Monday Poster Session
Category: GI Bleeding
P3078 - Clinical Outcomes in Patients With Iron Deficiency Anemia After a Severe Gastrointestinal Hemorrhage From Different Types of Gastrointestinal Lesions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Peerapol Wangrattanapranee, MD (he/him/his)
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Peerapol Wangrattanapranee, MD1, Dennis M.. Jensen, MD2, Usah Dutson, MD, MPH2, Mary Ellen Jensen, MLS2
1University of California Riverside School of Medicine, Riverside, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA
Introduction: Iron deficiency anemia (IDA) is often underrecognized in patients after a severe gastrointestinal (GI) hemorrhage (GIH). For patients with severe GIH, our aims were to compare rates of diagnosis and treatment of IDA and clinical outcomes of 3 subgroups of GIH: portal hypertension (PH) lesions (varices and PH gastropathy), acute on chronic anemia (ACA) from angioma syndromes, or IDA with acute GIH from focal lesions with arteries.
Methods: This is a retrospective analysis of prospectively collected data of patients hospitalized with severe GIH. Severe GIH was defined as acute GIH with drop of Hb ≥ 2g/dL or 1 unit of packed red blood cell transfusion. IDA was defined as serum iron < 50 mcg/dL, ferritin < 30 ng/mL, and transferrin saturation < 20%. Bivariate and multivariate analyses were used to compare clinical characteristics and outcomes. P-value < 0.05 was statistically significant.
Results: Table 1 lists the number and types of UGI and colon lesions by subgroups. There were significant differences in age, gender, race. Cardiovascular diseases (CVD) were significantly more prevalent in the ACA group and liver diseases more common in the variceal/PHG group. Rates of testing for IDA ranged from 42% to 59% - Table 2. For those tested, documented IDA prevalence was high, ranging from 72.2% to 84.6%. There were significant differences in the rates of iron treatment in the 3 groups: 59% in ACA, 36% in acute severe GIH, and 19% in variceal/PHG group – Table 2. For adjusted analysis using the acute severe GIH as reference group, the odds of iron treatment were lower in the variceal/PHG group (OR 0.25, p=0.001) but higher in the ACA group (OR 2.44, p=0.046). As shown in Table 2, both the number of severe clinical outcomes and the composite outcome score were significantly lower in the acute severe GIH group indicating better results than the other two subgroups.
Discussion: 1) 84.6% of patients with ACA had IDA and most received iron treatment but still had poor outcomes, 2) Patients with varices/PHG hemorrhage had the lowest rates of iron testing and treatment. 3) 51% of patients with acute severe GIH were tested for and 72.2% had IDA, 36% received iron, and they had the best clinical outcomes. 4) Further interventional studies should focus on diagnosis of IDA and treatment of IDA patients with acute severe GIH from focal lesions with arteries because they are most likely to benefit and not the other 2 subgroups.
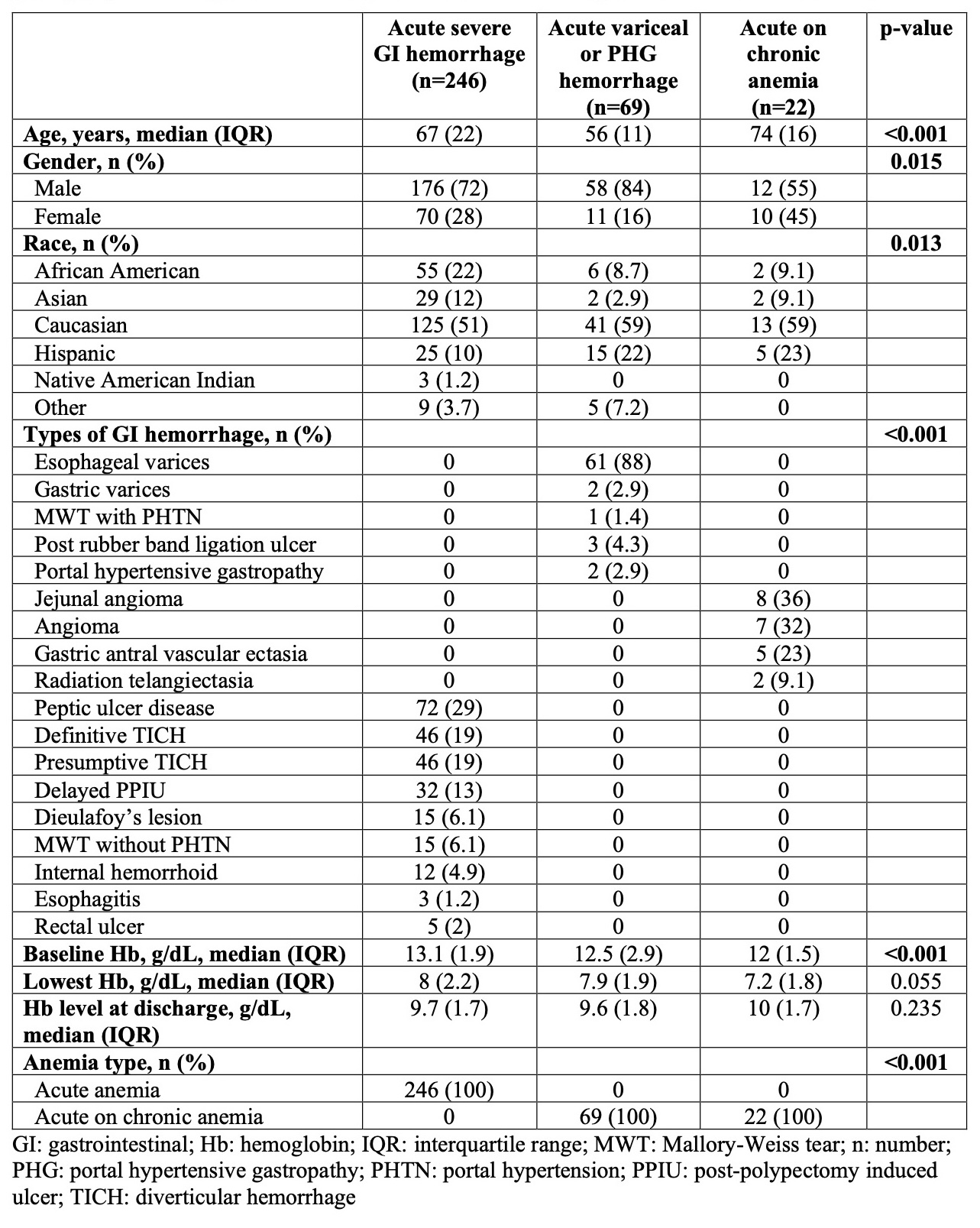
Figure: Table 1. Bivariate comparison of baseline characteristics of acute variceal or portal hypertensive gastropathy hemorrhage, acute severe gastrointestinal hemorrhage, or acute on chronic anemia
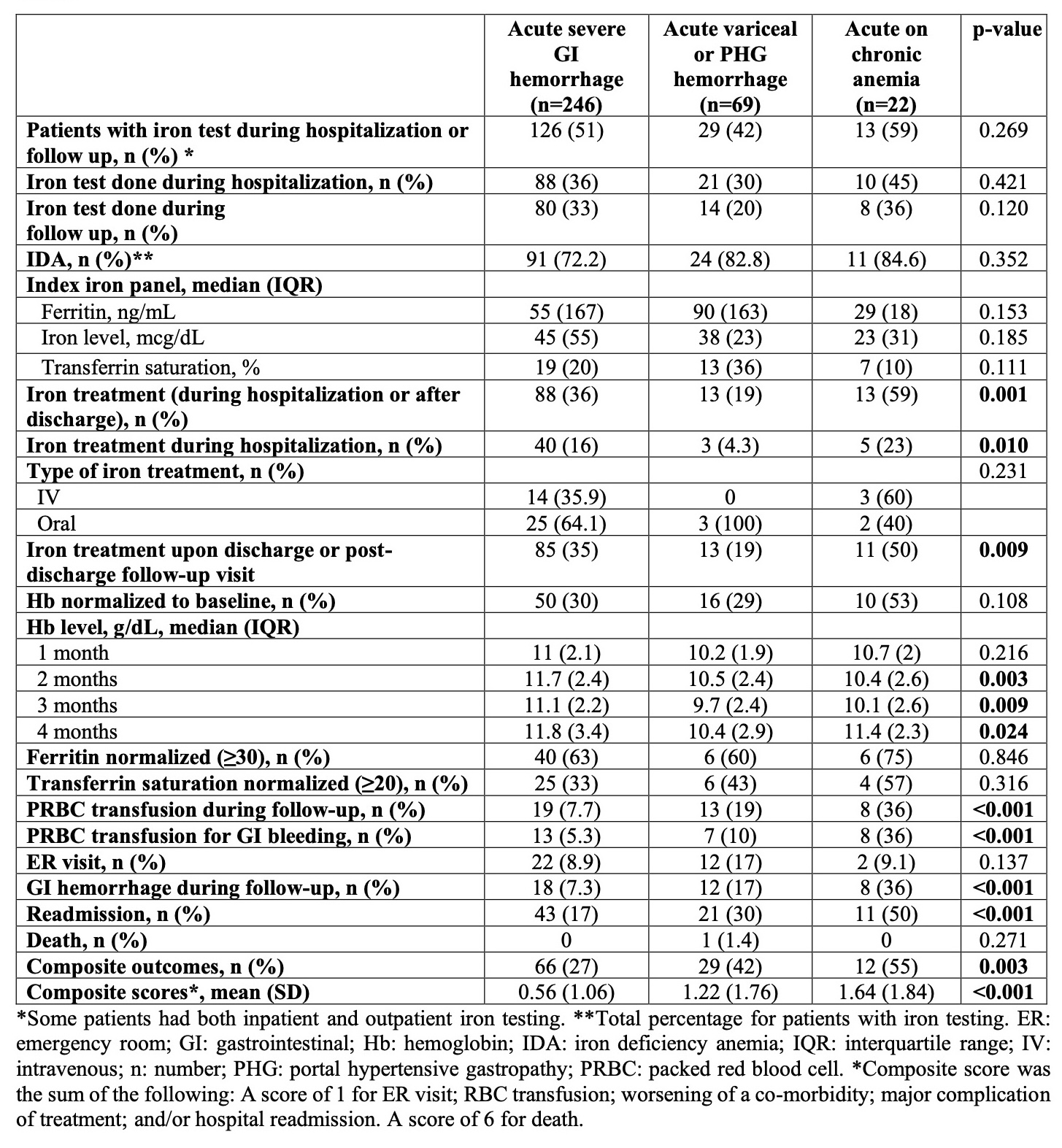
Figure: Table 2. Bivariate comparison of diagnosis and treatment of iron deficiency anemia and clinical outcomes of acute variceal or portal hypertensive gastropathy hemorrhage, acute severe gastrointestinal hemorrhage, or acute on chronic anemia
Disclosures:
Peerapol Wangrattanapranee indicated no relevant financial relationships.
Dennis Jensen indicated no relevant financial relationships.
Usah Dutson indicated no relevant financial relationships.
Mary Ellen Jensen indicated no relevant financial relationships.
Peerapol Wangrattanapranee, MD1, Dennis M.. Jensen, MD2, Usah Dutson, MD, MPH2, Mary Ellen Jensen, MLS2. P3078 - Clinical Outcomes in Patients With Iron Deficiency Anemia After a Severe Gastrointestinal Hemorrhage From Different Types of Gastrointestinal Lesions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2VA Greater Los Angeles Healthcare System, Los Angeles, CA
Introduction: Iron deficiency anemia (IDA) is often underrecognized in patients after a severe gastrointestinal (GI) hemorrhage (GIH). For patients with severe GIH, our aims were to compare rates of diagnosis and treatment of IDA and clinical outcomes of 3 subgroups of GIH: portal hypertension (PH) lesions (varices and PH gastropathy), acute on chronic anemia (ACA) from angioma syndromes, or IDA with acute GIH from focal lesions with arteries.
Methods: This is a retrospective analysis of prospectively collected data of patients hospitalized with severe GIH. Severe GIH was defined as acute GIH with drop of Hb ≥ 2g/dL or 1 unit of packed red blood cell transfusion. IDA was defined as serum iron < 50 mcg/dL, ferritin < 30 ng/mL, and transferrin saturation < 20%. Bivariate and multivariate analyses were used to compare clinical characteristics and outcomes. P-value < 0.05 was statistically significant.
Results: Table 1 lists the number and types of UGI and colon lesions by subgroups. There were significant differences in age, gender, race. Cardiovascular diseases (CVD) were significantly more prevalent in the ACA group and liver diseases more common in the variceal/PHG group. Rates of testing for IDA ranged from 42% to 59% - Table 2. For those tested, documented IDA prevalence was high, ranging from 72.2% to 84.6%. There were significant differences in the rates of iron treatment in the 3 groups: 59% in ACA, 36% in acute severe GIH, and 19% in variceal/PHG group – Table 2. For adjusted analysis using the acute severe GIH as reference group, the odds of iron treatment were lower in the variceal/PHG group (OR 0.25, p=0.001) but higher in the ACA group (OR 2.44, p=0.046). As shown in Table 2, both the number of severe clinical outcomes and the composite outcome score were significantly lower in the acute severe GIH group indicating better results than the other two subgroups.
Discussion: 1) 84.6% of patients with ACA had IDA and most received iron treatment but still had poor outcomes, 2) Patients with varices/PHG hemorrhage had the lowest rates of iron testing and treatment. 3) 51% of patients with acute severe GIH were tested for and 72.2% had IDA, 36% received iron, and they had the best clinical outcomes. 4) Further interventional studies should focus on diagnosis of IDA and treatment of IDA patients with acute severe GIH from focal lesions with arteries because they are most likely to benefit and not the other 2 subgroups.
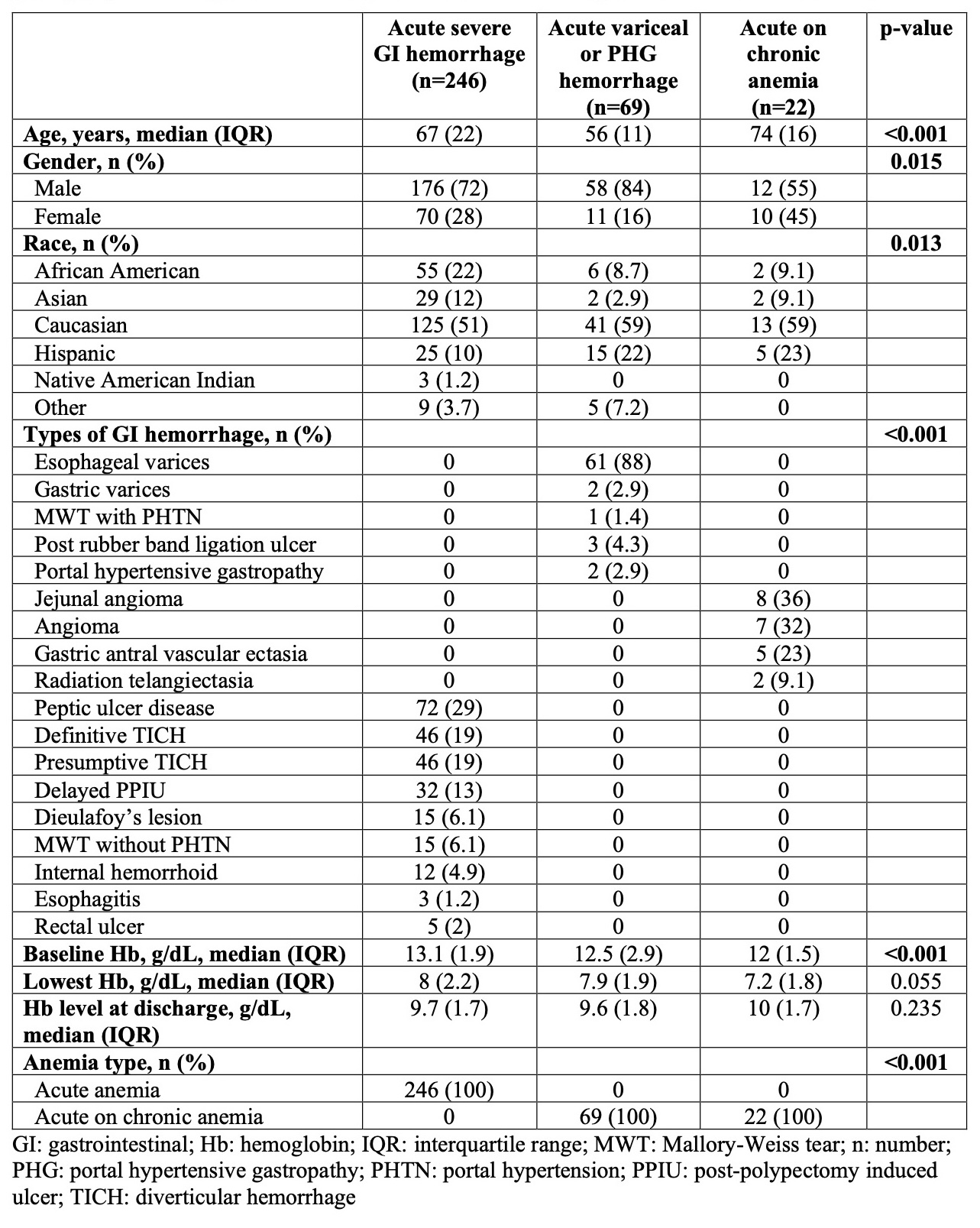
Figure: Table 1. Bivariate comparison of baseline characteristics of acute variceal or portal hypertensive gastropathy hemorrhage, acute severe gastrointestinal hemorrhage, or acute on chronic anemia
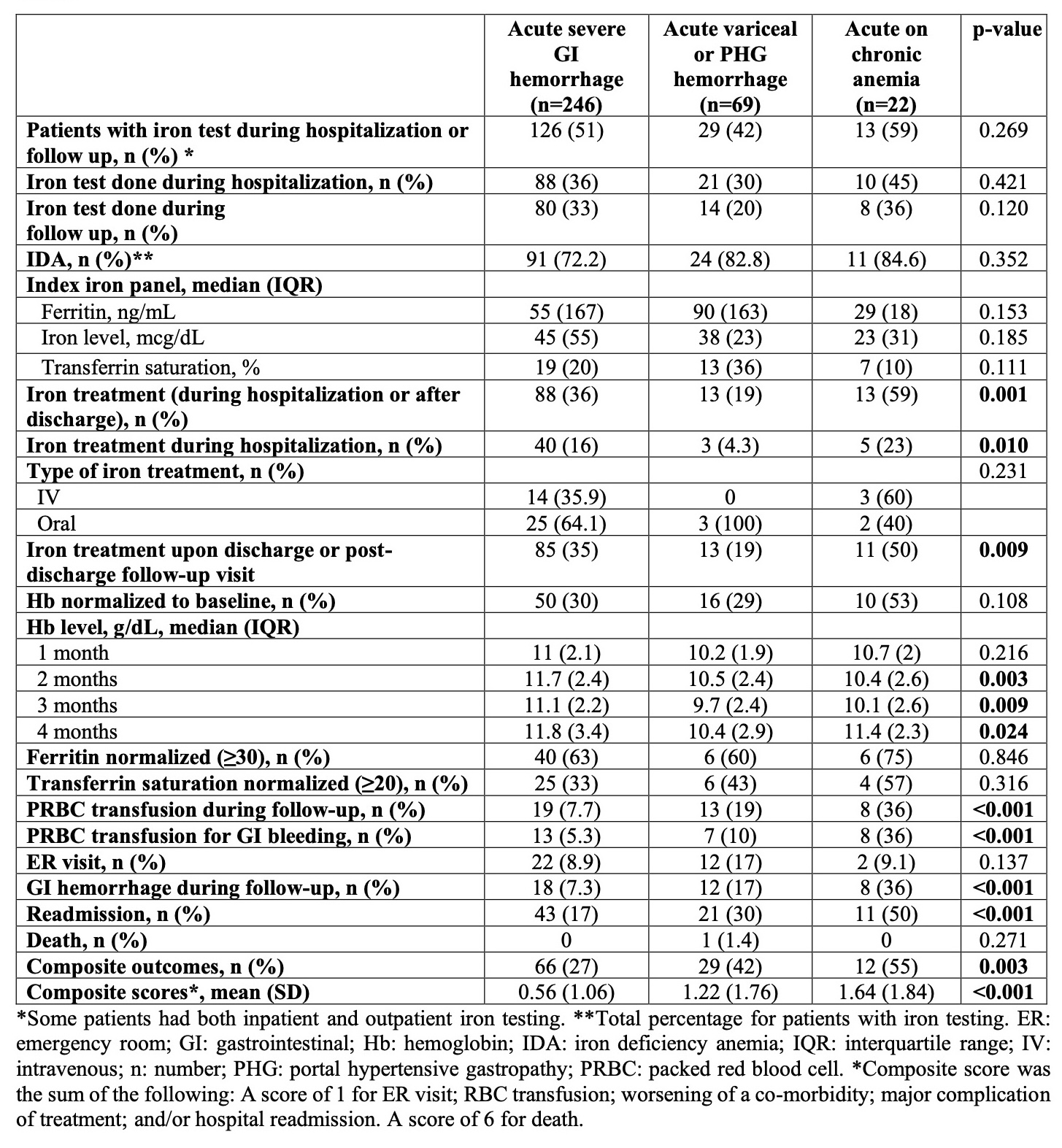
Figure: Table 2. Bivariate comparison of diagnosis and treatment of iron deficiency anemia and clinical outcomes of acute variceal or portal hypertensive gastropathy hemorrhage, acute severe gastrointestinal hemorrhage, or acute on chronic anemia
Disclosures:
Peerapol Wangrattanapranee indicated no relevant financial relationships.
Dennis Jensen indicated no relevant financial relationships.
Usah Dutson indicated no relevant financial relationships.
Mary Ellen Jensen indicated no relevant financial relationships.
Peerapol Wangrattanapranee, MD1, Dennis M.. Jensen, MD2, Usah Dutson, MD, MPH2, Mary Ellen Jensen, MLS2. P3078 - Clinical Outcomes in Patients With Iron Deficiency Anemia After a Severe Gastrointestinal Hemorrhage From Different Types of Gastrointestinal Lesions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

