Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 3B: Luminal GI / Endoscopy / Pancreas
47 - Utilization of the Glasgow-Blatchford Score to Guide Safe Disposition of Patients Admitted With Upper GI Bleeding: A Quality Improvement Research Project
Tuesday, October 28, 2025
2:25 PM - 2:35 PM PDT
Location: North Ballroom 120BC

Jose Garcia-Corella, MD (he/him/his)
UCLA-Kern Medical Center
Bakersfield, CA
Presenting Author(s)
Jose Garcia-Corella, MD1, Mahum Zahid, MD2, Nihad Al-Yousfi, MD2, Ikleel Moshref, MD2, BreeAnna Carlson, DO3, Nathan Lytton, DO2, Leila Moosavi, MD4, Igor Garcia-Pacheco, MD2, Kasey Fox, DO2
1UCLA-Kern Medical Center, Bakersfield, CA; 2Kern Medical Center, Bakersfield, CA; 3Western University of Health Sciences, Bakersfield, CA; 4Adventist Hospital Bakersfield, Bakersfield, CA
Introduction: Upper gastrointestinal bleeding (UGIB) is the most frequent emergency reported in gastroenterology, with a significant rate of morbidity and mortality. Current guidelines recommend the use of the Glasgow-Blatchford Score (GBS) to identify “very low risk” patients who would benefit from outpatient management rather than hospitalization. The use of scores has been previously proposed to help guide level of care upon admission, providing objectivity to support this decision, which presents an opportunity to improve patient outcomes and use of valuable resources.
Methods: Data obtained retrospectively from our community hospital revealed 329 admissions for UGIB within 2 years. The GBS was calculated for all patients and analyzed using logistic regression to numerically correlate for mortality rate, length of stay (LOS), and rate of upgrade to higher level of care (DOU/ICU) after admission. Afterwards, internal medicine physicians on the benefits of employing the GBS as a tool to guide safe disposition of patients admitted with UGIB. We suggested admission to the medical ward for patients with scores of 2-7, and to the DOU/ICU with a score of ≥8, or with severe hypotension on arrival. Repeat data was obtained 6 months after intervention and data from 84 admissions was reviewed.
Results: Initial analysis revealed a higher mortality, longer hospitalization, and more frequent upgrades to DOU/ICU among patients with a score ≥8, and patients with severe hypotension (defined as a mean arterial pressure [MAP] < 65 mmHg) on arrival, regardless of the score. Using these values as cutoff, more than half of these patients were admitted to the medical ward while meeting criteria for higher level of care. A root cause analysis revealed high variability in the criteria used to select the initial disposition, with a lack of objective data to support decision-making by admitting physicians. Reassessment 6 months after intervention revealed a statistically significant decrease in LOS and upgrade to DOU/ICU, with a non-significant trend towards decrease in mortality.
Discussion: By educating admitting physicians on the use of GBS as an objective tool to guide patient disposition, we were able to decrease length of hospitalization and preventable upgrades to higher level of care. Repeat data may support these findings and potentially reveal a statistically significant decrease in mortality as well.
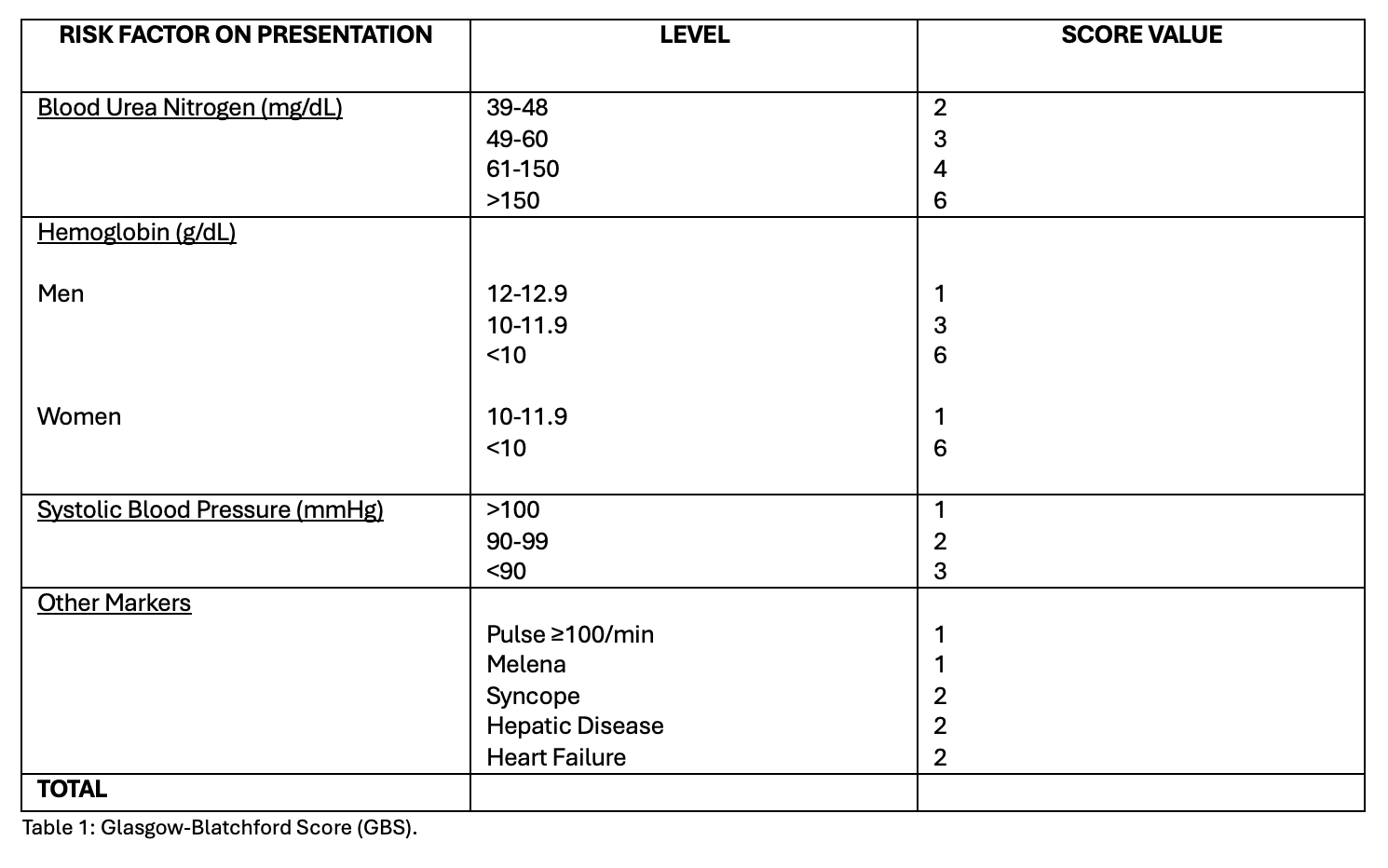
Figure: Table 1: Glasgow Blatchford Score (GBS).
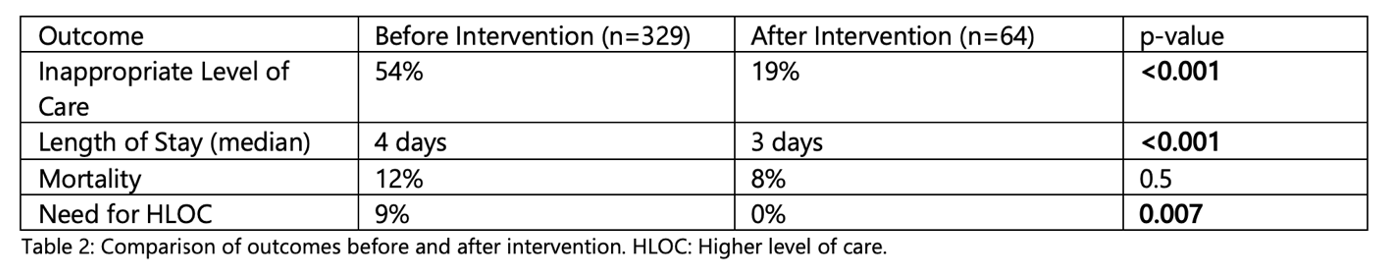
Figure: Table 2: Comparison of Outcomes Before and After Intervention. HLOC: Higher level of care.
Disclosures:
Jose Garcia-Corella indicated no relevant financial relationships.
Mahum Zahid indicated no relevant financial relationships.
Nihad Al-Yousfi indicated no relevant financial relationships.
Ikleel Moshref indicated no relevant financial relationships.
BreeAnna Carlson indicated no relevant financial relationships.
Nathan Lytton indicated no relevant financial relationships.
Leila Moosavi indicated no relevant financial relationships.
Igor Garcia-Pacheco indicated no relevant financial relationships.
Kasey Fox indicated no relevant financial relationships.
Jose Garcia-Corella, MD1, Mahum Zahid, MD2, Nihad Al-Yousfi, MD2, Ikleel Moshref, MD2, BreeAnna Carlson, DO3, Nathan Lytton, DO2, Leila Moosavi, MD4, Igor Garcia-Pacheco, MD2, Kasey Fox, DO2, 47, Utilization of the Glasgow-Blatchford Score to Guide Safe Disposition of Patients Admitted With Upper GI Bleeding: A Quality Improvement Research Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UCLA-Kern Medical Center, Bakersfield, CA; 2Kern Medical Center, Bakersfield, CA; 3Western University of Health Sciences, Bakersfield, CA; 4Adventist Hospital Bakersfield, Bakersfield, CA
Introduction: Upper gastrointestinal bleeding (UGIB) is the most frequent emergency reported in gastroenterology, with a significant rate of morbidity and mortality. Current guidelines recommend the use of the Glasgow-Blatchford Score (GBS) to identify “very low risk” patients who would benefit from outpatient management rather than hospitalization. The use of scores has been previously proposed to help guide level of care upon admission, providing objectivity to support this decision, which presents an opportunity to improve patient outcomes and use of valuable resources.
Methods: Data obtained retrospectively from our community hospital revealed 329 admissions for UGIB within 2 years. The GBS was calculated for all patients and analyzed using logistic regression to numerically correlate for mortality rate, length of stay (LOS), and rate of upgrade to higher level of care (DOU/ICU) after admission. Afterwards, internal medicine physicians on the benefits of employing the GBS as a tool to guide safe disposition of patients admitted with UGIB. We suggested admission to the medical ward for patients with scores of 2-7, and to the DOU/ICU with a score of ≥8, or with severe hypotension on arrival. Repeat data was obtained 6 months after intervention and data from 84 admissions was reviewed.
Results: Initial analysis revealed a higher mortality, longer hospitalization, and more frequent upgrades to DOU/ICU among patients with a score ≥8, and patients with severe hypotension (defined as a mean arterial pressure [MAP] < 65 mmHg) on arrival, regardless of the score. Using these values as cutoff, more than half of these patients were admitted to the medical ward while meeting criteria for higher level of care. A root cause analysis revealed high variability in the criteria used to select the initial disposition, with a lack of objective data to support decision-making by admitting physicians. Reassessment 6 months after intervention revealed a statistically significant decrease in LOS and upgrade to DOU/ICU, with a non-significant trend towards decrease in mortality.
Discussion: By educating admitting physicians on the use of GBS as an objective tool to guide patient disposition, we were able to decrease length of hospitalization and preventable upgrades to higher level of care. Repeat data may support these findings and potentially reveal a statistically significant decrease in mortality as well.
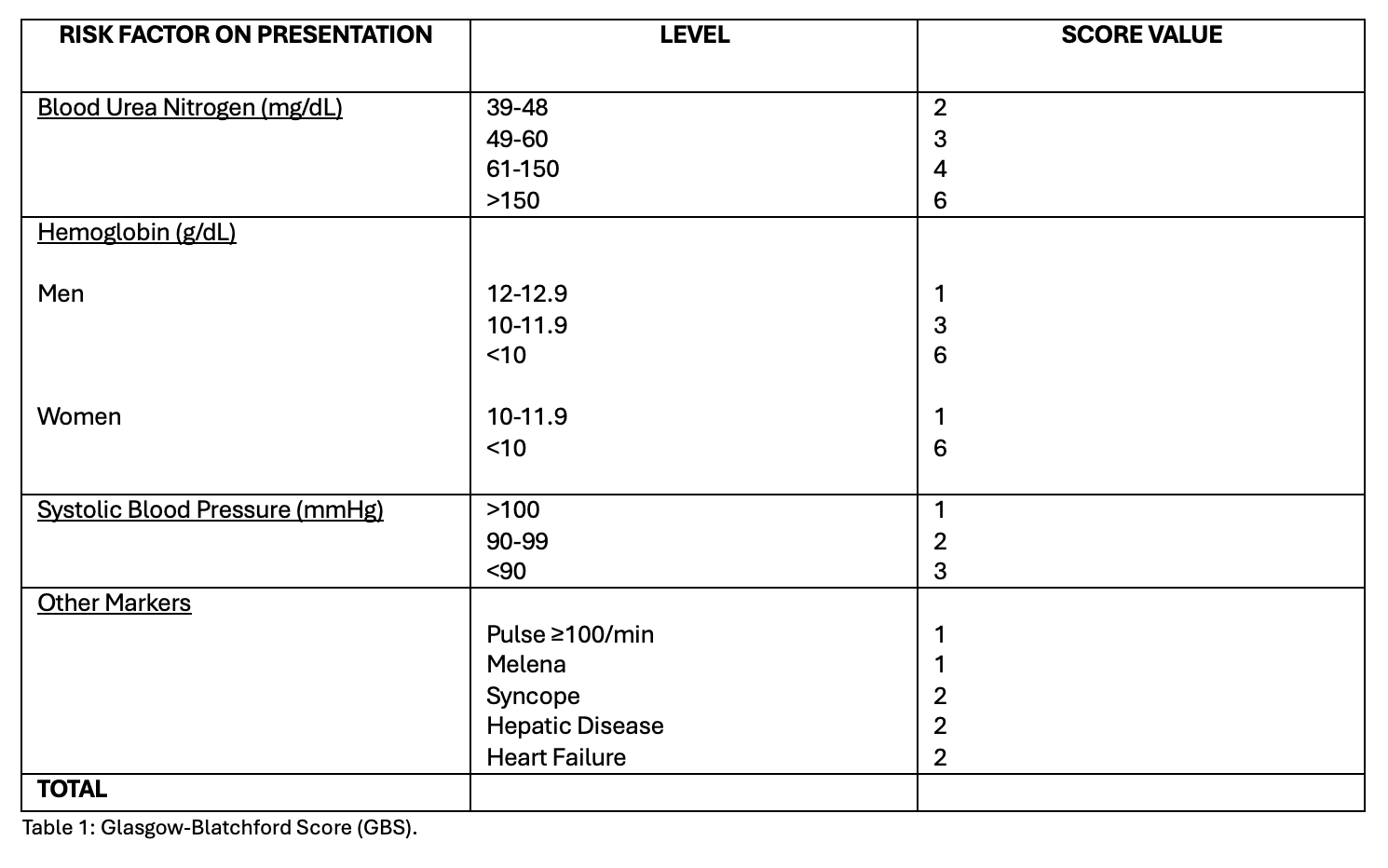
Figure: Table 1: Glasgow Blatchford Score (GBS).
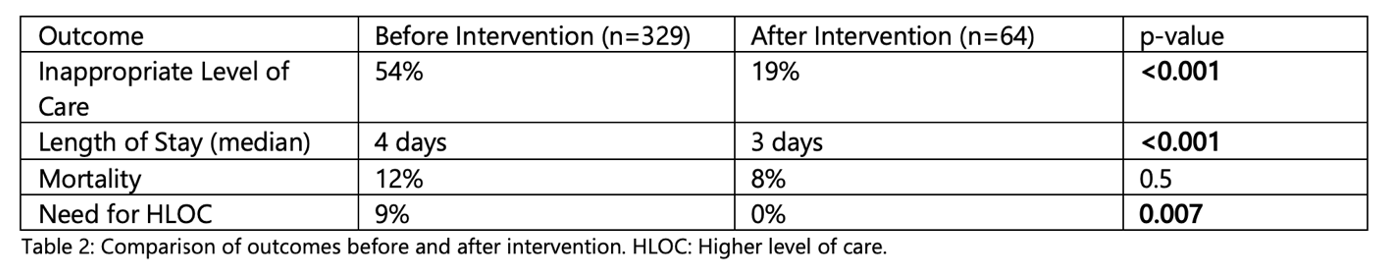
Figure: Table 2: Comparison of Outcomes Before and After Intervention. HLOC: Higher level of care.
Disclosures:
Jose Garcia-Corella indicated no relevant financial relationships.
Mahum Zahid indicated no relevant financial relationships.
Nihad Al-Yousfi indicated no relevant financial relationships.
Ikleel Moshref indicated no relevant financial relationships.
BreeAnna Carlson indicated no relevant financial relationships.
Nathan Lytton indicated no relevant financial relationships.
Leila Moosavi indicated no relevant financial relationships.
Igor Garcia-Pacheco indicated no relevant financial relationships.
Kasey Fox indicated no relevant financial relationships.
Jose Garcia-Corella, MD1, Mahum Zahid, MD2, Nihad Al-Yousfi, MD2, Ikleel Moshref, MD2, BreeAnna Carlson, DO3, Nathan Lytton, DO2, Leila Moosavi, MD4, Igor Garcia-Pacheco, MD2, Kasey Fox, DO2, 47, Utilization of the Glasgow-Blatchford Score to Guide Safe Disposition of Patients Admitted With Upper GI Bleeding: A Quality Improvement Research Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

