Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3A: Liver / Functional
40 - The Impact of Body Mass Index (BMI) and Obesity on Liver Transplant Outcomes: A Retrospective Analysis of a Single Center 8-Year Experience
Tuesday, October 28, 2025
2:45 PM - 2:55 PM PDT
Location: North Ballroom 120D
- MA
Mohammed Abusuliman, MD
Henry Ford Hospital
Dearborn, MI
Presenting Author(s)
Award: ACG Health Equity Research Award
Mohammed Abusuliman, MD1, Ali Kadouh, MD2, Agustin Gavidia Rosario, MD2, Razan Aburumman, MD2, Anju Pradeep, MD1, Jared Klutke, MD1, Tobias Cox, MD3, Amr Abusuliman, MD4, Yara Dababneh, MD1, Muhammad Zarrar Khan, MD1, Syed-Mohammed Jafri, MD2
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI; 3Wayne State School of Medicine, Detroit, MI; 4Tanta University, Qutour, Al Gharbiyah, Egypt
Introduction: Obesity is a growing global health challenge and a prevalent comorbidity in patients undergoing liver transplantation (LT). Its impact on post-transplant outcomes, including graft survival, rejection, and the need for transplantation, remains a topic of debate. We aimed to study the effects of obesity through body mass index (BMI) on LT outcomes.
Methods: We conducted a retrospective chart review on patients 18 years and older who underwent liver transplant at our center between 01/2015-01/2023. We categorized all the patients based on BMI (underweight, normal weight, overweight, obesity class 1, 2, or 3), and looked at multiple transplant outcomes, including mortality, episodes of rejection, need for re-transplantation, length of hospital stay following transplant, readmission rate within 1 year following transplant, emergent initiation of dialysis within 1 week of transplant, and graft failure.
Results: A total of 807 patients underwent liver transplant, 526 were males (65%) and 667 were white (83%). The patients were then categorized into six BMI groups, with the overweight group being the most common (n = 273, 34%). All BMI groups and baseline characteristics are listed in (Table 1).
BMI was not significantly associated with post-transplant mortality (p = 0.5), graft rejection (p = 0.6), readmissions (p = 0.9), emergent dialysis (p = 0.9), or length of hospital stay (p = 0.082).
BMI was significantly associated with the need for re-transplantation (p = 0.026) and graft failure (p = 0.013). Adjusted analysis revealed that overweight (OR: 0.34, 95% CI: 0.12–0.87), Class I obesity (OR: 0.32, 95% CI: 0.10–0.91), and Class II obesity (OR: 0.19, 95% CI: 0.03–0.77) were associated with significantly lower odds of graft failure compared to normal weight. Class III obesity showed a trend toward increased risk of re-transplantation (OR: 3.60, 95% CI: 0.84–15.4), though this did not reach statistical significance, outcomes are outlined in (Table 2)
Discussion: While extreme obesity may increase the risk of re-transplantation, overweight and moderate obesity were associated with lower odds of graft failure following liver transplantation. These findings suggest that BMI alone should not be a deterrent to transplantation candidacy.
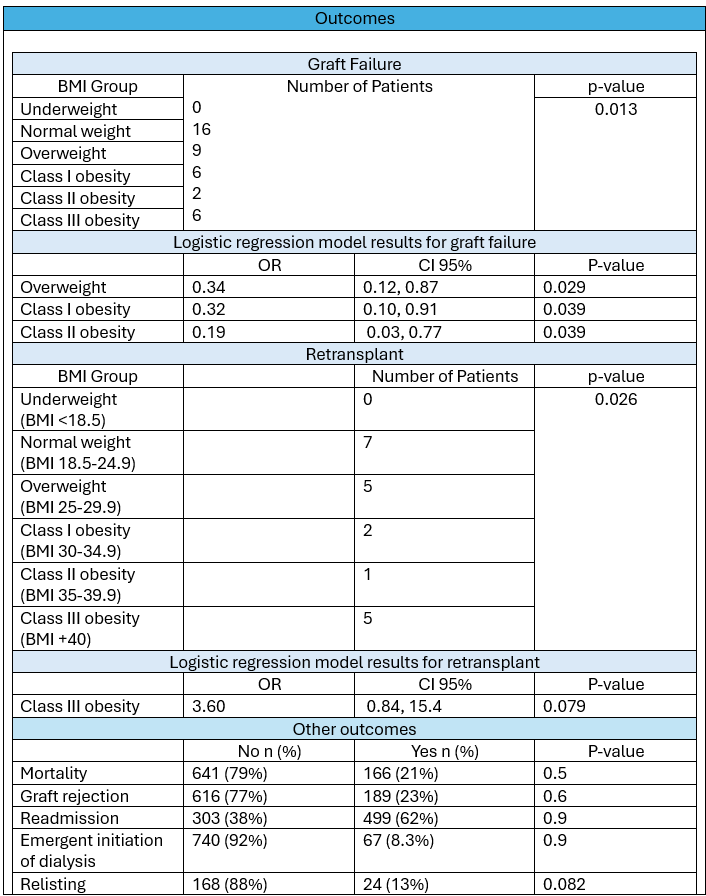
Figure: Table 1: Baseline criteria of liver transplant recipients
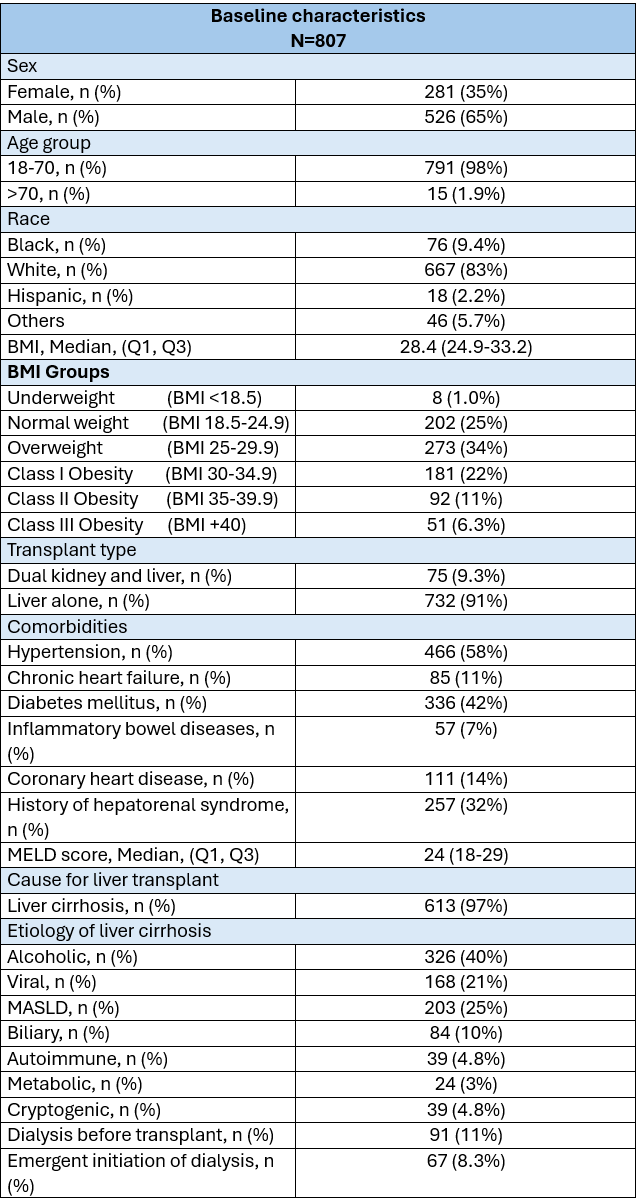
Figure: Table 2: Outcomes of liver transplantation.
Disclosures:
Mohammed Abusuliman indicated no relevant financial relationships.
Ali Kadouh indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Anju Pradeep indicated no relevant financial relationships.
Jared Klutke indicated no relevant financial relationships.
Tobias Cox indicated no relevant financial relationships.
Amr Abusuliman indicated no relevant financial relationships.
Yara Dababneh indicated no relevant financial relationships.
Muhammad Zarrar Khan indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Mohammed Abusuliman, MD1, Ali Kadouh, MD2, Agustin Gavidia Rosario, MD2, Razan Aburumman, MD2, Anju Pradeep, MD1, Jared Klutke, MD1, Tobias Cox, MD3, Amr Abusuliman, MD4, Yara Dababneh, MD1, Muhammad Zarrar Khan, MD1, Syed-Mohammed Jafri, MD2, 40, The Impact of Body Mass Index (BMI) and Obesity on Liver Transplant Outcomes: A Retrospective Analysis of a Single Center 8-Year Expericence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mohammed Abusuliman, MD1, Ali Kadouh, MD2, Agustin Gavidia Rosario, MD2, Razan Aburumman, MD2, Anju Pradeep, MD1, Jared Klutke, MD1, Tobias Cox, MD3, Amr Abusuliman, MD4, Yara Dababneh, MD1, Muhammad Zarrar Khan, MD1, Syed-Mohammed Jafri, MD2
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI; 3Wayne State School of Medicine, Detroit, MI; 4Tanta University, Qutour, Al Gharbiyah, Egypt
Introduction: Obesity is a growing global health challenge and a prevalent comorbidity in patients undergoing liver transplantation (LT). Its impact on post-transplant outcomes, including graft survival, rejection, and the need for transplantation, remains a topic of debate. We aimed to study the effects of obesity through body mass index (BMI) on LT outcomes.
Methods: We conducted a retrospective chart review on patients 18 years and older who underwent liver transplant at our center between 01/2015-01/2023. We categorized all the patients based on BMI (underweight, normal weight, overweight, obesity class 1, 2, or 3), and looked at multiple transplant outcomes, including mortality, episodes of rejection, need for re-transplantation, length of hospital stay following transplant, readmission rate within 1 year following transplant, emergent initiation of dialysis within 1 week of transplant, and graft failure.
Results: A total of 807 patients underwent liver transplant, 526 were males (65%) and 667 were white (83%). The patients were then categorized into six BMI groups, with the overweight group being the most common (n = 273, 34%). All BMI groups and baseline characteristics are listed in (Table 1).
BMI was not significantly associated with post-transplant mortality (p = 0.5), graft rejection (p = 0.6), readmissions (p = 0.9), emergent dialysis (p = 0.9), or length of hospital stay (p = 0.082).
BMI was significantly associated with the need for re-transplantation (p = 0.026) and graft failure (p = 0.013). Adjusted analysis revealed that overweight (OR: 0.34, 95% CI: 0.12–0.87), Class I obesity (OR: 0.32, 95% CI: 0.10–0.91), and Class II obesity (OR: 0.19, 95% CI: 0.03–0.77) were associated with significantly lower odds of graft failure compared to normal weight. Class III obesity showed a trend toward increased risk of re-transplantation (OR: 3.60, 95% CI: 0.84–15.4), though this did not reach statistical significance, outcomes are outlined in (Table 2)
Discussion: While extreme obesity may increase the risk of re-transplantation, overweight and moderate obesity were associated with lower odds of graft failure following liver transplantation. These findings suggest that BMI alone should not be a deterrent to transplantation candidacy.
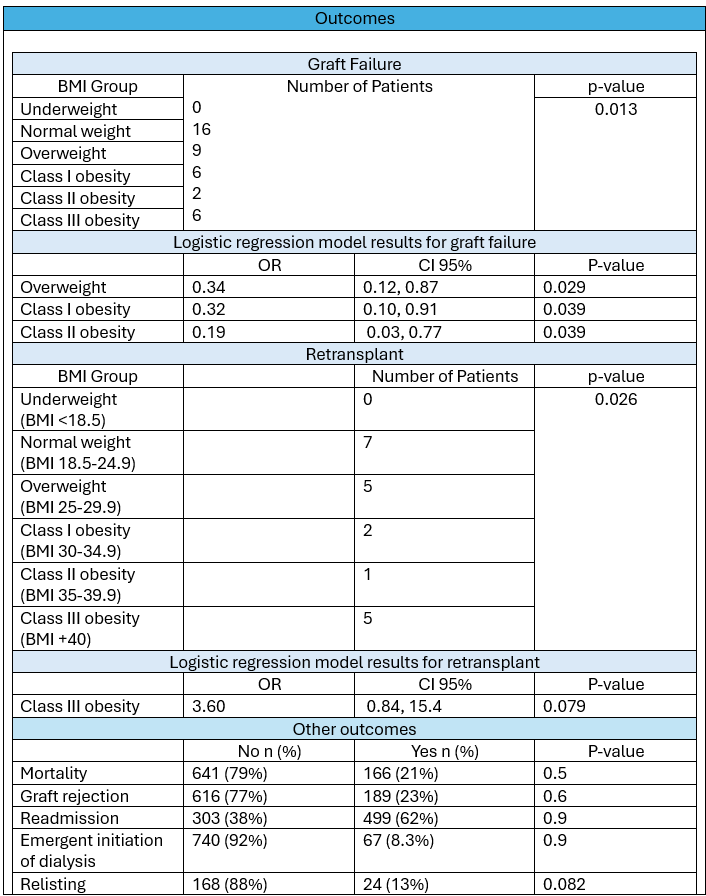
Figure: Table 1: Baseline criteria of liver transplant recipients
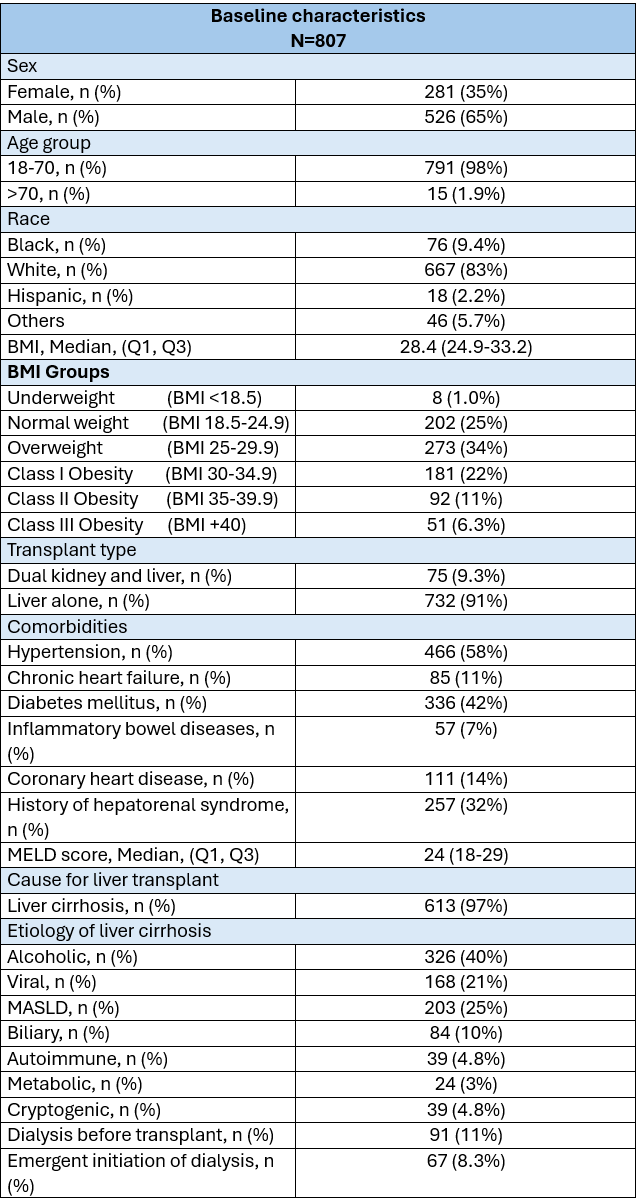
Figure: Table 2: Outcomes of liver transplantation.
Disclosures:
Mohammed Abusuliman indicated no relevant financial relationships.
Ali Kadouh indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Anju Pradeep indicated no relevant financial relationships.
Jared Klutke indicated no relevant financial relationships.
Tobias Cox indicated no relevant financial relationships.
Amr Abusuliman indicated no relevant financial relationships.
Yara Dababneh indicated no relevant financial relationships.
Muhammad Zarrar Khan indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Mohammed Abusuliman, MD1, Ali Kadouh, MD2, Agustin Gavidia Rosario, MD2, Razan Aburumman, MD2, Anju Pradeep, MD1, Jared Klutke, MD1, Tobias Cox, MD3, Amr Abusuliman, MD4, Yara Dababneh, MD1, Muhammad Zarrar Khan, MD1, Syed-Mohammed Jafri, MD2, 40, The Impact of Body Mass Index (BMI) and Obesity on Liver Transplant Outcomes: A Retrospective Analysis of a Single Center 8-Year Expericence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.



