Tuesday Poster Session
Category: Liver
P5791 - Clostridioides difficile Infection and Risk of Spontaneous Bacterial Peritonitis in Liver Cirrhosis: A Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Edgar M. Luna Landa, MD
Texas Tech University Health Sciences Center
Odessa, TX
Presenting Author(s)
Edgar M. Luna Landa, MD1, Melina Arroyo Cisneros, 2, Chun Ho Szeto, MD, MPH1, Guy Loic Nguefang Tchoukeu, MD1, Anjul Verma, MD1, Gloria Erazo, MD1, Godfrey Tabowei, MD3, Jorge Rodriguez, MD4
1Texas Tech University Health Sciences Center, Odessa, TX; 2Independent Statistician, Odessa, TX; 3Texas Tech University Health Science center, Permian Basin, Odessa, TX; 4Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX
Introduction: Clostridioides difficile infection (CDI) and Spontaneous Bacterial Peritonitis (SBP) cause significant morbidity and mortality in patients with Liver Cirrhosis. Both infections are well studied, however, the potential role of CDI in precipitating SBP remains unclear. We aimed to evaluate whether CDI is associated with a higher risk of SBP and worse clinical outcomes in patients with liver cirrhosis.
Methods: We used the MIMIC-IV V3.1 database to identify hospital admissions in adults aged ≥18 years with liver cirrhosis between 2008-2022. Liver Cirrhosis was defined using ICD-9 and ICD-10-based taxonomy. CDI was identified using ICD-9 codes 00845 and ICD-10 codes A047. SBP was defined using ICD-9 code 56723 and ICD-10 code K652. Secondary outcomes included In-hospital and ICU mortality, ICU admission, and Hospital and ICU length of stay (LOS). Multivariable Firth logistic regression was used to estimate adjusted odds ratios (aORs), reduce small-sample bias and address separation issues. A linear regression model was used for continuous outcomes. Our models were adjusted for age group, gender, Meld score ≥15, and Charlson Comorbidity index. We included an interaction term for CDI x Meld score ≥15. Descriptive statistics and chi-square tests were used to compare baseline characteristics.
Results: Of the 23,393 patients with liver cirrhosis, 2.7% had CDI, and 5% had spontaneous bacterial peritonitis (SBP). In our unadjusted analysis, CDI was associated with higher SBP incidence (OR 1.79, p< 0.001). After adjustment, CDI remained independently associated with SBP (Adjusted Odds Ratio [aOR] 1.37 [95% CI 1.02-1.82]). CDI was associated with higher In-Hospital mortality (aOR 1.97 [95% CI 1.13-3.20]), with a remarkable interaction indicating a reduced effect in mortality in patients with MELD ≥15 (interaction aOR: 0.51 [95% CI 0.29–0.95]), possibly due to a higher baseline mortality risk. CDI was associated with higher odds of ICU admission (aOR 1.92 [95% CI 1.45-2.5]) and increased hospital LOS of 5.7 days, p < 0.001). Additionally, ICU mortality and ICU length of stay were not significantly associated with CDI.
Discussion: CDI significantly increases the risk of SBP, in-hospital mortality, ICU admission, and prolonged hospital stay in patients with liver cirrhosis. Remarkably mortality was higher in patients with lower MELD scores, suggesting a possible ceiling effect. Due to a small sample size, larger datasets studies may be needed to improve statistical power and validate these findings.
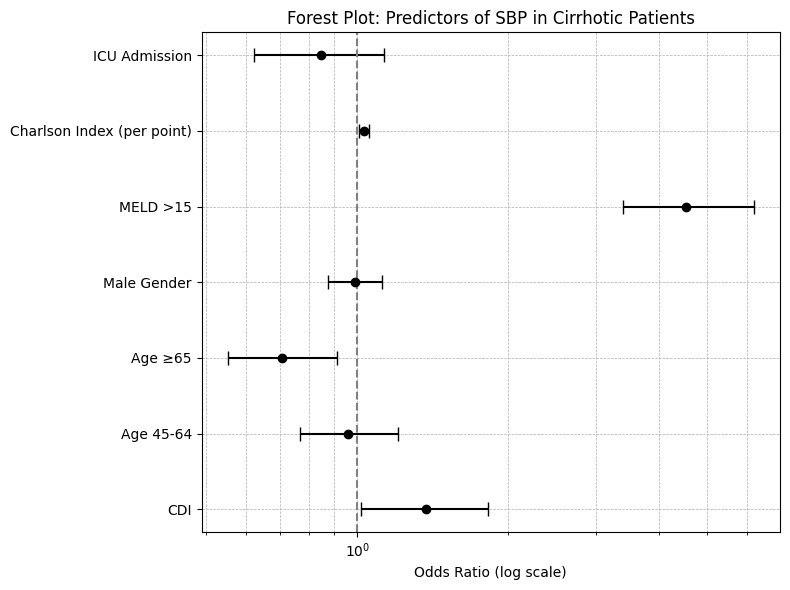
Figure: Forest plot showing adjusted predictors of spontaneous bacterial peritonitis in hospitalized patients with liver cirrhosis. Odds ratios (ORs) with 95% confidence intervals (CIs) are shown on a log scale. CDI and MELD scores >15 were independently associated with increased odds of SBP.
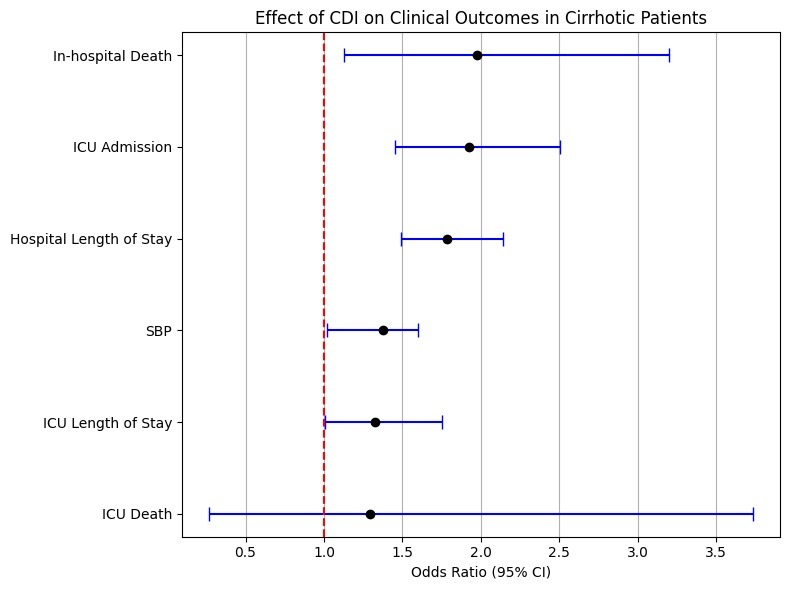
Figure: Effect of Clostridioides difficile infection on clinical outcomes in cirrhotic patients. Adjusted odds ratios (aORs) with 95% confidence intervals are shown for each outcome. CDI was associated with a significantly increased risk of in-hospital mortality, ICU admission, SBP, and hospital length of stay.
Disclosures:
Edgar Luna Landa indicated no relevant financial relationships.
Melina Arroyo Cisneros indicated no relevant financial relationships.
Chun Ho Szeto indicated no relevant financial relationships.
Guy Loic Nguefang Tchoukeu indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Gloria Erazo indicated no relevant financial relationships.
Godfrey Tabowei indicated no relevant financial relationships.
Jorge Rodriguez indicated no relevant financial relationships.
Edgar M. Luna Landa, MD1, Melina Arroyo Cisneros, 2, Chun Ho Szeto, MD, MPH1, Guy Loic Nguefang Tchoukeu, MD1, Anjul Verma, MD1, Gloria Erazo, MD1, Godfrey Tabowei, MD3, Jorge Rodriguez, MD4. P5791 - Clostridioides difficile Infection and Risk of Spontaneous Bacterial Peritonitis in Liver Cirrhosis: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Odessa, TX; 2Independent Statistician, Odessa, TX; 3Texas Tech University Health Science center, Permian Basin, Odessa, TX; 4Texas Tech University Health Sciences Center - Permian Basin, Odessa, TX
Introduction: Clostridioides difficile infection (CDI) and Spontaneous Bacterial Peritonitis (SBP) cause significant morbidity and mortality in patients with Liver Cirrhosis. Both infections are well studied, however, the potential role of CDI in precipitating SBP remains unclear. We aimed to evaluate whether CDI is associated with a higher risk of SBP and worse clinical outcomes in patients with liver cirrhosis.
Methods: We used the MIMIC-IV V3.1 database to identify hospital admissions in adults aged ≥18 years with liver cirrhosis between 2008-2022. Liver Cirrhosis was defined using ICD-9 and ICD-10-based taxonomy. CDI was identified using ICD-9 codes 00845 and ICD-10 codes A047. SBP was defined using ICD-9 code 56723 and ICD-10 code K652. Secondary outcomes included In-hospital and ICU mortality, ICU admission, and Hospital and ICU length of stay (LOS). Multivariable Firth logistic regression was used to estimate adjusted odds ratios (aORs), reduce small-sample bias and address separation issues. A linear regression model was used for continuous outcomes. Our models were adjusted for age group, gender, Meld score ≥15, and Charlson Comorbidity index. We included an interaction term for CDI x Meld score ≥15. Descriptive statistics and chi-square tests were used to compare baseline characteristics.
Results: Of the 23,393 patients with liver cirrhosis, 2.7% had CDI, and 5% had spontaneous bacterial peritonitis (SBP). In our unadjusted analysis, CDI was associated with higher SBP incidence (OR 1.79, p< 0.001). After adjustment, CDI remained independently associated with SBP (Adjusted Odds Ratio [aOR] 1.37 [95% CI 1.02-1.82]). CDI was associated with higher In-Hospital mortality (aOR 1.97 [95% CI 1.13-3.20]), with a remarkable interaction indicating a reduced effect in mortality in patients with MELD ≥15 (interaction aOR: 0.51 [95% CI 0.29–0.95]), possibly due to a higher baseline mortality risk. CDI was associated with higher odds of ICU admission (aOR 1.92 [95% CI 1.45-2.5]) and increased hospital LOS of 5.7 days, p < 0.001). Additionally, ICU mortality and ICU length of stay were not significantly associated with CDI.
Discussion: CDI significantly increases the risk of SBP, in-hospital mortality, ICU admission, and prolonged hospital stay in patients with liver cirrhosis. Remarkably mortality was higher in patients with lower MELD scores, suggesting a possible ceiling effect. Due to a small sample size, larger datasets studies may be needed to improve statistical power and validate these findings.
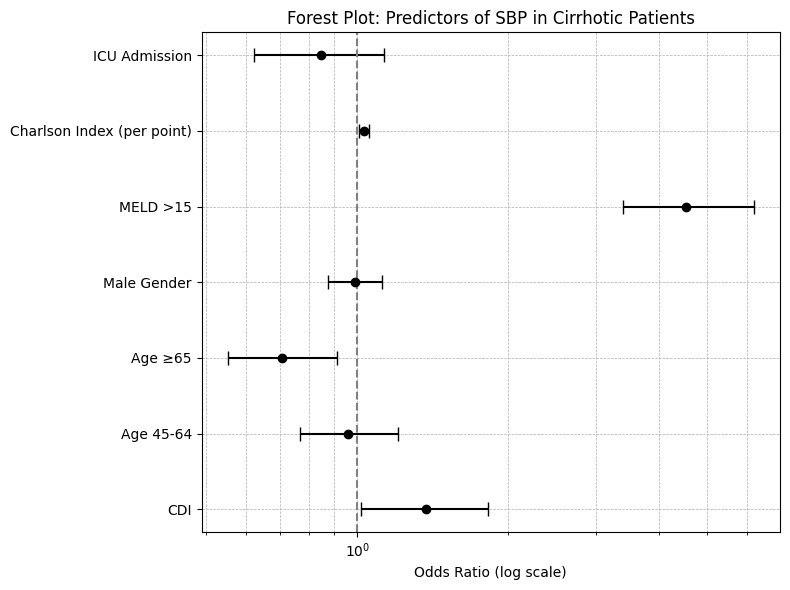
Figure: Forest plot showing adjusted predictors of spontaneous bacterial peritonitis in hospitalized patients with liver cirrhosis. Odds ratios (ORs) with 95% confidence intervals (CIs) are shown on a log scale. CDI and MELD scores >15 were independently associated with increased odds of SBP.
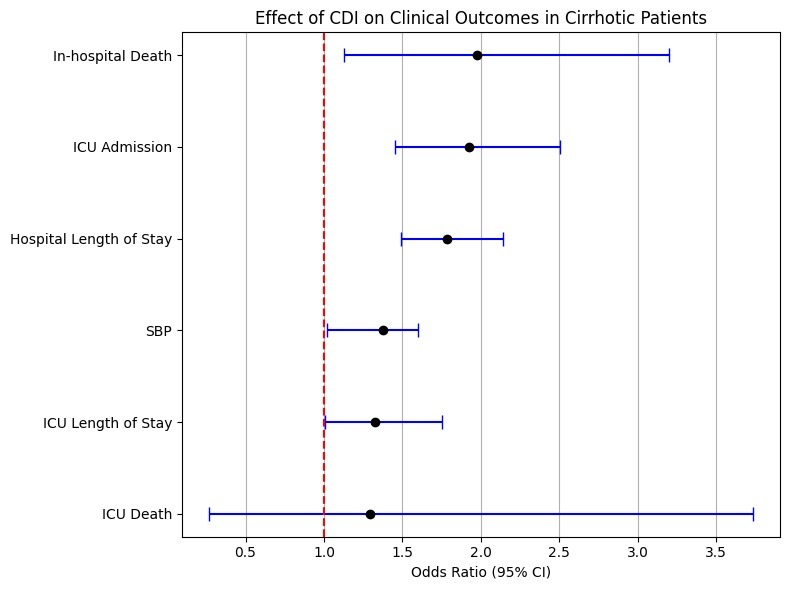
Figure: Effect of Clostridioides difficile infection on clinical outcomes in cirrhotic patients. Adjusted odds ratios (aORs) with 95% confidence intervals are shown for each outcome. CDI was associated with a significantly increased risk of in-hospital mortality, ICU admission, SBP, and hospital length of stay.
Disclosures:
Edgar Luna Landa indicated no relevant financial relationships.
Melina Arroyo Cisneros indicated no relevant financial relationships.
Chun Ho Szeto indicated no relevant financial relationships.
Guy Loic Nguefang Tchoukeu indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Gloria Erazo indicated no relevant financial relationships.
Godfrey Tabowei indicated no relevant financial relationships.
Jorge Rodriguez indicated no relevant financial relationships.
Edgar M. Luna Landa, MD1, Melina Arroyo Cisneros, 2, Chun Ho Szeto, MD, MPH1, Guy Loic Nguefang Tchoukeu, MD1, Anjul Verma, MD1, Gloria Erazo, MD1, Godfrey Tabowei, MD3, Jorge Rodriguez, MD4. P5791 - Clostridioides difficile Infection and Risk of Spontaneous Bacterial Peritonitis in Liver Cirrhosis: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

