Sunday Poster Session
Category: Colon
P0265 - The Effects of Pelvic Radiation on Ileal-Anal Pouches: A Systematic Review and Meta-Analysis
- SQ
Stephanie Quon, BASc (she/her/hers)
University of British Columbia
Vancouver, BC, Canada
Presenting Author(s)
1University of British Columbia, Vancouver, BC, Canada; 2University of British Columbia Department of Medicine, Surrey, BC, Canada; 3UBC Department of Medicine/IBD Centre of BC, Vancouver, BC, Canada
Introduction:
Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the gold-standard surgical treatment for ulcerative colitis and familial adenomatous polyposis. While IPAA preserves continence and avoids a permanent stoma, it carries risks such as pouchitis and pouch failure. Pelvic radiation, used for co-existing malignancies, has been associated with pouch complications, yet existing guidance is limited. This review synthesized evidence on the effects of pelvic radiation in patients with IPAA.
Methods:
This PRISMA-guided systematic review searched PubMed, Embase, and Scopus in February 2025 for studies from January 2000 onward on IPAA patients exposed to pelvic radiation reporting ≥1 pouch-related outcome. English, peer-reviewed studies, including cohort, case-control, and case series, were included. Abstracts, reviews, and non-original data were excluded. One reviewer screened and extracted data. A meta-analysis assessed heterogeneity and radiation type (external beam or brachytherapy, before or after IPAA) as a moderator of pouchitis risk.
Results: Twelve studies (2004-2024) met inclusion criteria, consisting of 101 patients who underwent IPAA and pelvic radiation (83 external beam, 18 brachytherapy). The mean patient age was 57.8 years, with an average follow-up of 58.8 months. Radiation was most commonly administered for anorectal (n=35) and prostate cancers (n=29). Overall, 28% of patients developed pouchitis (95% CI: 24-34%), though attribution to radiation is limited by lack of control groups. Complications were more common when radiation was delivered after IPAA compared to before (pouchitis: 53.7% vs. 7.7%; pouch failure: 39.0% vs. 3.8%). Brachytherapy was associated with lower rates of pouchitis (16.7% vs. 25.3%) and pouch failure (11.1% vs. 18.1%) compared to external beam. A random-effects meta-analysis revealed moderate heterogeneity (I²=26.2%), and meta-regression showed no significant difference in pouchitis rates by radiation type (p=0.372). A funnel plot showed no major publication bias.
Discussion:
Pelvic radiation in patients with IPAA is associated with adverse pouch outcomes. This review found that pouchitis and pouch failure were more common with radiotherapy given after IPAA than before. While brachytherapy showed lower complication rates than external beam, differences were not statistically significant. These findings highlight the need for individualized decision-making and further research to guide radiation planning in patients with IPAA.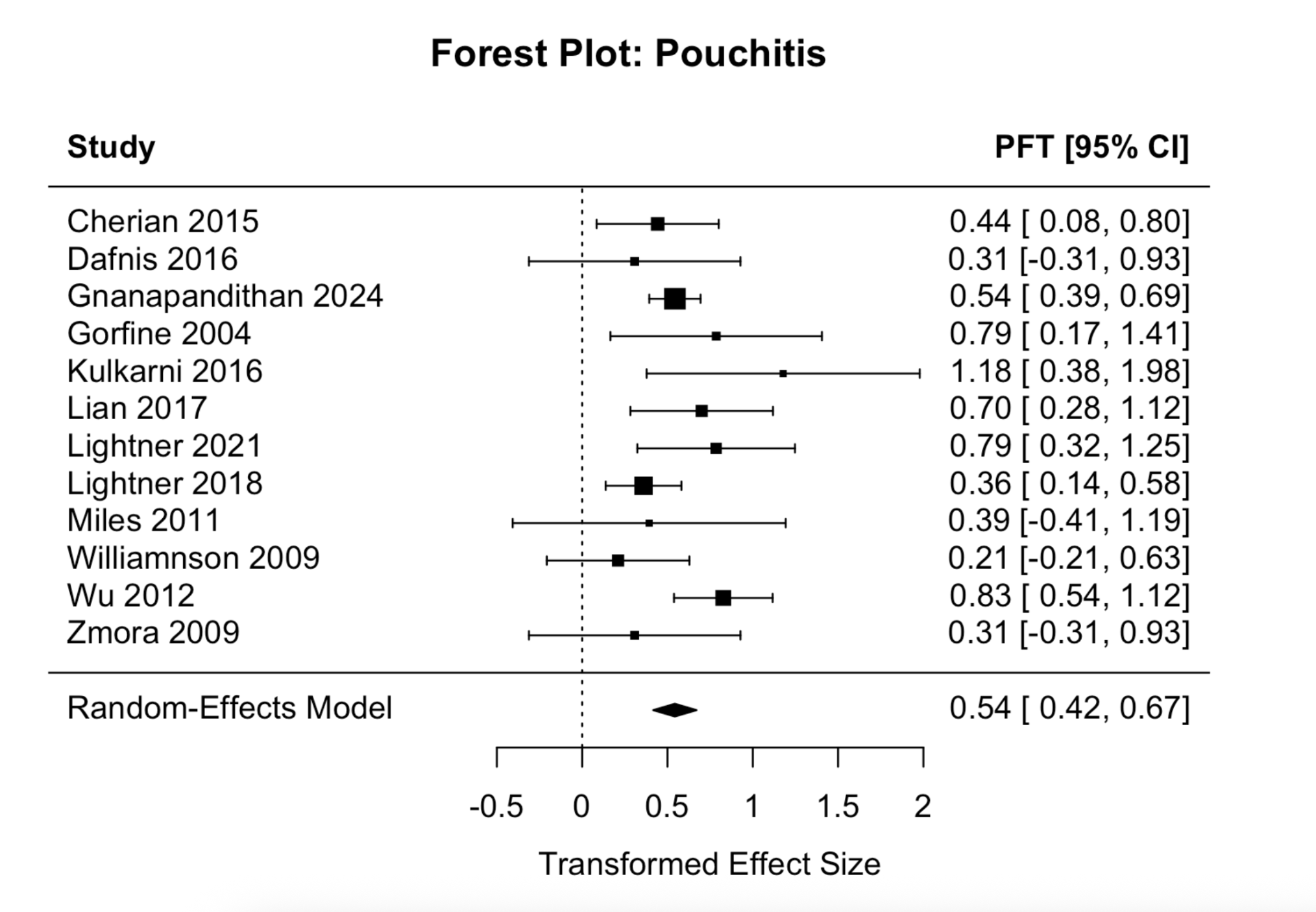
Figure: Figure 1: Forest plot of pouchitis rates among patients undergoing pelvic radiation. Individual study estimates are presented using Freeman-Tukey transformed proportions with 95% confidence intervals.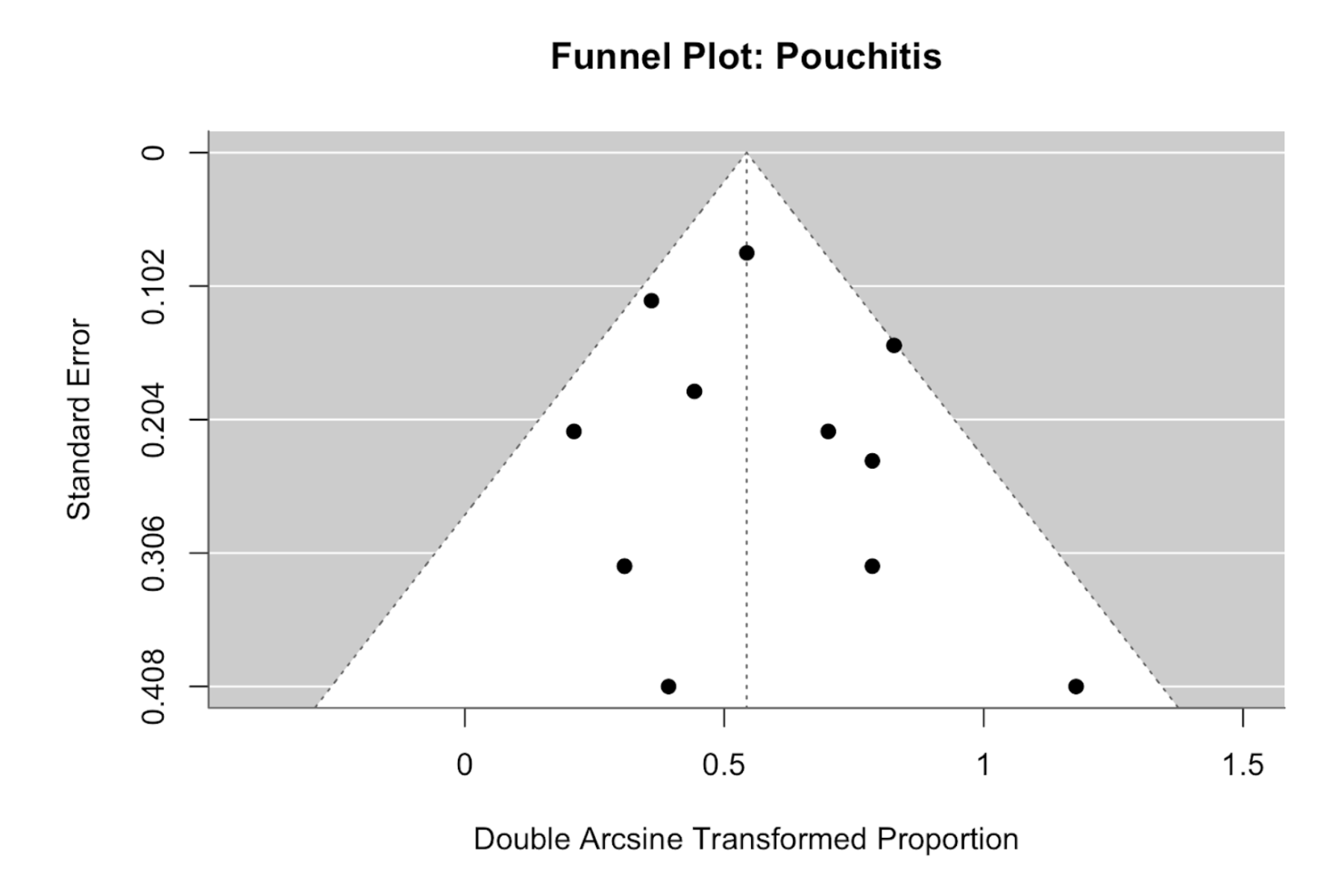
Figure: Figure 2: Funnel plot assessing potential publication bias in studies reporting pouchitis rates. Each dot represents a study, plotted against its standard error and Freeman-Tukey transformed proportion. The symmetry of the distribution suggests no substantial small-study or publication bias.
Disclosures:
Stephanie Quon indicated no relevant financial relationships.
Bachviet Nguyen indicated no relevant financial relationships.
Astrid-Jane Williams indicated no relevant financial relationships.
Stephanie Quon, BASc1, Bachviet AH. Nguyen, MD2, Astrid-Jane Williams, MD3. P0265 - The Effects of Pelvic Radiation on Ileal-Anal Pouches: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
