Sunday Poster Session
Category: Esophagus
P0748 - Aneurysmal Achalasia: Unmasking Dysphagia in the Shadow of the Aorta
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ryan Burd, DO (he/him/his)
Southwest Healthcare MEC
Temecula, CA
Presenting Author(s)
Ryan Burd, DO, Ryan Gilbertson, MD, Edwin Choque, MD, John Michael Vincent Coralde, MD, Indraneel Chakrabarty, MD
Southwest Healthcare MEC, Temecula, CA
Introduction: Pseudoachalasia is diagnostically similar to achalasia and is most commonly secondary to local gastro-esophageal malignancy. We present the case of an 83-year-old female who exhibited intermittent dysphagia with solid foods and was ultimately diagnosed with pseudoachalasia secondary to descending thoracic aortic aneurysm. This report highlights the exceedingly rare association between thoracic aneurysm and pseudoachalasia and is the first of its kind to demonstrate concurrent esophageal candidiasis.
Case Description/
Methods: An 83-year-old female with a past medical history of abdominal aortic aneurysm (AAA) and attempted stent repair, COPD, DVT and hypertension presented to the emergency department with malaise, sore throat and mild headaches for 1 day. Upon further questioning, the patient revealed progressive dysphagia to solid foods for 1 year. GI was consulted and EGD with dilation displayed food residue within the stomach and white esophageal plaques confirmed to be candida species on gram stain. Radiographic esophagram noted a high-grade stricture of the distal third of the esophagus with significant retention of contrast. Subsequent CT enterography and angiography revealed a 4.9cm aneurysm of the descending thoracic aorta and 6.5cm x 7.2cm fusiform aneurysm of the infrarenal abdominal aorta. The patient was diagnosed with pseudoachalasia secondary to descending thoracic aortic aneurysm. The patient elected to proceed with hospice given age and comorbidities, ultimately expiring inpatient due to acute onset abdominal pain and hemodynamic instability due to suspected AAA rupture.
Discussion: According to modern meta analyses, thoracic aortic aneurysm is among the rarest etiologies of pseudoachalasia, accounting for < 1% of reported cases. Among the publications documenting this phenomenon, this is the first and only case to report candidiasis as a likely sequela to aneurysmally-derived pseudoachalasia. This case reinforces the criticality of endoscopy in the diagnosis of pseudoachalasia to distinguish invasive neoplasm from external obstructions. While esophageal manometry can be useful in confirming diagnosis, pseudoachalasia cannot be distinguished from achalasia by esophageal manometry alone. Although the presented patient elected against invasive management, the current guideline-directed treatment of pseudoachalasia includes pneumatic dilation and surgical Heller myotomy with fundoplication or peroral endoscopic myotomy (POEM).
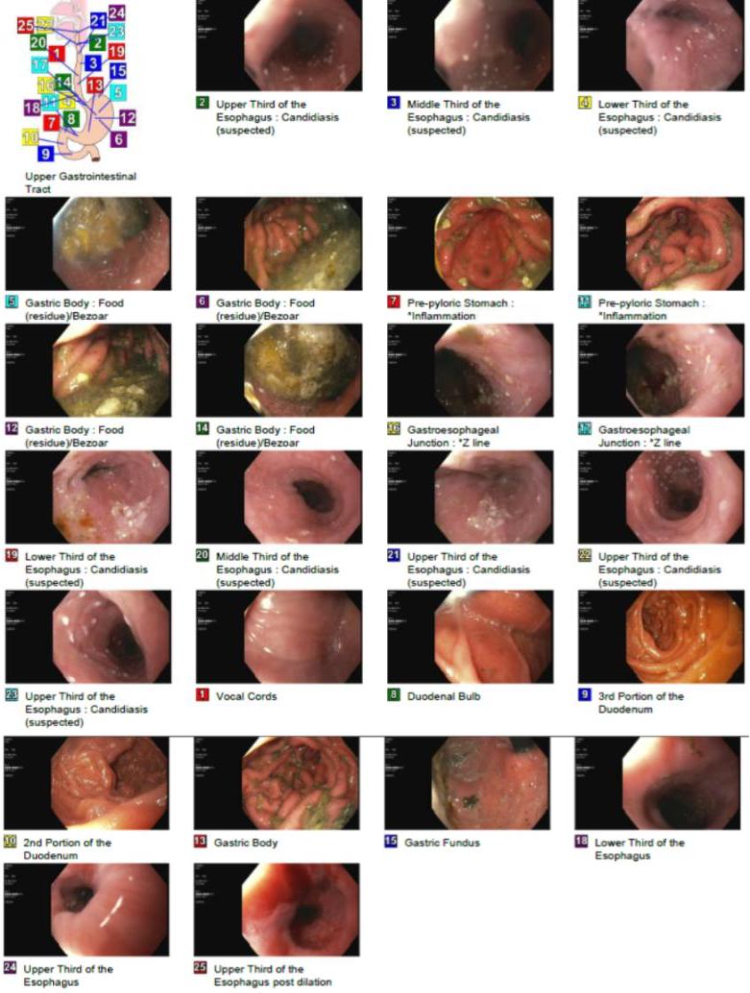
Figure: Esophagogastroduodenoscopy study visualizing candidal plaques across the upper, mid and lower esophagus and food residue within the gastric body, indicating need for further assessment with radiographic esophagram.
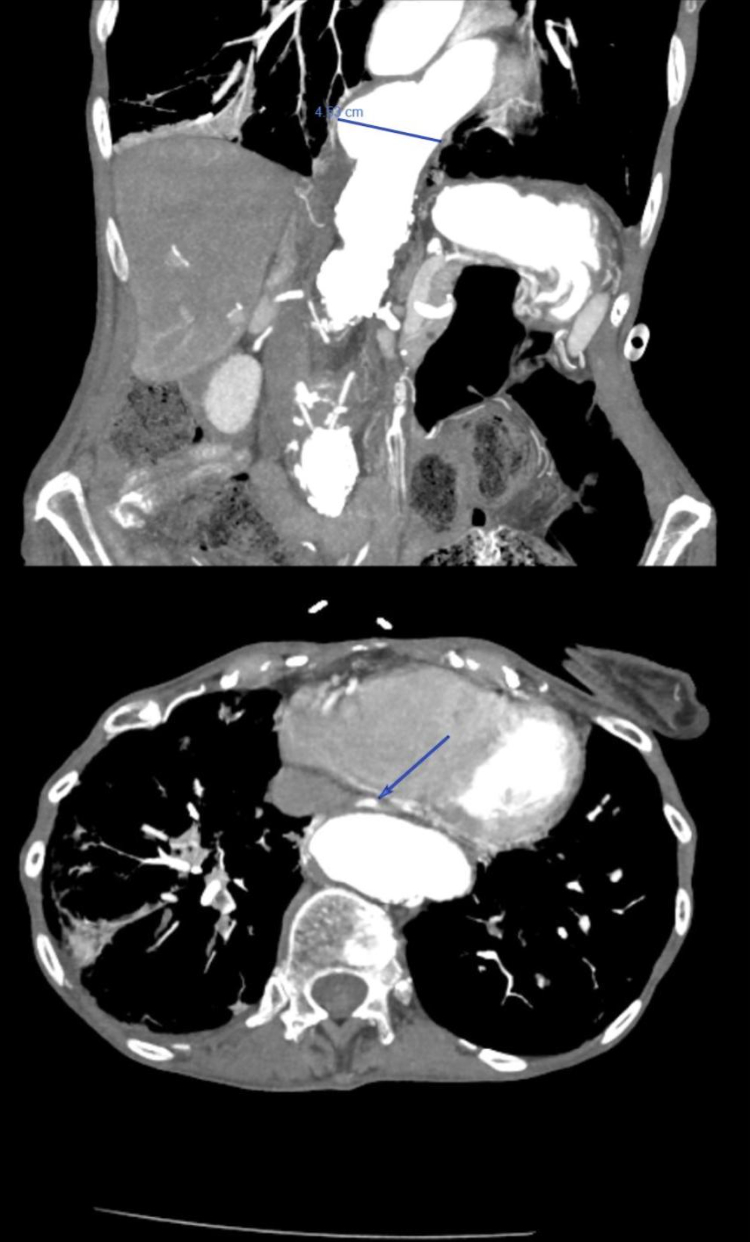
Figure: Coronal CT angiography of abdomen showing descending thoracic aortic aneurysm as marked (top) beneath mid and lower esophagus containing residual enterography contrast, and axial view demonstrating esophageal narrowing as marked (bottom) secondary to posterior thoracic aortic aneurysm.
Disclosures:
Ryan Burd indicated no relevant financial relationships.
Ryan Gilbertson indicated no relevant financial relationships.
Edwin Choque indicated no relevant financial relationships.
John Michael Vincent Coralde indicated no relevant financial relationships.
Indraneel Chakrabarty indicated no relevant financial relationships.
Ryan Burd, DO, Ryan Gilbertson, MD, Edwin Choque, MD, John Michael Vincent Coralde, MD, Indraneel Chakrabarty, MD. P0748 - Aneurysmal Achalasia: Unmasking Dysphagia in the Shadow of the Aorta, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Southwest Healthcare MEC, Temecula, CA
Introduction: Pseudoachalasia is diagnostically similar to achalasia and is most commonly secondary to local gastro-esophageal malignancy. We present the case of an 83-year-old female who exhibited intermittent dysphagia with solid foods and was ultimately diagnosed with pseudoachalasia secondary to descending thoracic aortic aneurysm. This report highlights the exceedingly rare association between thoracic aneurysm and pseudoachalasia and is the first of its kind to demonstrate concurrent esophageal candidiasis.
Case Description/
Methods: An 83-year-old female with a past medical history of abdominal aortic aneurysm (AAA) and attempted stent repair, COPD, DVT and hypertension presented to the emergency department with malaise, sore throat and mild headaches for 1 day. Upon further questioning, the patient revealed progressive dysphagia to solid foods for 1 year. GI was consulted and EGD with dilation displayed food residue within the stomach and white esophageal plaques confirmed to be candida species on gram stain. Radiographic esophagram noted a high-grade stricture of the distal third of the esophagus with significant retention of contrast. Subsequent CT enterography and angiography revealed a 4.9cm aneurysm of the descending thoracic aorta and 6.5cm x 7.2cm fusiform aneurysm of the infrarenal abdominal aorta. The patient was diagnosed with pseudoachalasia secondary to descending thoracic aortic aneurysm. The patient elected to proceed with hospice given age and comorbidities, ultimately expiring inpatient due to acute onset abdominal pain and hemodynamic instability due to suspected AAA rupture.
Discussion: According to modern meta analyses, thoracic aortic aneurysm is among the rarest etiologies of pseudoachalasia, accounting for < 1% of reported cases. Among the publications documenting this phenomenon, this is the first and only case to report candidiasis as a likely sequela to aneurysmally-derived pseudoachalasia. This case reinforces the criticality of endoscopy in the diagnosis of pseudoachalasia to distinguish invasive neoplasm from external obstructions. While esophageal manometry can be useful in confirming diagnosis, pseudoachalasia cannot be distinguished from achalasia by esophageal manometry alone. Although the presented patient elected against invasive management, the current guideline-directed treatment of pseudoachalasia includes pneumatic dilation and surgical Heller myotomy with fundoplication or peroral endoscopic myotomy (POEM).
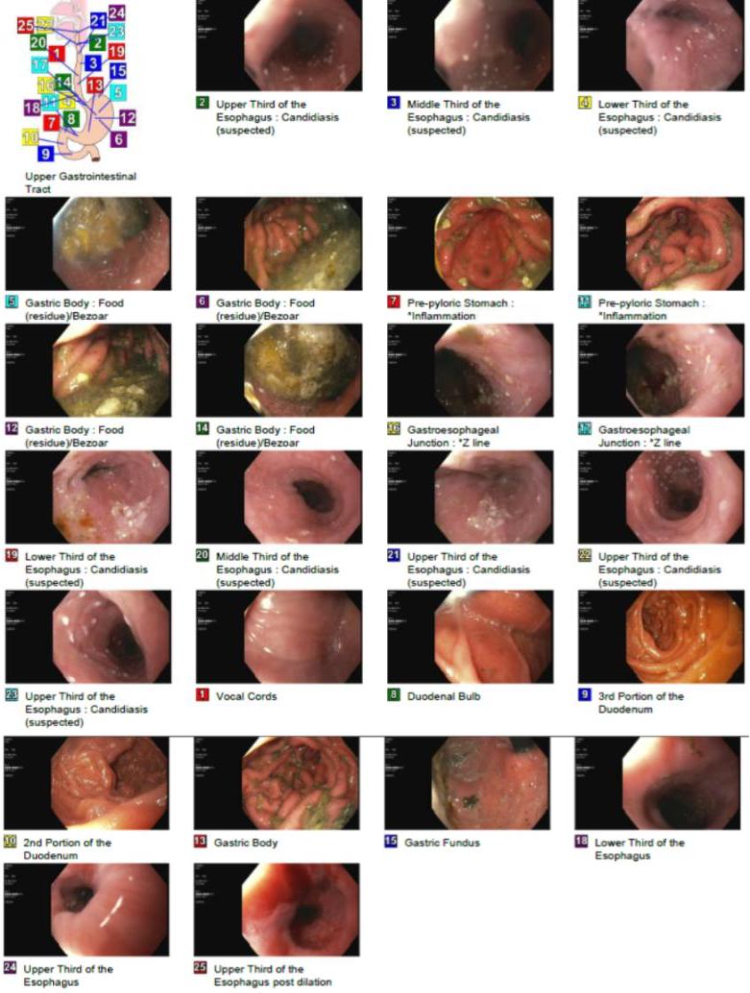
Figure: Esophagogastroduodenoscopy study visualizing candidal plaques across the upper, mid and lower esophagus and food residue within the gastric body, indicating need for further assessment with radiographic esophagram.
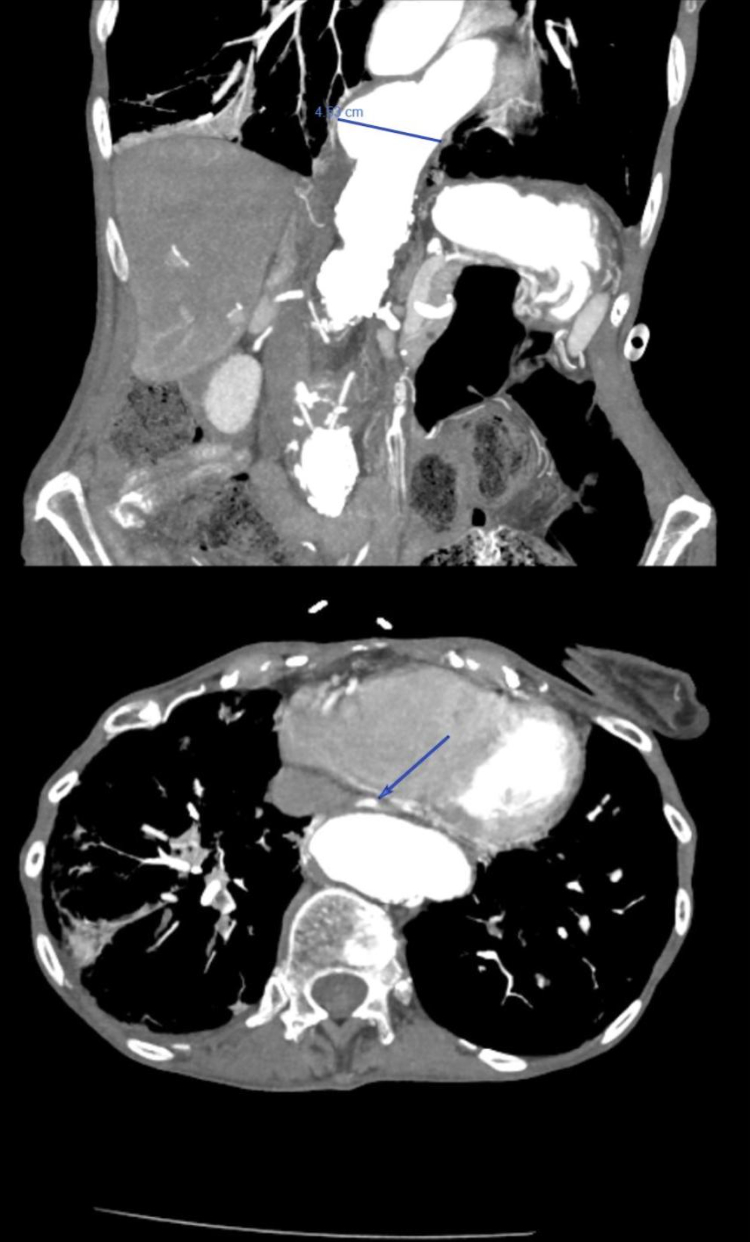
Figure: Coronal CT angiography of abdomen showing descending thoracic aortic aneurysm as marked (top) beneath mid and lower esophagus containing residual enterography contrast, and axial view demonstrating esophageal narrowing as marked (bottom) secondary to posterior thoracic aortic aneurysm.
Disclosures:
Ryan Burd indicated no relevant financial relationships.
Ryan Gilbertson indicated no relevant financial relationships.
Edwin Choque indicated no relevant financial relationships.
John Michael Vincent Coralde indicated no relevant financial relationships.
Indraneel Chakrabarty indicated no relevant financial relationships.
Ryan Burd, DO, Ryan Gilbertson, MD, Edwin Choque, MD, John Michael Vincent Coralde, MD, Indraneel Chakrabarty, MD. P0748 - Aneurysmal Achalasia: Unmasking Dysphagia in the Shadow of the Aorta, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
