Tuesday Poster Session
Category: Liver
P6051 - Segmental Atrophy of the Liver: A Rare, Often Misdiagnosed Pseudotumor
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Swetha Tummala, MD
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Swetha Tummala, MD1, Natalie Patel, MD2, Sanjeev Tummala, MD3
1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Peninsula Pathologists Medical Group, San Francisco, CA; 3Palo Alto Medical Foundation, Mountain View, CA
Introduction: Segmental atrophy of the liver is a rare, often misdiagnosed pseudotumor that can lead to unnecessary surgical intervention. We describe a case of a sixty-five-year-old male with an incidentally found hepatic mass with biopsy showing key histological features of segmental atrophy of the liver that guided conservative management.
Case Description/
Methods: A sixty-five-year-old male with a history of hypertension, atrial fibrillation, and nephrolithiasis presented to the emergency department with acute, upper abdomen and left flank pain and blood in the urine. The patient does not smoke or drink. He has no family history of liver disease or cancer. Vitals, physical exam, complete blood count, and liver function tests were normal. A urinalysis showed blood. A CT scan of the abdomen showed a two millimeter left mid-lumbar ureter stone with minimal hydronephrosis. Incidentally, a 5.9 centimeter solid lesion was noted in the right hepatic dome. The patient’s symptoms resolved with pain medications. He had a follow-up triphasic CT scan of the abdomen that showed a heterogeneous, exophytic, solid 5.7 centimeter mass in the posterior dome of the liver (Figure 1) which was atypical for hemangioma. A targeted liver biopsy showed loss of hepatic parenchyma with marked elastotic to sclerotic stroma with intermixed abnormal blood vessels and mild inflammation, consistent with late stages of segmental atrophy (Figure 2). No malignancy was identified. Since the patient was asymptomatic, the patient is being followed conservatively.
Discussion: Segmental atrophy of the liver is rare and often misdiagnosed due to the wide variability of histological changes. These include hepatic inflammation, loss of hepatic parenchyma, bile duct proliferation, biliary cysts, and elastotic and fibrotic changes. There are three stages based on the extent of elastosis/fibrosis. Early lesions have minimal elastosis. They are characterized by collapsed parenchyma. Advanced lesions have more elastosis. End-stage lesions appear as a fibrotic mass. Segmental atrophy of the liver is often misdiagnosed as sclerosing cavernous hemangioma, hydatid cyst, cirrhosis, hepatocellular carcinoma, and cholangiocarcinoma, frequently leading to surgery. This case highlights key histological features of segmental atrophy of the liver. Though malignancy is on the differential, we hope that this case raises awareness among clinicians for segmental atrophy of the liver as a probable diagnosis to help prevent unnecessary surgical intervention.
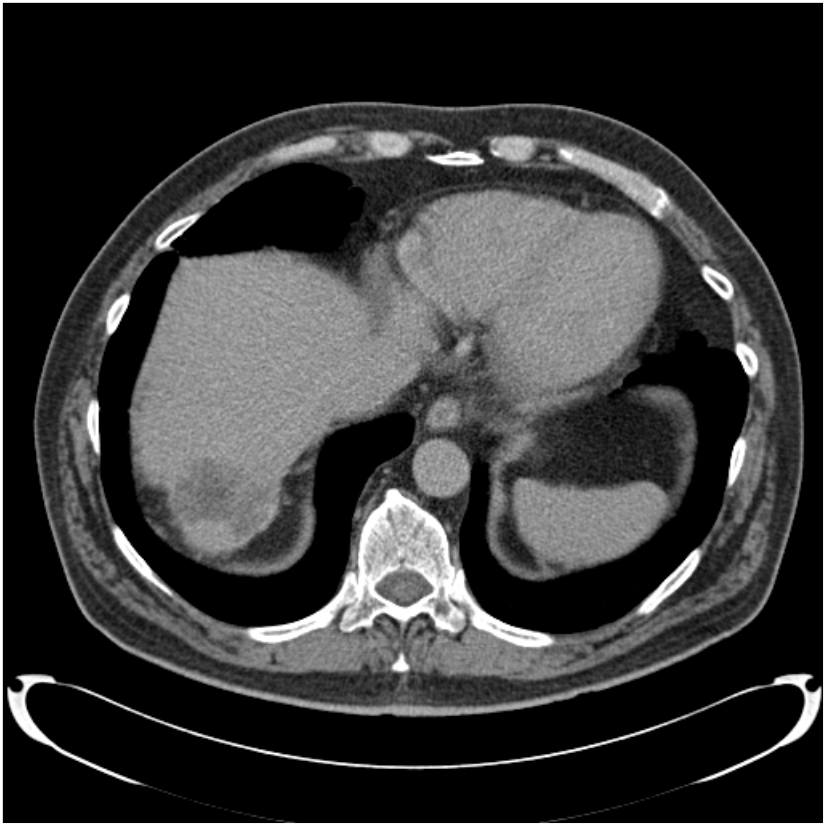
Figure: CT scan showing heterogeneous, partially exophytic, solid 5.7 cm mass in the posterior dome of the liver.
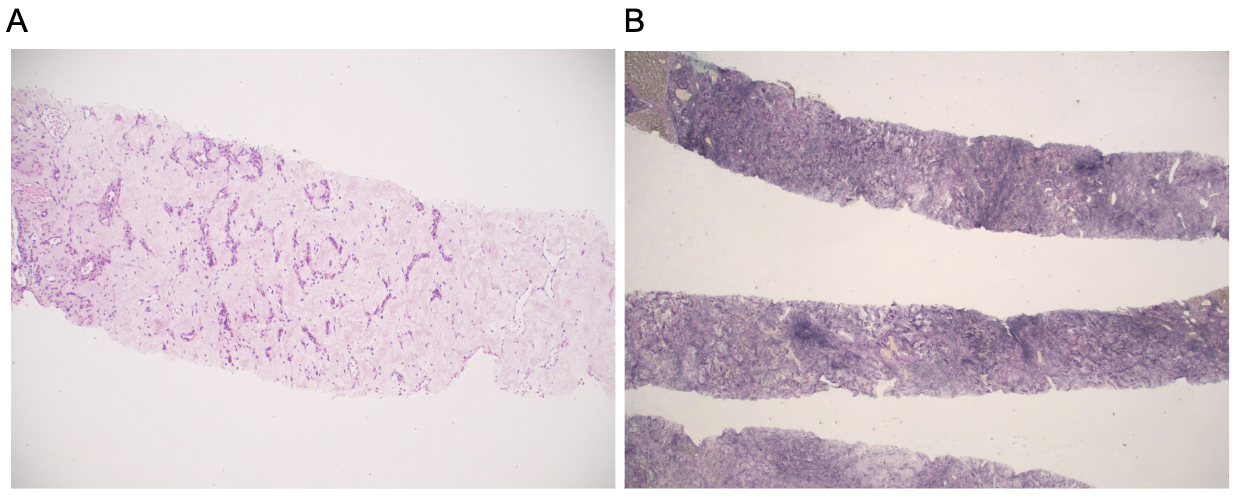
Figure: Picture of a liver biopsy at 10x magnification on H&E slide (A) with a markedly sclerotic to elastotic stroma with intermixed thin walled blood vessels and abnormal thick walled blood vessels. Increased stromal elastosis is highlighted with elastin special stain (B).
Disclosures:
Swetha Tummala indicated no relevant financial relationships.
Natalie Patel indicated no relevant financial relationships.
Sanjeev Tummala indicated no relevant financial relationships.
Swetha Tummala, MD1, Natalie Patel, MD2, Sanjeev Tummala, MD3. P6051 - Segmental Atrophy of the Liver: A Rare, Often Misdiagnosed Pseudotumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Peninsula Pathologists Medical Group, San Francisco, CA; 3Palo Alto Medical Foundation, Mountain View, CA
Introduction: Segmental atrophy of the liver is a rare, often misdiagnosed pseudotumor that can lead to unnecessary surgical intervention. We describe a case of a sixty-five-year-old male with an incidentally found hepatic mass with biopsy showing key histological features of segmental atrophy of the liver that guided conservative management.
Case Description/
Methods: A sixty-five-year-old male with a history of hypertension, atrial fibrillation, and nephrolithiasis presented to the emergency department with acute, upper abdomen and left flank pain and blood in the urine. The patient does not smoke or drink. He has no family history of liver disease or cancer. Vitals, physical exam, complete blood count, and liver function tests were normal. A urinalysis showed blood. A CT scan of the abdomen showed a two millimeter left mid-lumbar ureter stone with minimal hydronephrosis. Incidentally, a 5.9 centimeter solid lesion was noted in the right hepatic dome. The patient’s symptoms resolved with pain medications. He had a follow-up triphasic CT scan of the abdomen that showed a heterogeneous, exophytic, solid 5.7 centimeter mass in the posterior dome of the liver (Figure 1) which was atypical for hemangioma. A targeted liver biopsy showed loss of hepatic parenchyma with marked elastotic to sclerotic stroma with intermixed abnormal blood vessels and mild inflammation, consistent with late stages of segmental atrophy (Figure 2). No malignancy was identified. Since the patient was asymptomatic, the patient is being followed conservatively.
Discussion: Segmental atrophy of the liver is rare and often misdiagnosed due to the wide variability of histological changes. These include hepatic inflammation, loss of hepatic parenchyma, bile duct proliferation, biliary cysts, and elastotic and fibrotic changes. There are three stages based on the extent of elastosis/fibrosis. Early lesions have minimal elastosis. They are characterized by collapsed parenchyma. Advanced lesions have more elastosis. End-stage lesions appear as a fibrotic mass. Segmental atrophy of the liver is often misdiagnosed as sclerosing cavernous hemangioma, hydatid cyst, cirrhosis, hepatocellular carcinoma, and cholangiocarcinoma, frequently leading to surgery. This case highlights key histological features of segmental atrophy of the liver. Though malignancy is on the differential, we hope that this case raises awareness among clinicians for segmental atrophy of the liver as a probable diagnosis to help prevent unnecessary surgical intervention.
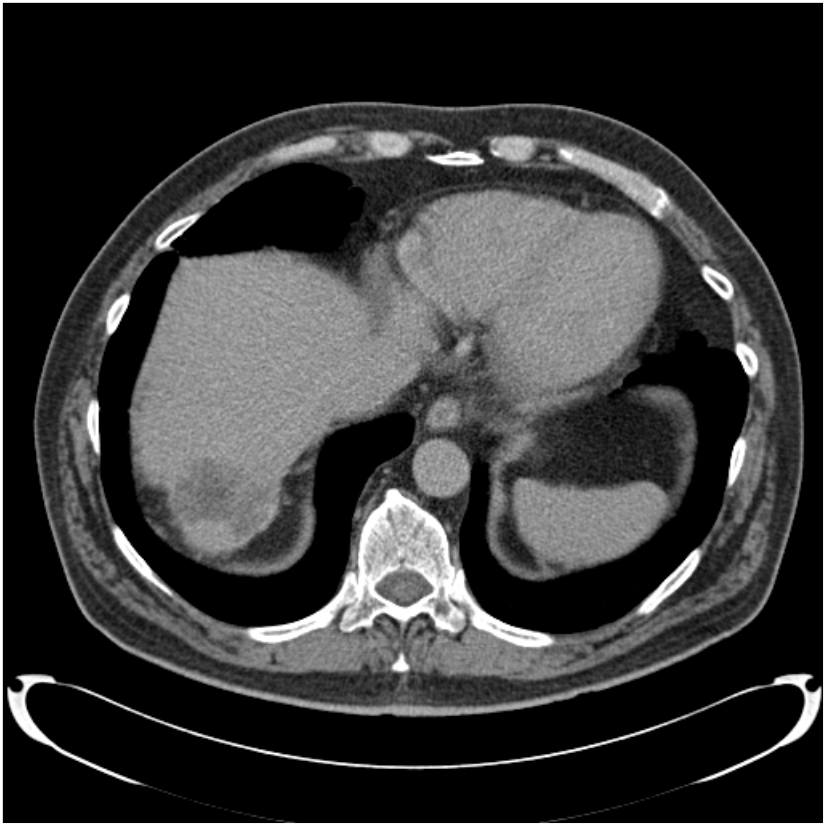
Figure: CT scan showing heterogeneous, partially exophytic, solid 5.7 cm mass in the posterior dome of the liver.
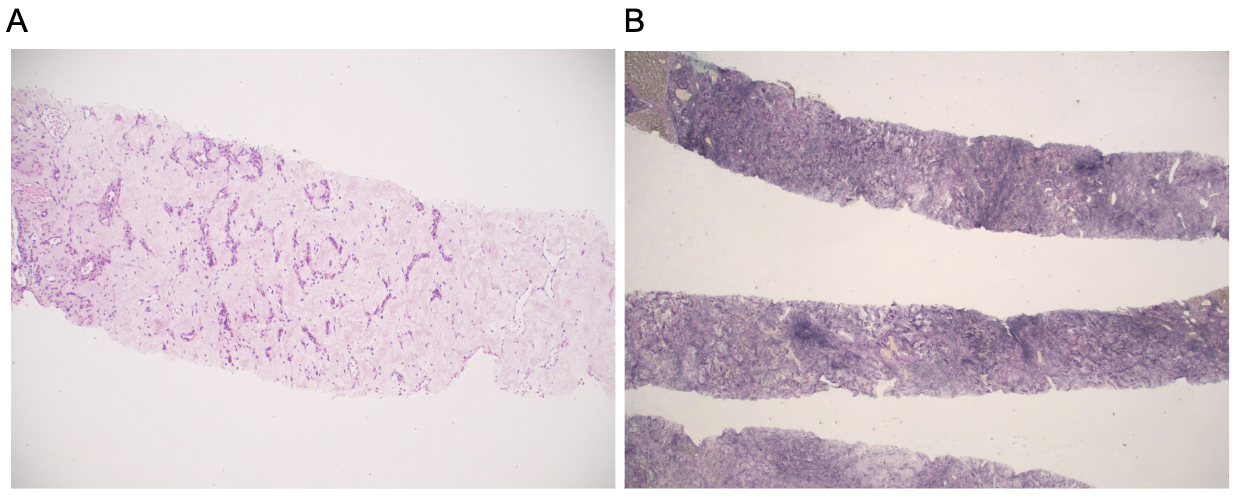
Figure: Picture of a liver biopsy at 10x magnification on H&E slide (A) with a markedly sclerotic to elastotic stroma with intermixed thin walled blood vessels and abnormal thick walled blood vessels. Increased stromal elastosis is highlighted with elastin special stain (B).
Disclosures:
Swetha Tummala indicated no relevant financial relationships.
Natalie Patel indicated no relevant financial relationships.
Sanjeev Tummala indicated no relevant financial relationships.
Swetha Tummala, MD1, Natalie Patel, MD2, Sanjeev Tummala, MD3. P6051 - Segmental Atrophy of the Liver: A Rare, Often Misdiagnosed Pseudotumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
