Tuesday Poster Session
Category: Interventional Endoscopy
P5757 - Buried Bumper Syndrome: A Rare Complication of Percutaneous Gastrostomy Tube Placement
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JD
Jessica Demes, MD (she/her/hers)
Brooke Army Medical Center
Fort Sam Houston, TX
Presenting Author(s)
Jessica Demes, MD, Luis Velez-Colon, MD
Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Buried bumper syndrome (BBS) is an uncommon serious complication of percutaneous gastrostomy tube (PEG) placement. Over 250,000 PEGs are placed in the United States yearly. BBS occurs in approximately 1% of patients with PEGs. BBS develops as a consequence of excess traction on the external PEG bumper against the abdominal wall. This results in the internal bumper being enveloped by the gastrostomy tract causing swelling of surrounding cutaneous tissues and lodging of the bumper between the gastric wall and the skin. In extreme cases, this can result in an abscess cavity with a fistulous tract, peritonitis, and perforation. Cardinal feature is the inability to advance the tube and difficulty rotating the tube. We present a case of this rare complication requiring advanced endoscopy for removal of the impacted PEG bumper.
Case Description/
Methods: 42 year old non verbal male with a history of traumatic brain injury and ongoing disorder of consciousness after an accident. PEG was placed in Nov 2024. PEG stopped flushing in March 2025. Computed tomography scan showed PEG was partially positioned within the gastric wall. Initial esophagogastroduodenoscopy (EGD) showed overgrown gastric mucosa with central depression and pus draining with manipulation of PEG. EGD was repeated with advanced endoscopy. A wire was placed through the tract and advanced into the stomach. Using a balloon dilator, needle knife, and an electrosurgical knife, the gastric mucosa was dissected until the bumper was visualized. Raptor graspers were used to pull bumper through the gastric mucosa and out. The gastric defect was closed using an endoscopic suturing device. Due to large inflamed defect, no safe endoscopic target was noted for PEG replacement and ultimately surgery replaced PEG.
Discussion: BBS is an uncommon serious complication of PEG tubes. It highlights the importance of patient education in proper PEG care including ensuring appropriate distance between external bolster and the abdominal wall and avoiding gauze pads under the external bolster to avoid excessive traction. When BBS occurs, there is a role for advanced endoscopy in removal of the PEG helping patients to avoid partial gastrectomy. If the internal bumper is within the gastric wall, there are multiple techniques advanced endoscopy could attempt to remove the tube including endoscopic submucosal dissection devices, dilating over a wire, papillotome, and snare techniques. These provide options for treating BBS, helping patients to avoid invasive surgery.

Figure: CT scan sagittal plane showing concern for buried internal PEG bumper
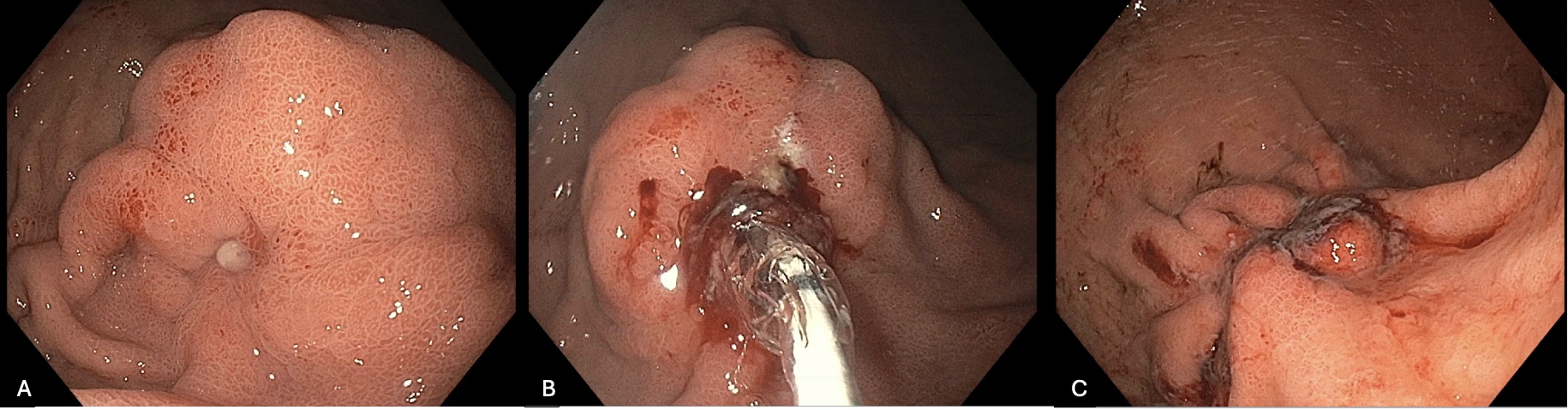
Figure: A. Gastric body with buried PEG bumper and small amount of pus oozing from suspected tract
B. Balloon dilation of PEG tract
C. Closed defect status post removal of buried PEG bumper and closure via endoscopic suturing
Disclosures:
Jessica Demes indicated no relevant financial relationships.
Luis Velez-Colon indicated no relevant financial relationships.
Jessica Demes, MD, Luis Velez-Colon, MD. P5757 - Buried Bumper Syndrome: A Rare Complication of Percutaneous Gastrostomy Tube Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Buried bumper syndrome (BBS) is an uncommon serious complication of percutaneous gastrostomy tube (PEG) placement. Over 250,000 PEGs are placed in the United States yearly. BBS occurs in approximately 1% of patients with PEGs. BBS develops as a consequence of excess traction on the external PEG bumper against the abdominal wall. This results in the internal bumper being enveloped by the gastrostomy tract causing swelling of surrounding cutaneous tissues and lodging of the bumper between the gastric wall and the skin. In extreme cases, this can result in an abscess cavity with a fistulous tract, peritonitis, and perforation. Cardinal feature is the inability to advance the tube and difficulty rotating the tube. We present a case of this rare complication requiring advanced endoscopy for removal of the impacted PEG bumper.
Case Description/
Methods: 42 year old non verbal male with a history of traumatic brain injury and ongoing disorder of consciousness after an accident. PEG was placed in Nov 2024. PEG stopped flushing in March 2025. Computed tomography scan showed PEG was partially positioned within the gastric wall. Initial esophagogastroduodenoscopy (EGD) showed overgrown gastric mucosa with central depression and pus draining with manipulation of PEG. EGD was repeated with advanced endoscopy. A wire was placed through the tract and advanced into the stomach. Using a balloon dilator, needle knife, and an electrosurgical knife, the gastric mucosa was dissected until the bumper was visualized. Raptor graspers were used to pull bumper through the gastric mucosa and out. The gastric defect was closed using an endoscopic suturing device. Due to large inflamed defect, no safe endoscopic target was noted for PEG replacement and ultimately surgery replaced PEG.
Discussion: BBS is an uncommon serious complication of PEG tubes. It highlights the importance of patient education in proper PEG care including ensuring appropriate distance between external bolster and the abdominal wall and avoiding gauze pads under the external bolster to avoid excessive traction. When BBS occurs, there is a role for advanced endoscopy in removal of the PEG helping patients to avoid partial gastrectomy. If the internal bumper is within the gastric wall, there are multiple techniques advanced endoscopy could attempt to remove the tube including endoscopic submucosal dissection devices, dilating over a wire, papillotome, and snare techniques. These provide options for treating BBS, helping patients to avoid invasive surgery.

Figure: CT scan sagittal plane showing concern for buried internal PEG bumper
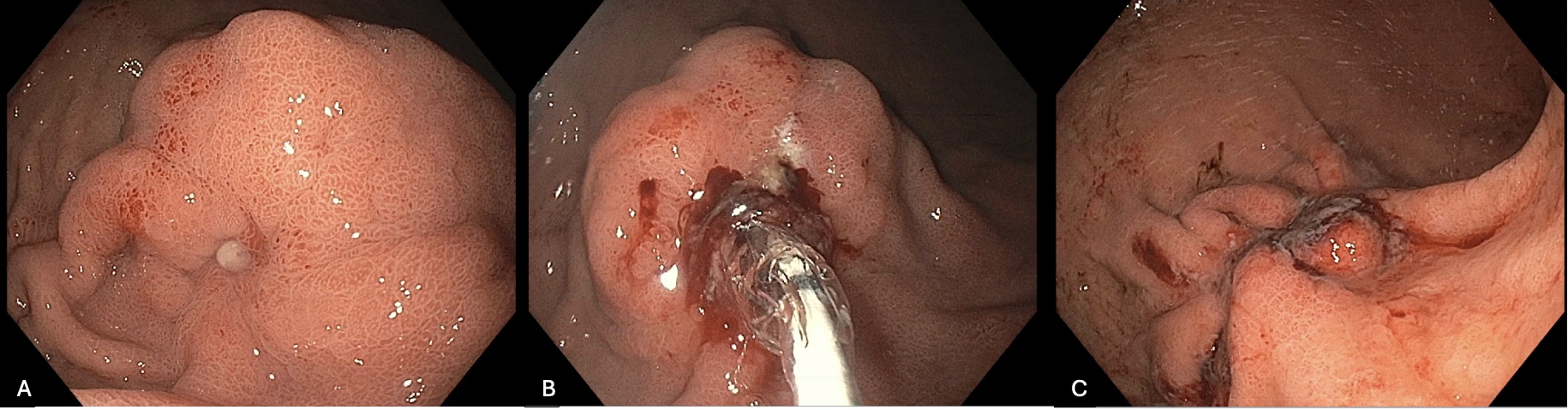
Figure: A. Gastric body with buried PEG bumper and small amount of pus oozing from suspected tract
B. Balloon dilation of PEG tract
C. Closed defect status post removal of buried PEG bumper and closure via endoscopic suturing
Disclosures:
Jessica Demes indicated no relevant financial relationships.
Luis Velez-Colon indicated no relevant financial relationships.
Jessica Demes, MD, Luis Velez-Colon, MD. P5757 - Buried Bumper Syndrome: A Rare Complication of Percutaneous Gastrostomy Tube Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
