College, Pakistan, Rahim Yar Khan, Punjab, Pakistan; 14Allama Iqbal Medical college, Lahore, Punjab, Pakistan; 15Duke University, Durham, NC; 16Karachi Medical And Dental College, Karachi, Sindh, Pakistan
Introduction: The incidence of obesity-related cancers has increased markedly over the past two decades, paralleling the rise in obesity prevalence across the United States. Among these, gastrointestinal (GI) cancers have shown particularly strong associations with excess body weight. Monitoring mortality trends linked to these cancers is critical to understanding obesity’s long-term effects on cancer outcomes.
Methods: We conducted a retrospective analysis of adults aged ≥25 years using CDC WONDER (1999–2020) to identify deaths co-listed with obesity (E66) and obesity-associated GI cancers, including malignancies of the esophagus (C15), stomach (C16), colon (C18), rectosigmoid junction (C19), rectum (C20), liver/intrahepatic bile ducts (C22), gallbladder (C23), and pancreas (C25). Age-adjusted mortality rates (AAMRs) per million were calculated, and trends assessed using Joinpoint regression by sex, race/ethnicity, region, and urbanization level.
Results: From 1999 to 2020, AAMR for obesity-associated gastrointestinal (GI) cancers increased from 0.8 to 2.6 per million (AAPC: +5.48%, CI: +4.43 to +6.53, p < 0.001). A total of 7,232 deaths were recorded. Mortality rose steadily from 1999 to 2018 (APC: +4.45%, CI: +3.89 to +5.03, p < 0.001), followed by a sharper increase from 2018 to 2020 (APC: +15.67%, CI: +4.68 to +27.81, p = 0.006). AAMRs rose across all demographic and geographic subgroups. By 2020, males had a higher AAMR (3.3) than females (2.3). Non-Hispanic (NH) American Indian or Alaska Native individuals had the highest overall AAMR(2.6). followed by NH Black (1.9), NH Whites (1.5),Hispanics(1.2),NH Asian or Pacific Islander(0.3).The Midwest had the highest regional AAMR (1.7), followed by the West (1.6),South (1.4), and Northeast (1.2). Urbanization analysis showed greater mortality in non-metropolitan areas (AAMR=2) compared to metropolitan areas (AAMR=1.4). Although age-specific Joinpoint analysis could not be performed due to data variability, descriptive trends indicated increases across all adult age groups.
Discussion: Mortality from obesity-related GI cancers has more than tripled over two decades, with accelerated increases in recent years. The disparities across sex, race, region, and urbanization highlight a need for focused prevention. Strengthening obesity control measures, increasing early GI cancer screening, and enhancing equitable access to care should be central to national public health strategies.
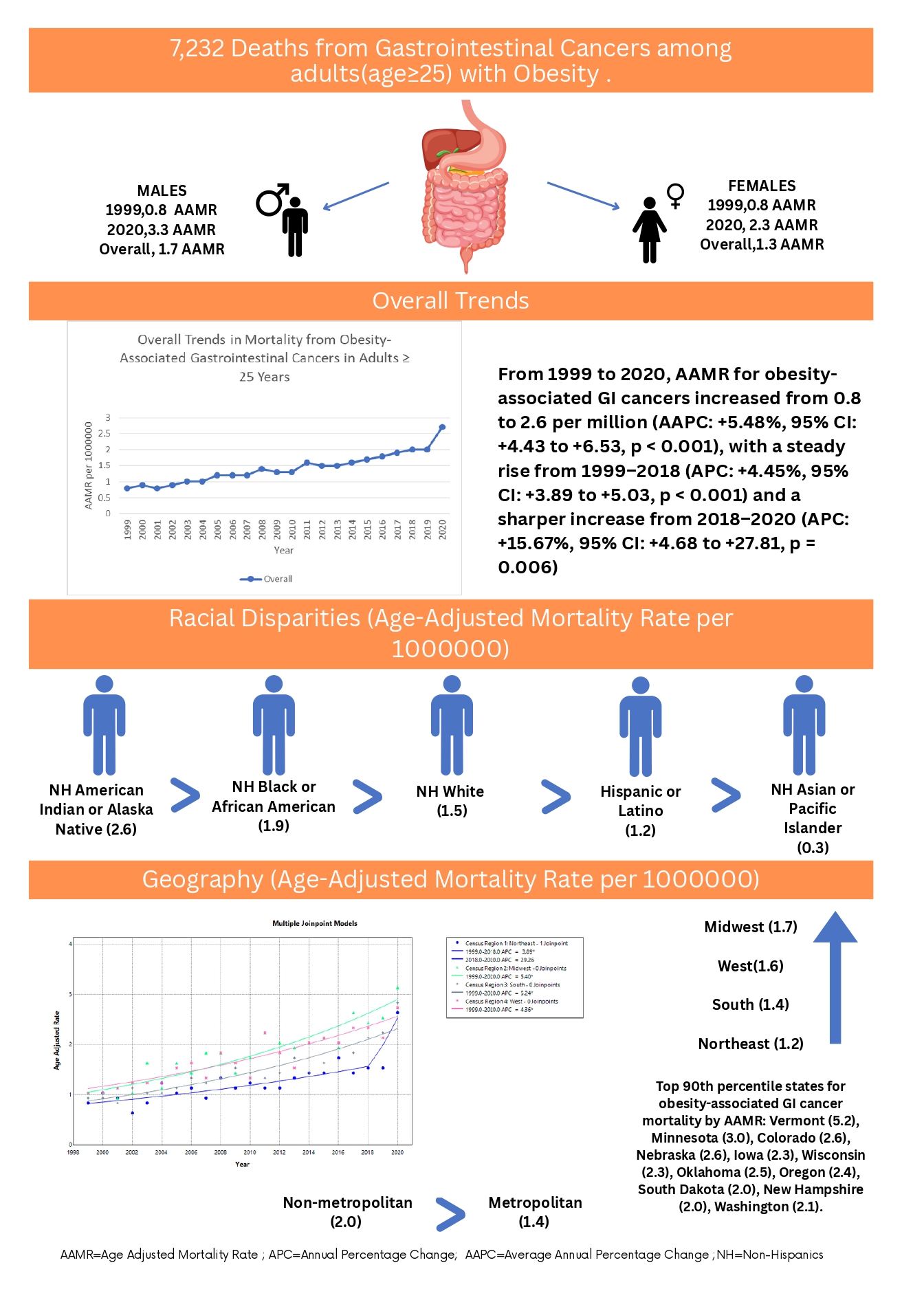
Figure: Figure 1: Trends and Disparities in Mortality from Obesity-Associated Gastrointestinal Cancers in the United States, 1999–2020: A CDC WONDER Analysis.
Disclosures:
Usama Sakhawat indicated no relevant financial relationships.
Usman Mazhar indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Hafsah Ali indicated no relevant financial relationships.
Daniyal Abbasi indicated no relevant financial relationships.
Ali Hamza indicated no relevant financial relationships.
Fnu Veena indicated no relevant financial relationships.
Muhammad Hamza Rafique indicated no relevant financial relationships.
Usama Bilal indicated no relevant financial relationships.
Maham Waqar indicated no relevant financial relationships.
Allah Dad indicated no relevant financial relationships.
Sheena Shamoon indicated no relevant financial relationships.
Muhammad Arham indicated no relevant financial relationships.
Faseeh Haider indicated no relevant financial relationships.
Faizan Ahmad indicated no relevant financial relationships.
Fatima Binte Athar indicated no relevant financial relationships.
Moheudin Khan indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Usama Sakhawat, MD1, Usman Mazhar, MBBS2, Ahmed Shehadah, MD3, Hafsah Ali, MBBS4, Daniyal Abbasi, MBBS5, Ali Hamza, MBBS6, Fnu Veena, MD7, Muhammad Hamza Rafique, MD8, Usama Bilal, MBBS9, Maham Waqar, MBBS10, Allah Dad, MD11, Sheena Shamoon, MD12, Muhammad Arham, 13, Faseeh Haider, MD14, Faizan Ahmad, MD15, Fatima Binte Athar, MBBS16, Moheudin Khan, MD1, Toseef Javaid, MD1, 44, Trends and Disparities in Mortality From Obesity-Associated Gastrointestinal Cancers in the United States, 1999–2020: A CDC WONDER Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Usama Sakhawat, MD1, Usman Mazhar, MBBS2, Ahmed Shehadah, MD3, Hafsah Ali, MBBS4, Daniyal Abbasi, MBBS5, Ali Hamza, MBBS6, Fnu Veena, MD7, Muhammad Hamza Rafique, MD8, Usama Bilal, MBBS9, Maham Waqar, MBBS10, Allah Dad, MD11, Sheena Shamoon, MD12, Muhammad Arham, 13, Faseeh Haider, MD14, Faizan Ahmad, MD15, Fatima Binte Athar, MBBS16, Moheudin Khan, MD1, Toseef Javaid, MD1
1United Health Services, Wilson Medical Center, Johnson City, NY; 2Rawalpindi Medical University, Pakistan, Rawalpindi, Punjab, Pakistan; 3United Health Services, Wilson Medical Center, Binghamton, NY; 4Allama Iqbal Medical College, Manama, Al Muharraq, Bahrain; 5Islamabad Medical and Dental College, Islamabad, Islamabad, Pakistan; 6Army Medical College, Rawalpindi, Punjab, Pakistan; 7BronxCare Health System, Bronx, NY; 8Woodhull Medical Center, Brooklyn, NY; 9Rawalpindi Medical University, Rawalpindi, Rawalpindi, Punjab, Pakistan; 10Rawalpindi Medical University, Rawalpindi, Punjab, Pakistan; 11Shiekh Zayed Medical College Rahim Yar Khan, Pakistan, Kot Addu, Punjab, Pakistan; 12University at Buffalo, Buffalo, NY; 13Sheikh Zayed Medical College, Pakistan, Rahim Yar Khan, Punjab, Pakistan; 14Allama Iqbal Medical college, Lahore, Punjab, Pakistan; 15Duke University, Durham, NC; 16Karachi Medical And Dental College, Karachi, Sindh, Pakistan
Introduction: The incidence of obesity-related cancers has increased markedly over the past two decades, paralleling the rise in obesity prevalence across the United States. Among these, gastrointestinal (GI) cancers have shown particularly strong associations with excess body weight. Monitoring mortality trends linked to these cancers is critical to understanding obesity’s long-term effects on cancer outcomes.
Methods: We conducted a retrospective analysis of adults aged ≥25 years using CDC WONDER (1999–2020) to identify deaths co-listed with obesity (E66) and obesity-associated GI cancers, including malignancies of the esophagus (C15), stomach (C16), colon (C18), rectosigmoid junction (C19), rectum (C20), liver/intrahepatic bile ducts (C22), gallbladder (C23), and pancreas (C25). Age-adjusted mortality rates (AAMRs) per million were calculated, and trends assessed using Joinpoint regression by sex, race/ethnicity, region, and urbanization level.
Results: From 1999 to 2020, AAMR for obesity-associated gastrointestinal (GI) cancers increased from 0.8 to 2.6 per million (AAPC: +5.48%, CI: +4.43 to +6.53, p < 0.001). A total of 7,232 deaths were recorded. Mortality rose steadily from 1999 to 2018 (APC: +4.45%, CI: +3.89 to +5.03, p < 0.001), followed by a sharper increase from 2018 to 2020 (APC: +15.67%, CI: +4.68 to +27.81, p = 0.006). AAMRs rose across all demographic and geographic subgroups. By 2020, males had a higher AAMR (3.3) than females (2.3). Non-Hispanic (NH) American Indian or Alaska Native individuals had the highest overall AAMR(2.6). followed by NH Black (1.9), NH Whites (1.5),Hispanics(1.2),NH Asian or Pacific Islander(0.3).The Midwest had the highest regional AAMR (1.7), followed by the West (1.6),South (1.4), and Northeast (1.2). Urbanization analysis showed greater mortality in non-metropolitan areas (AAMR=2) compared to metropolitan areas (AAMR=1.4). Although age-specific Joinpoint analysis could not be performed due to data variability, descriptive trends indicated increases across all adult age groups.
Discussion: Mortality from obesity-related GI cancers has more than tripled over two decades, with accelerated increases in recent years. The disparities across sex, race, region, and urbanization highlight a need for focused prevention. Strengthening obesity control measures, increasing early GI cancer screening, and enhancing equitable access to care should be central to national public health strategies.
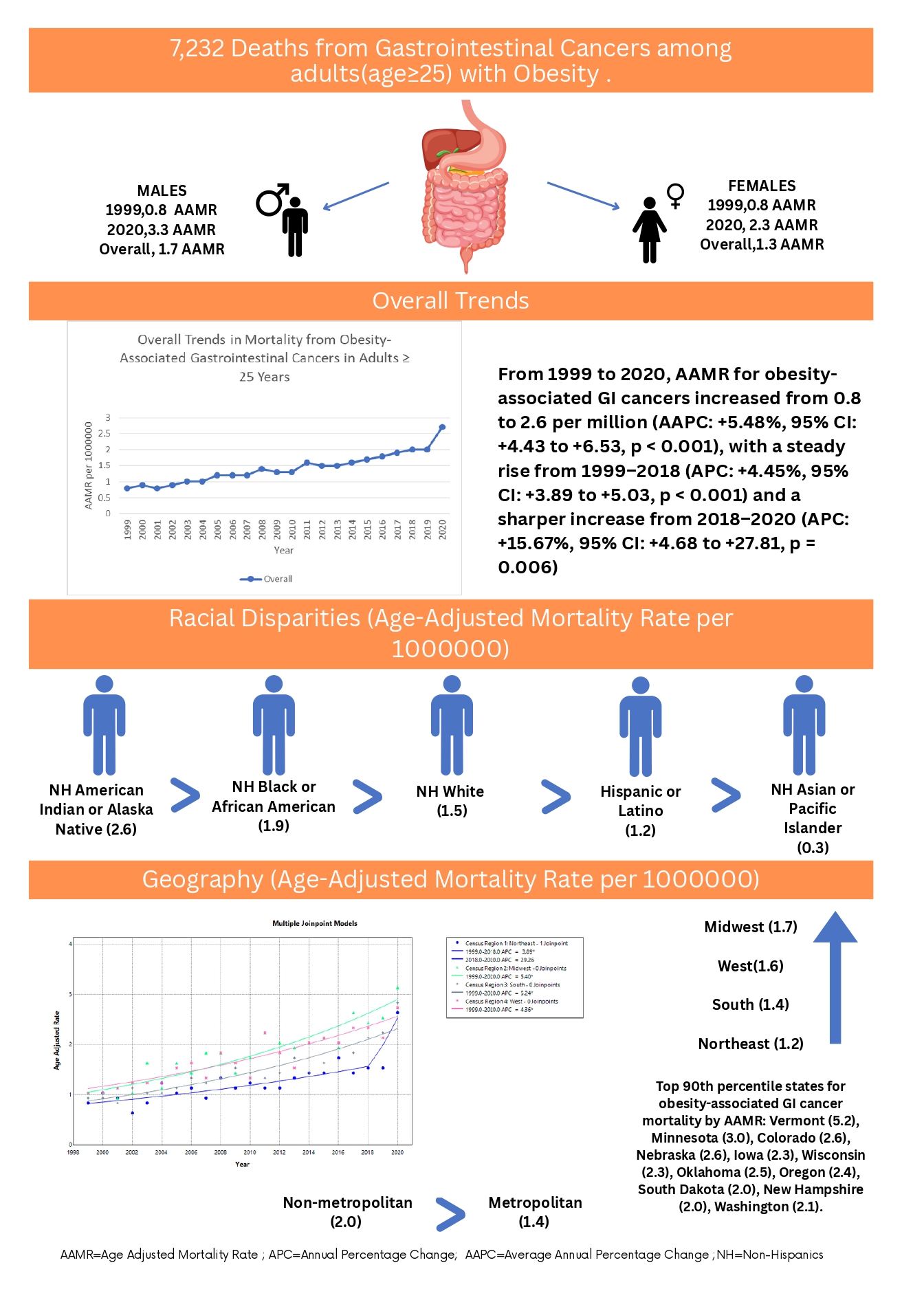
Figure: Figure 1: Trends and Disparities in Mortality from Obesity-Associated Gastrointestinal Cancers in the United States, 1999–2020: A CDC WONDER Analysis.
Disclosures:
Usama Sakhawat indicated no relevant financial relationships.
Usman Mazhar indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Hafsah Ali indicated no relevant financial relationships.
Daniyal Abbasi indicated no relevant financial relationships.
Ali Hamza indicated no relevant financial relationships.
Fnu Veena indicated no relevant financial relationships.
Muhammad Hamza Rafique indicated no relevant financial relationships.
Usama Bilal indicated no relevant financial relationships.
Maham Waqar indicated no relevant financial relationships.
Allah Dad indicated no relevant financial relationships.
Sheena Shamoon indicated no relevant financial relationships.
Muhammad Arham indicated no relevant financial relationships.
Faseeh Haider indicated no relevant financial relationships.
Faizan Ahmad indicated no relevant financial relationships.
Fatima Binte Athar indicated no relevant financial relationships.
Moheudin Khan indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Usama Sakhawat, MD1, Usman Mazhar, MBBS2, Ahmed Shehadah, MD3, Hafsah Ali, MBBS4, Daniyal Abbasi, MBBS5, Ali Hamza, MBBS6, Fnu Veena, MD7, Muhammad Hamza Rafique, MD8, Usama Bilal, MBBS9, Maham Waqar, MBBS10, Allah Dad, MD11, Sheena Shamoon, MD12, Muhammad Arham, 13, Faseeh Haider, MD14, Faizan Ahmad, MD15, Fatima Binte Athar, MBBS16, Moheudin Khan, MD1, Toseef Javaid, MD1, 44, Trends and Disparities in Mortality From Obesity-Associated Gastrointestinal Cancers in the United States, 1999–2020: A CDC WONDER Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.



